![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
21 Cards in this Set
- Front
- Back
|
4 general considerations when regarding consequence to injurious stimuli: |
1. Type of injury 2. Duration 3. Severity/extent/concentration in tissue 4. Type of cell injuried, and its current status |
|
|
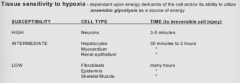
Which tissues are most sensitive to hypoxia? |
|
|
|
Which 5 intracellular systems are most vulnerable to injury? |
1. Cell membrane (around the cell and around organelles) 2. Aerobic respiration (mitochondrial oxidative phosphorylation/ATP production) 3. Protein synthesis (structural and functional proteins) 4. Cytoskeleton 5. Genetic apparatus (DNA) |
|
|
5 biochemical mechanisms of cell injury: |
1. ATP depletion 2. Free radical induced injury (oxidative stress) 3. Intracellular calcium and loss of calcium homeostasis 4. Mitochondrial damage (can be from membrane defects and lead to ATP depletion) 5. Defects in membrane permeability (plasma membrane, lysosome membrane) |
|
|
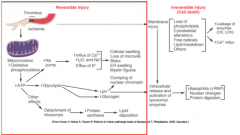
What can cause ATP depletion? How does it affect cells? |
- Common consequence of ischemic and toxic injury - ATP require for membrane transport/osmotic balance, protein synthesis, protein stability (folding), lipogenesis etc |
|
|
Why is oxidative stress bad? What can cause it? |
- Free radicals: molecules with a single unpaired electron - readily react with organic or inorganic chemicals, attack and degrade nucleic acids and membrane molecules - Mechanism of cell damage during disease processes such as chemical, radiation, O2 toxicity, inflammation, reperfusion etc - Injury occurs when free radical generation overwhelms radical-scavenging defense mechanisms |
|
|
What are the 3 main sites of free radical damage? |
1. Membranes (lipid peroxidation) 2. Proteins 3. DNA |
|
|
How does your cell protect itself against free radical damage? |
1. Storage and transport proteins - Proteins bind iron and copper (which catalyze formation of reactive oxygen forms) - IE: ceruloplasmin, transferrin, lactoferrin, apoferritin
2. Antioxidants - Either block the formation of free radicals or inactivate/scavenge them - IE: vitamin A and E (in membranes), vitamin C (in cytosol), glutathione (in cytosol)
3. Enzymes that scavenge free radicals - Glutathione peroxidase - Superoxide dismutase (converts O2- to H2O2) - Catalase (breaks down H2O2 to oxygen and water) |
|
|
How does glutathione act as an antioxidant? |
When in reduced form (GSH), it reacts with H2O2 or OH* to form oxidized glutathione (GSSG) and water.
Glutathione peroxidase catalyzes GSH to GSSG. |
|
|
What is the normal level of free calcium in the cytosol? |
Cytosolic free calcium is LOW - <0.1umol - compared to extracellular Ca2+. This is because of energy dependent pumps and sequestration within the mitochondria and ER. |
|
|
What can cause increases in cytosolic calcium? |
Ischemia and some toxins: cause influx of calcium across the plasma membrane and release of calcium from the ER and mitochondria. |
|
|
What effects does increased cytosolic Ca2+ have on the cell? |
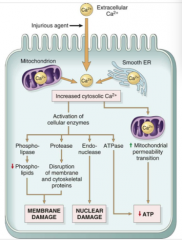
Activation of enzymes that have negative effects: - ATPases = ATP depletion - Phospholipidases = membrane damage - Proteases = breakdown of membrane/skeletal proteins - Endonucleases = DNA/chromatin damage |
|
|
How does mitochondrial damage affect cells? How do they get damaged? |
All cells depend on oxidative metabolism for long term survival, so mitochondrial damage will eventually kill cells.
Mitochondria damage can happen: - Directly: via certain toxins (ie cyanide) - Indirectly: via increased cytosolic calcium, free radicals, phospholipidases etc |
|
|
How does damage to membranes occur? |
- Directly by free radicals, physical agents, chemical agents, bacterial toxins, viruses, lytic complement components - Indirect damage from ATP depletion, calcium activation of phospholipidases, proteases (producing damage to cytoskeletons)
- Lyosomal membrane damage will cause leakage of enzymes that self digest. |
|
|
What is the main type of reversible cell injury? |
- Hydropic degeneration aka acute cell swelling: an early, sublethal manifestation of cell damage, characterized by increased cell size and volume. - Recognized by light microscopy |
|
|
What is the pathogenesis of acute cell swelling? |
- Overload of intracellular water due to electrolyte transport alterations across plasma membranes and ER - Failure of osmotic homeostasis: diffuse disintegration of organelles and cytoplasmic proteins |
|
|
Etiology of acute cell swelling - what can cause it? |
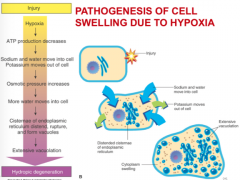
Anything capable of disrupting cellular homeostasis: - Physical injury - Hypoxia - Toxins - Free radicals - Viruses - Bacteria - Immune mediated injury |
|
|
What is the gross appearance of acute cell swelling? |
- Organ swollen with round edges - Paler than normal - Cut surfaces bulge - Heavier than normal |
|
|
What is the histological appearance of acute cell swelling? |
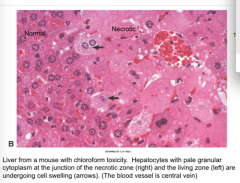
- Water dilutes cytoplasm (=pale) - Cells appear larger - Nucleus often in normal position |
|
|
What are the three degrees of microscopic changes in acute cell swelling? |
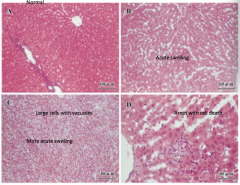
1. Cloudy swelling: cells are pale and slightly granular (mildest)
2. Hydropic/vacuolar degeneration: cells swollen with many vacuoles in the cytoplasm
3. Ballooning degeneration: cells enlarge and rupture. Often seen in viral diseases. (most severe) |
|
|
What are the ultrastructural changes that occur due to acute cell swelling? |
Plasma membrane: microvilli loss, blebbing, myelin figures, intercellular attachments loosen
Endoplasmic reticulum: cisternae dilation/fluid accumulation, polysome detachment/disintegration
Mitochondria: swelling, appearance of small densities
Nucleus: chromatin clumping, granular/fibrillar component disintegration |

