![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back
|
Case: 32 yo female sustained a right ankle fracture, 1 week after the cast was applied she developed some right leg pain. The next day she had shortness of breath, anterior chest discomfort, palpitations, and mild hemoptysis.
What is most likely responsible for her symptoms? How do you treat this? |
Pulmonary Embolism after DVT:
- Confirmed w/ chest CT w/ pulmonary angio (contrast fo fill in blood vessels) protocol - Bilateral lower lobe filling defects consistent w/ acute PE * Give her heparin followed by coumadin for 3 months |
|
|
What should you do for a patient who has acute PE?
|
- Heparin
- Coumadin for 3 months |
|
|
How do you diagnose Pulmonary Embolism?
|
Chest CT w/ pulmonary angio (contrast fo fill in blood vessels) protocol
|
|
|
What is the prognosis for Pulmonary Embolism?
|
- Often fatal
- But many causes are preventable |
|
|
What are the risk factors for Pulmonary Embolism?
|
- Thrombophilias (hyper-coagulable states)
- Can be a genetic defect that predisposes them to clotting - Other conditions independent of genetics (Virchow's Triad and other medical risks) |
|
|
What are the thrombophilias that can make you at increased risk for Venous Thromboembolism?
|
Abnormal tendency to develop blood clots:
- Protein C, S - ATIII - Factor V Leiden - Prothrombin gene mutation - MTHFR - Factor VIII |
|
|
What is Virchow's Triad?
|
- Stasis
- Injury - Hyper-coagulability *Main risk factors for Venous Thromboembolism |
|
|
What are the medical risks for Venous Thromboembolism?
|
- Hip, knee surgery
- Immobility - CHF, obesity - Malignancy (may be cause of idiopathic VTE) - Acquired hyper-coagulability |
|
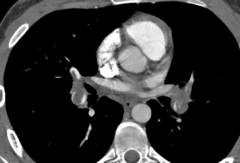
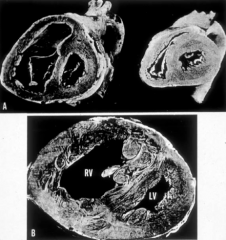
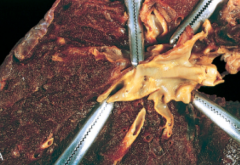
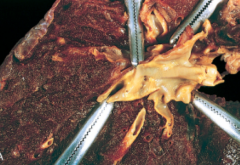
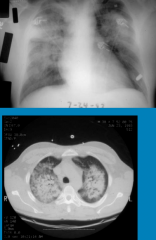
What is shown here?
|
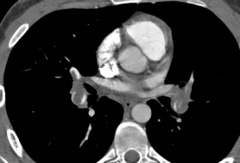
Saddle Embolus
- White opaque material should be filing up blood vessels - Black material in pulmonary vessel is a blockage |
|
|
Where do most Pulmonary Embolisms originate?
|
60-90% originate in proximal deep veins of the legs
|
|
|
What is the mortality risk for PE if untreated? if treated in hospital?
|
- Untreated: 30% mortality
- In-hospital: 2.5% (vast majority resolve w/ treatment) |
|
|
What percent of acute PE becomes chronic PE? Risk factor?
|
- 1-3% become chronic PE
- Main risk factor: recurrent events |
|
|
Why do people die in the hospital after PE?
|
- Recurrent, acute PE
- Massive obstruction of vessels - RV failure, infarct |
|
|
What are the symptoms of PE? Why is it hard to diagnose PE based on symptoms?
|
Symptoms are rather non-specific so easy to miss:
- Dyspnea (acute or subacute) - Dizziness or syncope (often w/ large PE, massive, "saddle") - Chest pain is "pleuritic" (d/t infarct, bloody effusion) - Palpitations and tachycardia - Hemoptysis (infarct) |
|
|
If a pulmonary infarct occurs, where is it most likely to occur after PE?
|
Distal .....
|
|
|
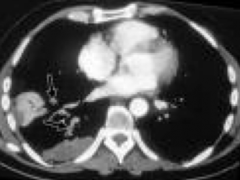
What tool can be used to workup Pulmonary Hypertension?
|
Ventilation perfusion lung scan
- This lung scan has a high sensitivity (90-100%) and specificity (94-100%) for distinguishing between IPAH and CTEPH |
|
|
Why is a ventilation perfusion lung scan an important component of the workup for pulmonary hypertension?
