![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
65 Cards in this Set
- Front
- Back
|
What is the volume of air inhaled during a normal inhalation?
|
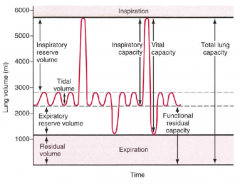
Tidal Volume (Vt)
|
|
|
What is the maximum amount of air that can be inhaled beyond the tidal volume?
|
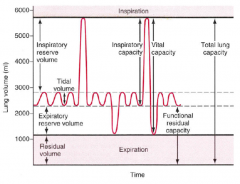
Inspiratory Reserve Volume
|
|
|
What is the maximum amount of air that can be exhaled beyond the tidal volume?
|
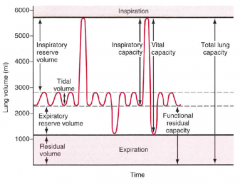
Expiratory Reserve Volume
|
|
|
What is the amount of air that can not be exhaled from the lungs?
|
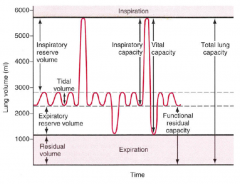
Residual Volume
|
|
|
What is the term for the amount of air that can be inhaled after a normal exhalation?
|
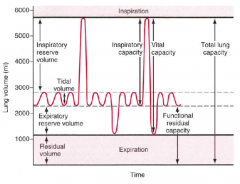
Inspiratory Capacity = Inspiratory Reserve Volume + Tidal Volume
|
|
|
What is the term for a maximal inspiration after exhaling all of your air?
|
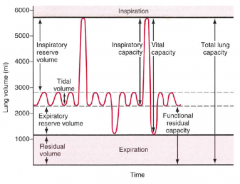
Vital Capacity = Inspiratory Reserve Volume + Tidal Volume + Expiratory Reserve Volume
|
|
|
What is the term for the amount of air remaining in the lungs after a normal exhalation?
|
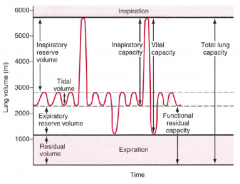
Functional Residual Capacity = Expiratory Reserve Volume + Residual Volume
|
|
|
What is the term for all of the air in the lungs after a maximal inspiration?
|
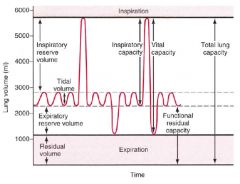
Total Lung Capacity = Inspiratory Reserve Volume + Tidal Volume + Expiratory Reserve Volume + Residual Volume
|
|
|
How do you calculate the trans-pulmonary pressure?
|
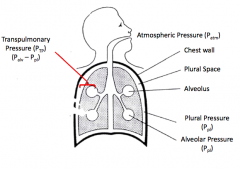
Ptp = Palv - Ppl
Transpulmonary Pressure = Alveolar Pressure - Pleural Pressure |
|
|
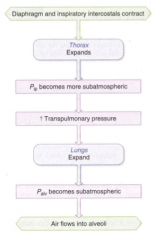
What is the sequence of events during inspiration?
|
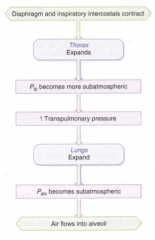
1. Diaphragm and inspiratory intercostals contract
2. Thorax expands 3. Pleural pressure becomes subatmospheric 4. Transpulmonary pressure increases 5. Lungs expand and pulls open alveoli 6. Alveolar pressure becomes subatmospheric (negative) 7. Air flows into alveoli |
|
|
What happens to the alveolar pressure during inspiration and expiration?
|
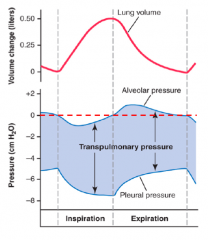
- Negative during inspiration (draws air in)
- Positive during expiration (pushes air out) |
|
|
What happens to the pleural pressure during inspiration and expiration?
|
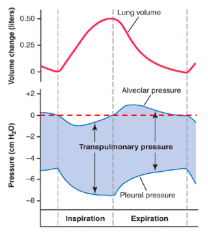
Always negative
- Becomes more negative during inspiration - Returns to normal (less negative) during expiration |
|
|
What happens to the the transpulmonary pressure during inspiration and expiration?
|
- Ppl is negative at the onset of inspiration, and becomes more negative to generate a negative Palv
