![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
90 Cards in this Set
- Front
- Back
|
What are the methods of antibiotic treatment?
|
- Empiric
- Directed |
|
|
What does "empiric" antibiotic treatment mean?
|
- Initiation of treatment prior to determination of a firm diagnosis
- Typically broad-spectrum - Should be chosen based on the likely pathogen / diagnosis, patient exposure history, and patient allergy history |
|
|
What does "directed" antibiotic treatment mean?
|
- Treatment based on culture and susceptibility results
- Use the most clinically effective, least toxic, narrowest spectrum, and most cost effective agent - AKA Drug of Choice - Drug, dose, route, interval, and duration is disease state and patient specific |
|
|
How do you interpret the MIC?
|
Minimum Inhibitory Concentration:
- Either S (susceptible), I (intermediate), or R (resistant) - Bug-drug specific (relative to concentrations of drug in body) |
|
|
Is it better to have a lower or higher MIC?
|
Lower Minimum Inhibitory Concentration is better, BUT you can't just pick an antibiotic with the lowest MIC
|
|
|
What are the drugs of choice for invasive MSSA infections?
|
- Nafcillin (Oxacillin)
- Cefazolin |
|
|
What are the common undesired implications of antibiotic therapy?
|
- Antibiotic resistance
- Adverse drug events (ADEs) - Increased health-care costs |
|
|
What are some Adverse Drug Events (ADEs) for antibiotics?
|
- Hypersenstivity / allergy (78% of ED visits d/t Abx)
- Drug side effects (19% of ED visits d/t Abx) - Clostridium difficile infection - Antibiotic associated diarrhea / colitis |
|
|
How often are Adverse Drug Events d/t antibiotics?
|
19.3% of drug adverse events are d/t antibiotics
|
|
|
What kind of antibiotics have the most Adverse Drug Effects?
|
50% d/t Penicillin and Cephalosporin classes
|
|
|
What factors should be considered when selecting an antibiotic?
|
1. Spectrum of coverage
2. Patterns of resistance (at hospital, city, etc) 3. Evidence or track record for specified infection 4. Achievable serum, tissue, or body fluid concentration (eg, CSF or urine) 5. Allergy 6. Toxicity 7. Formulation (IV vs PO); if PO assess bioavailability 8. Adherence / convenience (eg, 2x/day vs 6x/day) 9. Cost |
|
|
What is important to consider before giving a patient an antibiotic besides that which is directly related to the present illness?
|
- Duration of hospitalization, if any
- Co-morbidities - Prior antibiotic use - What are the patterns of resistance in your institution |
|
|
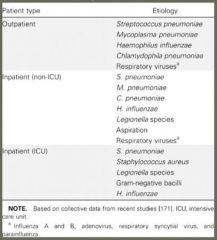
What are the most common etiologies of community acquired pneumonia in out-patient setting? (* those that are specific to this patient type)
|

- Streptococcus pneumoniae
- Mycoplasma pneumoniae - Haemophilus influenzae - Chlamydophila pneumoniae - Respiratory viruses (influenza A and B, adenovirus, RSV, parainfluenza) |
|
|
What are the most common etiologies of community acquired pneumonia in in-patient (non-ICU) setting? (* those that are specific to this patient type)
|

- Streptococcus pneumoniae
- Mycoplasma pneumoniae - Chlamydophila pneumoniae - Haemophilus influenzae - Legionella species * Aspiration - Respiratory viruses (influenza A and B, adenovirus, RSV, parainfluenza) |
|
|
What are the most common etiologies of community acquired pneumonia in in-patient (ICU) setting? (* those that are specific to this patient type)
|

- Streptococcus pneumoniae
* Staphylococcus aureus - Legionella species * Gram-negative bacilli - Haemophilus influenzae |
|
|
What are the types of "atypical pneumonias"?
|
- Chlamydophila pneumoniae (non-ICU and outpatient)
- Mycoplasma pneumoniae (non-ICU and outpatient) - Legionella species (in-patient only) |
|
|
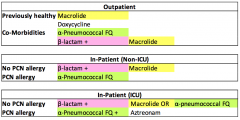
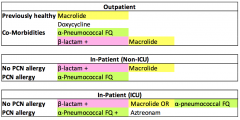
How should you treat a previously healthy patient with Community-Acquired Pneumonia as an out-patient?