|
To exclude CTEPH, a potentially curable cause of PH
|
|
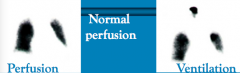
What do these images show?
|
Shows homogenous uptake of radio tracer in the lungs with both perfusion and ventilation, typical in patients with IPAH (idiopathic pulmonary artery hypertension)
|
|
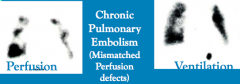
What do these images show?
|
Shows a matched ventilation and perfusion defect in the right mid-lung, but several defects on perfusion imaging that are not matched with defects on ventilation (ie, unmatched perfusion defects), findings that are highly suspicious for *chronic pulmonary embolic disease*
|
|
|
What happens in thromboembolic obstruction of proximal pulmonary arteries?
|
- Surgical candidates, need to be on chronic anti-coagulation post-surgery too to prevent this from happening again
- Obstruction of distal pulmonary arteries too |
|
|
What are the classifications of pulmonary hypertension?
|
- I: pulmonary arterial HTN
- II: pulmonary venous HTN, left heart failure (most common) - III: pulmonary HTN w/ respiratory disorder (FVC < 70%) - IV: pulmonary HTN w/ thromboembolic disorder - V: miscellaneous pulmonary HTN |
|
|
What is the most common type of Pulmonary HTN?
|
Group II - Pulmonary HTN d/t Left Heart failure:
- L heart backs up fluid into the pulmonary vasculature |
|
|
What is Pulmonary HTN group 1?
|
Pulmonary Arterial HTN:
- Mean pulmonary arterial pressure (mPAP) > 25 mmHg at rest - Normal wedge pressure (PCWP) |
|
|
What is Pulmonary HTN group 2?
|
Pulmonary Venous HTN d/t Left Heart Failure (passive process)
|
|
|
What is Pulmonary HTN group 3?
|
Pulmonary HTN w/ respiratory disorder (FVC < 70%)
|
|
|
What is Pulmonary HTN group 4?
|
Pulmonary HTN w/ chronic Thromboembolic Disorders
|
|
|
What is Pulmonary HTN group 5?
|
Miscellaneous causes of Pulmonary HTN (eg, sarcoidosis)
|
|
|
What is the best, non-invasive test for assessing Pulmonary HTN?
|
Echocardiogram
|
|
|
What are the etiologies of Pulmonary HTN?
|
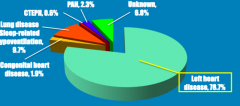
- Left heart disease (79%)
- Lung disease, sleep related hypoventilation (10%) - Unknown (7%) - PAH (2%) - Congenital heart disease (2%) - CTEPH (0.6%) |
|
|
What are the associated adverse changes in Group 1 Pulmonary Artery HTN?
|
Vasculopathy in pulmonary vasculature at level of RV
|
|
|
How do you diagnose Pulmonary HTN?
|
Best w/ Echo:
- RA and RV changes (hypertrophy) - RV overload - Estimate PA pressure |
|
|
What is the prognosis of Pulmonary Arterial HTN (group 1)?
|
Fatal if untreated
|
|
|
What happens to the heart with Pulmonary HTN?
|
Decreased RV function
|
|
|
What are the causes of Group 1 Pulmonary Arterial HTN (PAH)?
|
- Idiopathic (IPAH)
- Heritable (BMPR2 genetic mutation) - Persistent fetal circulation |
|
|
What is Group 1 Pulmonary Arterial HTN (PAH) associated with?
|
APAH (Associated Pulmonary Artery HTN):
- Collagen Vascular Disease (Scleroderma, SLE, RA) - Congenital Heart Disease - Portal HTN - HIV - Drugs - Other |
|
|
What is the genetic cause of Group 1 Pulmonary Arterial HTN (PAH)? How common?
|
- 10% of PAH is familial, heritable
- Mapped to long arm chromosome 2: BMPR2 - BMPR2 = Bone Morphogenic Protein Receptor-2 - Autosomal dominant but low penetrance (only 20% w/ gene get disease) |
|
|
What are the classes / degrees of Group 1 Pulmonary Arterial HTN (PAH)?