- The differences between the two (Ptp) increases during inspiration - There is a greater net change in Ppl for a given change in Palv during inspiration - This occurs because the lungs are elastic structures, and there is a requirement for greater force to overcome those opposing forces - This is also reflected in the fact that expiration is (mostly) passive, due in large part to the elastic recoil of the lung - During expiration, Ptp ultimately gets smaller |
|
|
What determines airflow, particularly during expiration?
|
Flow = (Palv - Patm) / airway resistance
- As Palv increases, flow increases - As airway resistance increases, flow decreases |
|
|
Where is airway resistance greatest?
|
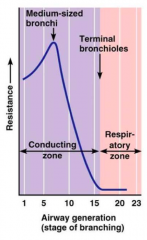
Medium sized bronchi in the conducting zone
|
|
|
Where is airway resistance lowest?
|
- Respiratory Zone (alveoli)
- For conducting zone it is lowest in the terminal bronchioles due to the vastly greater total cross-sectional area at the end of the “tree” |
|
|
How does lung volume affect airway resistance?
|
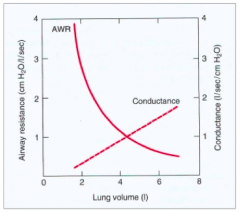
As lung volume is increased, total airway resistance decreases d/t overall increase in total airway diameter
|
|
|
When is total airway resistance highest?
|
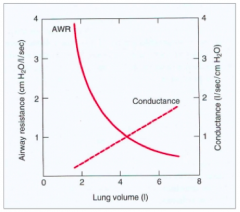
At low lung volumes, which contributes to the hysteresis of the pressure-volume relationship (see next slide)
|
|
|
What is the inverse of resistance? How is it affected by increased lung volumes?
|
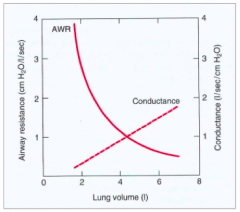
- Conductance is the inverse of resistance
- Increases with increased lung volumes - Lung compliance can be calculated as the change in lung volume (ΔV) for a given change in transpulmonary pressure (ΔPtp) *Compliance=ΔV/ΔPtp. |
|
|
How does the amount of elastic recoil relate to compliance?
|
- Elastic recoil of the lung is a mechanical property of the lung and is not physiologically regulated
- It is also conceptually the inverse of lung compliance - The more elastic recoil the lung has, the less compliant |
|
|
What happens to the (static) pressure-volume relationship in Emphysema?
|
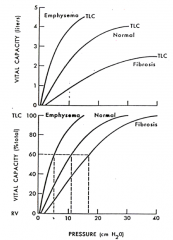
- Emphysema is a disease caused by breakdown of the lung tissue, largely due to a combination of factors (chronic inflammation/irritants like cigarette smoke)
- Tissue breakdown leads to reduced lung elasticity (increased compliance) among other factors such as airway narrowing which increases airway resistance Greater slope = increased lung compliance |
|
|
What happens to the (static) pressure-volume relationship in Fibrosis?
|
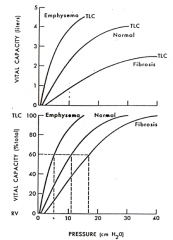
- Fibrosis is a type of interstitial lung disease in which irritants lead to an exchange of healthy lung tissue with fibrotic tissue (scarring)