|
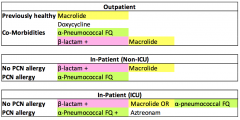
- Macrolide: Azithromycin, Clarithromycin, Erythromycin
- Doxycycline (if macrolide is contraindicated) |
|
|
How should you treat a patient with co-morbidities (uncontrolled COPD, diabetes, heart disease, etc) and Community-Acquired Pneumonia as an out-patient?
|
- α-Pneumococcal Fluoroquinolone: Moxifloxacin, Levofloxacin
- β-lactam + Macrolide (Azithromycin, Clarithromycin) |
|
|
How should you treat a patient without PCN allergy and Community-Acquired Pneumonia as an in-patient (non-ICU)?
|
β-lactam + Macrolide (Azithromycin, Clarithromycin)
|
|
|
How should you treat a patient with a PCN allergy and Community-Acquired Pneumonia as an in-patient (non-ICU)?
|
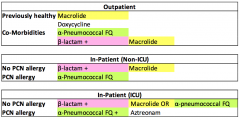
α-Pneumococcal Fluoroquinolone: Moxifloxacin, Levofloxacin
|
|
|
How should you treat a patient without PCN allergy and Community-Acquired Pneumonia as an in-patient (ICU)?
|
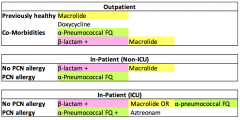
β-lactam
AND Macrolide (Azithromycin, Clarithromycin) OR α-Pneumococcal Fluoroquinolone (Moxifloxacin, Levofloxacin) |
|
|
How should you treat a patient with a PCN allergy and Community-Acquired Pneumonia as an in-patient (ICU)?
|
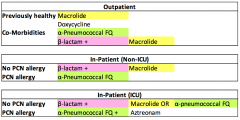
α-Pneumococcal Fluoroquinolone (Moxifloxacin, Levofloxacin)
AND Aztreonam (for G- coverage) |
|
|
How should you treat a patient with Community-Acquired Pneumonia if Pseudomonas is a consideration as an in-patient?
|
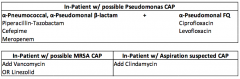
α-Pneumococcal, α-Pseudomonal β-lactam:
- Piperacillin-Tazobactam OR - Cefepime OR - Meropenem AND α-Pseudomonal Fluoroquinolone: - Ciprofloxacin OR - Levofloxacin |
|
|
What are the α-Pneumococcal, α-Pseudomonal β-lactams? When are they indicated?
|
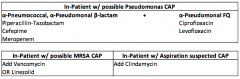
- Piperacillin-Tazobactam
- Cefepime - Meropenem Used for Community-Acquired Pneumonia if Pseudomonas is a consideration as an in-patient |
|
|
What are the α-Pneumococcal Fluoroquinolones?
|
- Moxifloxacin
- Levofloxacin |
|
|
What are the α-Pseudomonal Fluoroquinolones?
|
- Ciprofloxacin
- Levofloxacin |
|
|
How should you treat a patient with Community-Acquired Pneumonia if MRSA is suspected as an in-patient?
|
Add Vancomycin or Linezolid to plan
|
|
|
How should you treat a patient with Community-Acquired Pneumonia if aspiration is suspected as an in-patient?
|
Add Clindamycin to cover oral anaerobes (if initial regimen does not cover anaerobes)
|
|
|
In patients treated for Community-Acquired Pneumonia, how often is Pneumonia not actually present?
|
30% of patients
|
|
|
If a patient has an abnormal chest x-ray, what other evidence do you need before you treat suspected Community-Acquired Pneumonia with antibiotics?
|
Systemic evidence of inflammation:
- Fever - WBC - Sputum production - Etc |
|
|
What should you do if what you thought was pneumonia turns out to be an alternative diagnosis?