|
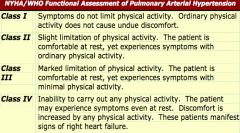
- Class I: sx do not limit physical activity, does not cause undue discomfort
- Class II: slight limitation of physical activity, comfortable at rest - Class III: marked limitation of physical activity, comfortable at rest - Class IV: inability to carry out any physical activity, may experience some sx at rest; manifest signs of RHF |
|
|
What are the symptoms of Pulmonary HTN?
|
* Breathlessness
- Fatigue - Near syncope, syncope (particularly w/ exertion in young adult) - Chest pain: angina - Palpitations |
|
|
If a young patient passes out with exertion what should you think of?
|
Pulmonary HTN
|
|
|
How does the class of Group 1 Pulmonary Arterial HTN (PAH) affect your prognosis?
|
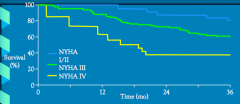
At 36 months:
- Class I/II: 80% survival - Class III: 60% survival - Class IV: 40% survival |
|
|
What happens to pulmonary arteries in Group 1 Pulmonary Arterial HTN (PAH)?
|
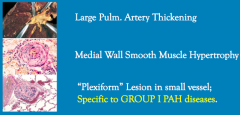
- Large PA thickening
- Medial wall smooth muscle hypertrophy - Plexiform lesion in small vessel |
|
|
What type of Pulmonary HTN are "plexiform" lesions in small vessels specific to?
|
Group 1 Pulmonary Arterial HTN (PAH)
|
|
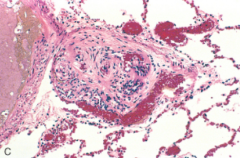
What does this image show?
|
Large PA thickening in Group 1 Pulmonary Arterial HTN (PAH)
|
|
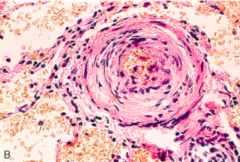
What does this image show?
|
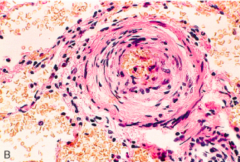
Medial wall smooth muscle hypertrophy in Group 1 Pulmonary Arterial HTN (PAH)
|
|
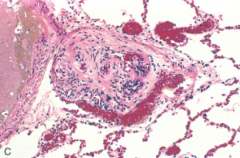
What does this image show?
|
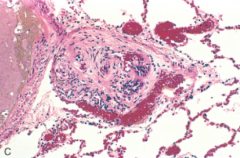
Plexiform lesion in small vessel in Group 1 Pulmonary Arterial HTN (PAH)
|
|
|
What causes endothelial cell defects in Pulmonary HTN?
|
- ↓ Prostacyclin
- ↑ Endothelin - ↓ Nitric Oxide Synthase |
|
|
How can you treat the endothelial cell defects in Pulmonary HTN?
|
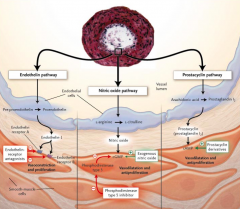
- Endothelin-Receptor Antagonists (because there is ↑ Endothelin)
- Phosphodiesterase type 5 inhibitor (this ↑cGMP allowing vasodilation and anti-proliferation) - Endogenous Nitric Oxide (this ↑cGMP allowing vasodilation and anti-proliferation) - Prostacyclin derivatives (because ↓ Prostacyclin) |
|
|
What drugs are used for Pulmonary Arterial HTN?
|
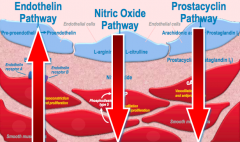
- IV Prostacyclin (Epoprostenol, Flolan)
- Bosentan (Endothelin Receptor Antagonist) - Sildenafil (NO Pathway, ↑cGMP) - Riociguat (NO Pathway, soluble GC stimulator, ↑cGMP) |
|
What does this image show?
|
Pulmonary Vasculitis
|
|
|
What is the pulmonary presentation of Pulmonary Vasculitis?
|
Pulmonary and Alveolar hemorrhage (eg, Goodpasture's Syndrome)
Lung Infiltrates: - Nodular - Cavitary lesions - Associated Interstitial Lung Disease - Acute, bilateral, diffuse Pulmonary HTN |
|
|
What are the classifications of Alveolar (Capillary) Hemorrhage Syndromes?