- This leads to increased tissue elasticity (reduced lung compliance), and lung volume limitations Lower slope = reduced lung compliance |
|
|
If we hold airway resistance constant, what is airflow proportional to?
|
Alveolar Pressure we can generate (which is effort dependent)
|
|
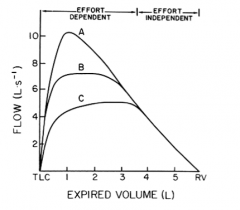
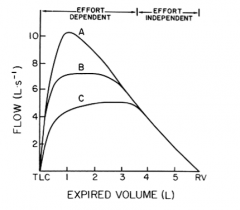
What do A, B, and C represent?
|
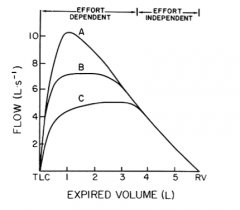
- If you inhale maximally to TLC and force expire maximally, there is an effort dependent phase and an effort independent phase.
- Shown in this figure is the relationship between lung volume expired (starting at TLC and exhaling to residual volume) and the resulting exhaled airflow - A is generated at 100% effort - B is generated at 75% effort - C is generated at 50% effort - Notice also that as you exhale more volume, the three volume-flow curves come together (around 4 liters of expired volume), demonstrating that no matter what your level of effort expired flow is the same (effort-independent phase) |
|
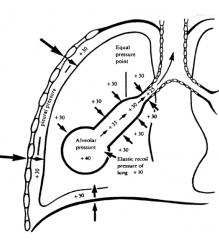
What do the big arrows represent in this image? Outcome?
|
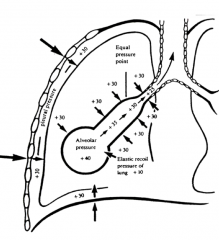
- Maximum effort (inward on the chest wall)
- Generates a large, positive plural pressure (+30 in this example) |
|
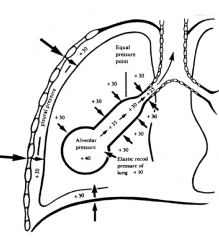
What leads to a positive pressure in the alveolar spaces (+40)? What happens?
|
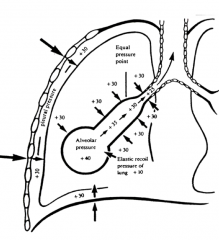
- Maximum effort of exhaling generates a large positive pleural pressure
- Combined with the natural elastic recoil tendency of the lung tissue creates an even greater positive pressure in the alveolar spaces (+40) - Because alveolar pressure far exceeds atmospheric pressure there is AIRFLOW OUT OF LUNG |
|
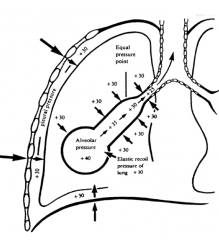
What happens as air flows out of the lungs (d/t positive alveolar pressure?
|
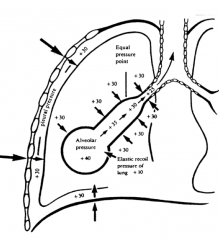
- As the airflow passes along through the airways, and as the lung volume decreases there is INCREASING airway RESISTANCE
- Increasing resistance REDUCES the net airway pressure - Creates a pressure gradient from the alveolus to the conducting airways |
|
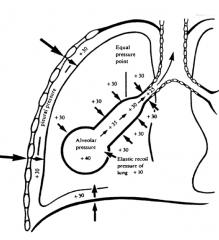
What happens as the airway pressure decreases?
|
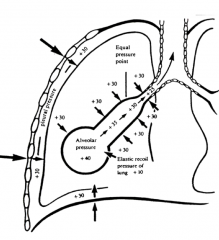
- As the airway pressure decreases it eventually reaches a point within the pleural cavity where the external positive pressure (+30) exceeds the airway pressure (+25 at the end of the airway in this figure)
- This leads to the airway tending to COLLAPSE - This collapse in turn creates GREATER RESISTANCE to airflow, and the collapsibility of the airway is highly dependent upon lung compliance |
|
|
What are the indications for Pulmonary Function Testing?
|