|
Discontinue antibiotics
|
|
|
What are the types of β-lactams?
|
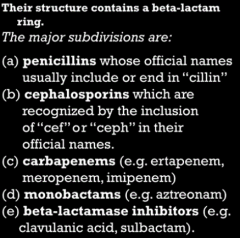
- Penicillins
- Cephalosporins - Carbapenems - Monobactams - β-Lactamases |
|
|
What are the types of Carbapenems? What kind of antibiotic are they?
|
- Ertapenem
- Meropenem - imipenem - β-lactam antibiotics |
|
|
What are the types of Monobactams? What kind of antibiotic are they?
|
- Aztreonam
- β-lactam antibiotics |
|
|
What are the types of β-lactamases? What kind of antibiotic are they?
|
- Clavulanic Acid
- Sulbactam - β-lactam antibiotics |
|
|
What are the drugs of choice for Pneumococcus infections?
|
- Cefotaxime (kids)
- Ceftriaxone (adults) |
|
|
What are the β-lactam drugs of choice for Pseudomonas aeruginosa infections?
|
- Piperacillin-Tazobactam
- Ceftazadime - Cefepime - Meropenem-Imipenem - Aztreonam (monobactam) |
|
|
What are the types of Macrolides?
|
- Azithromycin (easy, once/day)
- Clarithyromycin (twice/day) - Erythromycin (not used much) |
|
|
What are Macrolides (Azithromycin, Clarithromycin) used for?
|
- Respiratory G+ and G- bacteria
- Intracellular atypical pathogens (mycoplasma, chlamydia, legionella) |
|
|
What are α-Pneumococcal and α-Pseudomonal Fluoroquinolones used for besides what is in their names?
|
Intracellular atypical pathogens (Mycoplasma, Chlamydia, Legionella)
|
|
|
What are the Tetracycline antibiotics?
|
- Tetracycline (not used much, least efficacious)
- Doxycycline (equally effective as mino) - Minocycline (more side effects than doxy, but equally effective) |
|
|
What are the Tetracyclines used for?
|
- Wide range of G+ and G- bacteria found in respiratory tract
- Also cover atypical organisms such as chlamydia, mycoplasma, and legionella |
|
|
What are the drugs used for G+ Resistant bacteria (usually referring to MRSA)?
|
- Vancomycin
- Linezolid - Daptomycin |
|
|
What are the limitations of Vancomycin? What is it indicated for?
|
- Will not cover VRE
- IV formulation only - Covers most other resistant G+ bacteria |
|
|
What are the limitations of Linezolid? What is it indicated for?
|
- Bone marrow suppression and neuropathy w/ prolonged use
- Drug for resistant G+ bacteria (MRSA) |
|
|
What are the limitations of Daptomycin? What is it indicated for?
|
- Not for use in pneumonia because it is bound by surfactant
- Used for Resistant G+ bacterial (outside of lung infections) |
|
|
What is the typical duration of treatment for Community-Acquired Pneumonia? When is the duration longer?
|
- Minimum of 5 days, up to 7 days
- Longer duration if culture is positive for coagulase-positive Staph or Pseudomonas |
|
|
What criteria must the patient meet before stopping therapy for Community-Acquired Pneumonia?
|
- Afebrile for 48-72 hours
- Breathing w/o supplemental oxygen (unless required for pre-existing disease) - No more than one clinical instability factor (HR > 100, RR > 24, SBP ≤ 90) |
|
|
What are the risk factors for Multi-Drug Resistant Organisms (MDROs) in Health Care Associated Pneumonia (HCAP)?
|
- Current hospitalization ≥ 5 days
- Hospitalization in acute care hospital for ≥ 2 days within past 90 days - Resident of nursing home or long-term care facility - Recipient of recent IV antibiotic therapy, chemotherapy, or wound care within past 30 days - Chronic dialysis within 30 days - Family member w/ multi-drug resistant pathogen |
|
|
How should you treat a patient without risk factors for Multi-Drug Resistant Organisms (MDROs) with Health Care Associated Pneumonia (HCAP)?