|
- Antibasement Membrane Antibody Disease (ABMAb) (Goodpasture’s Syndrome)
- Anti Neutrophil Cytoplasmic Antibody (ANCA) Associated Vasculitis (Wegener’s) - Idiopathic Pulmonary Hemosiderosis - Collagen Vascular Diseases (eg, Systemic Lupus Erythematosis =SLE) |
|
|
What is the classic triad in Alveolar (Capillary) Hemorrhage Syndromes?
|
- Hemoptysis
- Pulmonary infiltrates - Anemia |
|
|
What are the life-threatening complications with Alveolar (Capillary) Hemorrhage Syndromes?
|
- Respiratory failure
- Acute renal failure - Severe anemia |
|
|
How do you diagnose Alveolar (Capillary) Hemorrhage Syndromes?
|
- Sputum, tracheal aspirate
- Urine (check for other organ problems) - Serial Hgb: -2 gm in 24 hrs - Serial chest x-rays - Serologies: ABMAb, ANCA, ANA, etc - Bronchoalveolar lavage, open lung biopsy - Biopsies of other organs: skin, renal |
|
|
What are you looking for on Bronchoalveolar Lavage (BAL) / open biopsy in Alveolar (Capillary) Hemorrhage Syndromes?
|
"Siderophages" - hemosideran laden macrophages (these occur after 48 hours of bleeding)
|
|
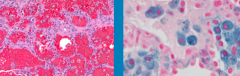
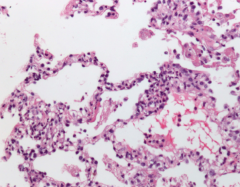
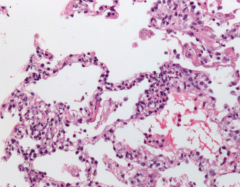
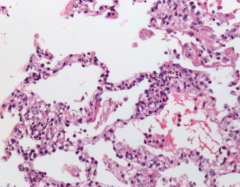
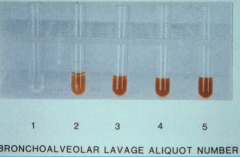
What do these images show?
|
Siderophages - hemosideran laden macrophages in Alveolar (Capillary) Hemorrhage Syndrome
(samples taken via bronchoalveolar lavage (BAL), open biopsy) |
|
Case: 38 yo male presents w/ weeks of coughing. Failed Abx x2, blood streaks in sputum. Otitis media (t tube), rhinitis, fever, tachypnea, tachycardic, crackles, red papules on legs, anemia, ESR 104, c-ANCA, ABMAb skin biopsy.
Diagnosis? Treamtent? |
Wegener's Vaculitis
Tx: pulse methylprednisolone, long-term tx: prednisone and cyclophosphamide |
|
|
What is Wegener's Granulomatosis? Where does it affect?
|
Systemic Vasculitis - granulomatous inflammation
- Affects upper (73%) before lower (45%) respiratory tract - Affects kidney (18%) |
|
|
What are the signs/symptoms of Wegener's Vasculitis?
|
- Upper respiratory tract (80%): Nasal, sinus, otitis
- Dyspnea, obstructive PFT (55%) - Infiltrates, cough, hemoptysis (45%) - Constitutional symptoms (joints/arthralgias (45%), fever) prominent - Skin (40%) - Neuro (40%) - Increased risk for DVT |
|
|
When is Wegener's Vasculitis most common?
|
- 5th decade
- Males > females |
|
|
What are the diagnostic studies for Wegener's Vasculitis?
|
- Tissue biopsy
- Serologies (c-ANCA) |
|
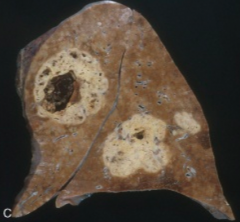
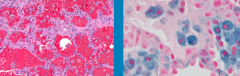
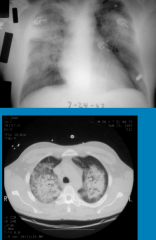
What is this image of?
|
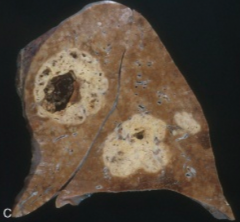
Wegener's Vasculitis:
- Perivascular, necrotizing granulomatous inflammation - Lung necrosis and cavitation - Hemorrhage |