|
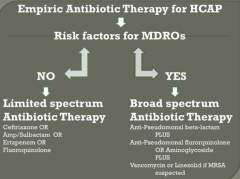
Limited Spectrum Abx Therapy:
- Ceftriaxone OR - Ampicillin-Sulbactam OR - Ertapenem OR - Fluoroquinolone |
|
|
How should you treat a patient with risk factors for Multi-Drug Resistant Organisms (MDROs) with Health Care Associated Pneumonia (HCAP)?
|
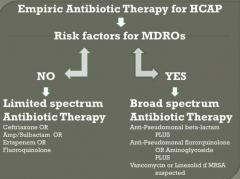
Broad Spectrum Abx Therapy:
α-Pseudomonal β-lactam AND α-Pseudomonal FQ OR Aminoglycoside AND Vancomycin or Linezolid if MRSA suspected |
|
|
What is often responsible for pneumonia in a patient w/ an early HIV infection?
|
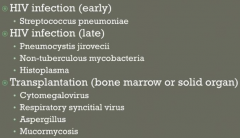
Streptococcus pneumoniae
|
|
|
What is often responsible for pneumonia in a patient w/ a late HIV infection?
|
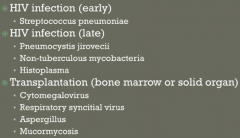
- Pneumocystis jirovecii
- Non-Tuberculous mycobacteria - Histoplasma |
|
|
What is often responsible for pneumonia in a patient w/ a transplantation (bone marrow or solid organ)?
|
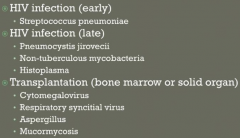
- Cytomegalovirus
- Respiratory syncytial virus - Aspergillus - Mucormycosis |
|
|
What is often responsible for pneumonia in a patient w/ exposure to birds?
|
- Parrots: Chlamydophila psittaci
- Poultry: Avian influenza |
|
|
What is often responsible for pneumonia in a patient w/ exposure to rabbits?
|
Francisella tularensis
|
|
|
What is often responsible for pneumonia in a patient w/ exposure to farm or parturient animals?
|
Coxiella burnetti (Q fever)
|
|
|
What is often responsible for pneumonia in a patient who has recently travelled to SW United States?
|
- Coccidioides
- Hantavirus |
|
|
What is often responsible for pneumonia in a patient w/ structural lung disease (cystic fibrosis, COPD, bronchiectasis)?
|
- Pseudomonas aeruginosa
- Staphylococcus aureus - Non-tuberculous mycobacteria - Aspergillus |
|
|
Case: 49 yo white male w/ hx of HTN and hyperlipidemia presents w/ 3 days of cough, chills, malaise, body aches, and fever to 102.5. He has no known medical allergies.
BP 110/70, T 101.0, RR 26. Crackles at left lung base and CXR reveals corresponding pneumonia. Patient reports that he is unable to sleep because of cough and has never felt as bad as he presently feels. What is the appropriate assessment/treatment of this patient? |
Patient should be treated as an out-patient w/ Azithromycin (Macrolide)
|
|
|
What scale can you use to determine the recommendation for pneumonia treatment / mortality?
|
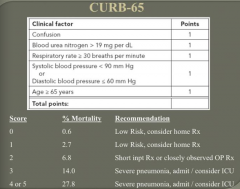
CURB-65:
- Confusion = 1 - BUN > 19 mg/dL = 1 - RR ≥ 30 = 1 - SBP < 90 mmHg or DBP ≤ 60 mmHg = 1 - Age ≥ 65 years = 1 |
|
|
What CURB-65 score is associated with a low-risk pneumonia and can be treated at home?
|
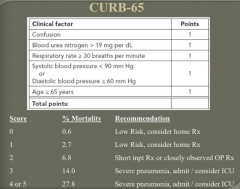
0 or 1
|
|
|
What CURB-65 score is associated with pneumonia that should be treated with a short-inpatient stay or closely observed out-patient?
|
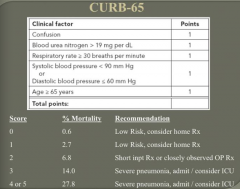
2
|
|
|
What CURB-65 score is associated with severe pneumonia and the patient should be admitted to the ICU?
|
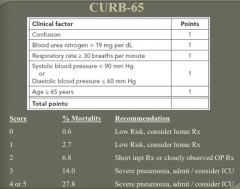
> 3
|
|
|
Case: 77 yo female presents to ED w/ dyspnea, fever, hypoTN, and mental status change. She lives at home and has been in relatively good health until this presentation.
T 103, BP 88/60, P 110, R 34, SaO2 88% on RA, improves to 99% on 4L NC Crackles in left lung base. CXR shows left lower lobe infiltrate. WBC of 2.3, BUN of 33, Creatinine of 1.3. Based on above presentation, what is the most appropriate course of action? |
- Based on CURB-65 score she should be admitted to ICU for severe pneumonia
- Begin fluid resuscitation - IV Ceftriaxone (β-lactam) and Moxifloxacin (α-Pneumococcal FQ) (Azithromycin could be substituted for Moxifloxacin too) |
|
|
What are the reasons for antibiotic overuse?
|
Patient Concerns:
- Want clear explanation - Green nasal discharge - Need to return to work Physician Concerns: - Patient expects antibiotic - Diagnostic uncertainty - Time pressure |
|
|
Which type of infection has the best use of antibiotics in terms of bacterial prevalence is high relative to antibiotic prescription?
|
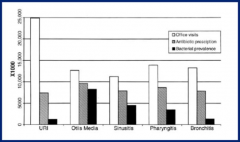
Otitis Media
|
|
|
What are the most common reasons for antibiotic treatment failure?
|
- Wrong diagnosis
- Undrained focus of infection - Foreign body - Secondary infection - Antibiotic resistance |
|
|
What are the long-term effects of being on an antibiotic?
|
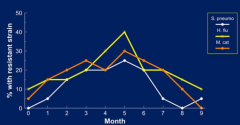
40% still have resistant strains after 5 months (so then if they get the same antibiotic within that time, it will have a higher failure rate)
|
|
|
What are the effects of misused antibiotics?
|
Leads to unnecessary adverse drug events (more ED visits d/t adverse rxns, ↑ risk of C. difficile, ↑ cost)
|
|
|
What kind of respiratory system infections are caused by viruses?
|
- Bronchitis
- Colds - Flu - Most coughs - Most ear infections - Most sore throats - Stomach flu (viral gastroenteritis) |
|
|
What kind of respiratory system infections are caused by bacteria?
|
- Bladder infections
- Wound and skin infections - Some ear infections - Strep throat - Severe sinus infections lasting > 2 weeks |
|
|
What are the instructions for appropriate usage of antibiotics?
|
- Finish entire course
- Do not borrow another person's antibiotics - Do not use expired antibiotics |
|
|
What is the most common organism responsible for outpatient treated CAP in older patients and those with significant underlying disease?
|
Streptococcus pneumoniae
|
|
|
What is the most common organism responsible for outpatient treated CAP in patients < 50 yo with no co-morbidities?
|
Mycoplasma pneumoniae
|
|
|
How do you treat CAP in outpatient setting for a healthy patient w/ no use of anti-microbials within the past 3 months?
|
- Macrolide: Azithromycin, Clarithromycin
- Doxycycline |
|
|
How do you treat CAP in outpatient setting for a patient w/ co-morbidities or use of anti-microbials within the past 3 months?
|
- Respiratory (α-pneumococcal) fluroquinolone: Levofloxacin or Moxifloxacin
OR - β-lactam (amoxicillin or w/ clavulanic acid, cefuroxime, cefpodoxime) + Macrolide |
|
|
What is the most common cause of acute sinusitis? How should it be treated?
|
Viruses account for 90-98% of all cases
Treat w/: - Anti-histamines - NSAIDs - Oral decongestants - Cough suppressant - Nasal spray w/ decongestant |
|
|
What are the most common causes of acute bacterial rhinosinusitis (ABRS)?
|
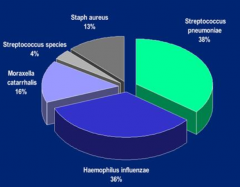
- 38% S. pneumoniae
- 36% H. influenzae - 16% Moraxella catarrhalis - 13% Staph aureus - 4% Other Streptococcus species |
|
|
What symptoms would make you think a patient has acute bacterial rhinosinusitis (ABRS)?
|
- Persistent and not improving for ≥ 10 days
- Severe and > 3-4 days - Double sickening (start w/ viral infection, got better, then got worse again probably d/t bacterial super-infection) |
|
|
How should you treat acute bacterial rhinosinusitis (ABRS)?
|
Initial Empirical therapy:
* Amoxicillin-Clavulanate bid x 14 days = Augmentin β-Lactam Allergy: - Doxycycline - Levofloxacin - Moxifloxacin Failure of Initial Therapy: - Levofloxacin - Moxifloxacin |
|
|
What are the most common primary diagnoses associated w/ S. aureus related hospitalizations?
|
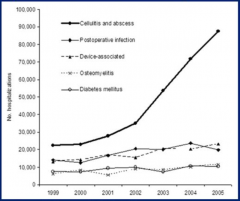
1. Cellulitis and Abscess*
2. Device-associated 3. Post-op infection 4. Osteomyelitis 5. Diabetes mellitus |
|
|
How should you manage a MRSA skin / soft tissue infection?
|
1. Cutaneous abscess: incision and drainage (primary treatment)
2. Antibiotic therapy recommended for abscesses w/: - Severe or extensive disease - Rapid progression - Co-morbidities or immuno-suppression - Abscess in area difficult to drain - Lack of response to I&D |
|
|
What antibiotics should you use to treat a MRSA skin / soft tissue infection?
|
Outpatient empiric coverage of CA-MRSA in cellulitis:
- Clindamycin - TMP-SMX - Doxycycline or Minocycline - Linezolid Inpatient complicated SSTI empiric therapy: - IV Vancomycin - IV Daptomycin - IV or PO Linezolid - IV or PO Clindamycin |
|
|
How should you manage recurrent MRSA skin / soft tissue infections?
|
- Keep draining wounds covered
- Hand and personal hygiene - Avoid sharing personal items - Environmental hygiene - Decolonization may be considered if recurrent SSTI despite wound care and hygiene OR ongoing transmission in household members or other close contacts despite wound care and hygiene |
|
|
How do you decolonize a recurrent MRSA skin / soft tissue infection? Utility?
|
- Often of limited use, but is offered in conjunction w/ ongoing reinforcement of hygiene measures
- Nasal decolonization w/ Mupirocin bid x 5-10 days - Topical body decolonization w/ Chlorhexidine or dilute bleach baths (1/4 cup bleach / 1/4 tub) - Oral antimicrobial therapy recommended only for treatment of active infection and not for decolonization |
|
|
How do you decolonize the nares?
|
- Mupirocin bid x 5-10 days
- Oral antimicrobial therapy recommended only for treatment of active infection and not for decolonization |
|
|
How do you decolonize the body/skin?
|
- Topical body decolonization w/ Chlorhexidine or dilute bleach baths (1/4 cup bleach / 1/4 tub)
- Oral antimicrobial therapy recommended only for treatment of active infection and not for decolonization |
|
|
Case: 27 yo male grad stuent presents to health services. Feels fatigued, complains of fever, swollen glands, and mild sore throat for 2 weeks. Ill-appearing w/ temp 99.9. Throat injected, no tonsillar exudates. Bilateral anterior and posterior cervical adenopathy. Mild hepatosplenomegaly. Faint, erythematous macular rash over torso.
He is given penicillin for possible "strep throat". He returns in a week still feeling bad. Strep screen negative. Monospot negative. WBC low but normal. Low hemoglobin. What is the most likely diagnosis? |
Acute Retroviral Syndrome (primary HIV infection)
|
|
|
What is the common presentation of Acute Retroviral Syndrome?
|
- Headache
- Fever - Rash - Adenopathy - Weight loss - Cytopenias, especially thrombocytopenia |