- Used when signs/symptoms/lab tests suggest an abnormality in lungs
- Need to determine if they are functioning properly - Helps us to determine the etiology - Also helps to assess the effects of disease and therapies |
|
|
When would you use Pulmonary Function Testing as a screening tool?
|

- Smokers
- Occupational exposures - Preoperative risk - Disability - Prognosis |
|

What values are assessed in Spirometry / PFTs?
|
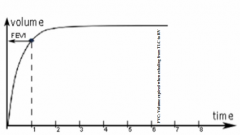
- FEV1
- FVC |
|
|
What is FEV1?
|
Forced Expiratory Volume in 1 second (maximum air you can exhale in 2 second)
|
|
|
What is FVC?
|
Forced Vital Capacity (maximum air you can exhale from total lung capacity)
|
|
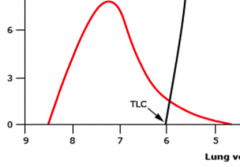
What is this kind of expiratory flow volume loop indicative of?
|
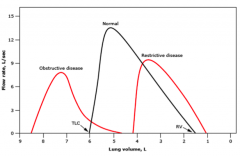
Obstructive disease: scalloped / concave
|
|
|
What disease process would make the expiratory flow volume loop smaller and at a lower volume than normal?
|
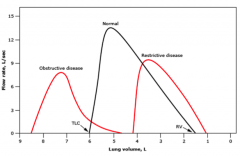
Restrictive disease
|
|
|
Will Obstructive or Restrictive disease have a higher lung volume?
|
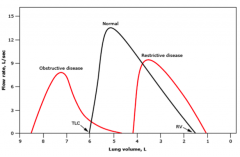
Obstructive disease has a larger volume than normal at maximum inhalation
Restrictive disease has a smaller volume than normal at maximum inhalation |
|

What is this kind of expiratory flow volume loop indicative of?
|

Fixed Large Airway Obstruction:
- Exhalation and inhalation curves are shallower than usual |
|

What is this kind of expiratory flow volume loop indicative of?
|

Extrathoracic Disease (e.g., vocal cord paralysis, goiter, etc.)
- Issue with inhalation (extrathoracic airways are smaller on inhalation) |
|

What is this kind of expiratory flow volume loop indicative of?
|

Intrathoracic Disease
- Issue with exhalation (intrathoracic airways are smaller in exhalation) |
|
|
What are the keys to interpreting spirometry?
|
- Look at FEV1/FVC ratio, FEV1, and FVC
- Always look at FEV1/FVC ratio first - FEV1/FVC <95% expected is abnormal = Obstruction - FVC <80% expected is abnormal = Restriction |
|
|
What does it tell you if the FEV1/FVC ratio is >95% of the predicted value (ratio: 0.70-0.87)?
|
Either NORMAL or RESTRICTIVE (would cause both FEV1 and FVC to be proportionally lower making ratio seem normal)
|
|
|
What does it tell you if the FEV1/FVC ratio is <95% of the predicted value?
|
Obstructive process
|
|
|
What does it tell you if the FVC <80% of the predicted value?
|
Restrictive Lung Disease
|
|
|
How do you rank the Obstructive Ventilatory Defects?
|
Based on % of Predicted FEV1:
- >99%: physiologic variant - 70-99%: mild - 60-69%: moderate - 50-59%: moderately severe - 34-49%: severe - <34%: very severe Obstructive Ventilatory Defect |
|
|
What should you do for all patients w/ spirometry showing low FEV1/FVC ratio?
|
Bronchodilator Responsivity Testing:
- A significant response to a bronchodilator is shown when the FVC or FEV1 increases at least 12% and 200 mLs |
|
|
What would indicate a positive bronchodilator responsivity test? When would you order this test?
|
- FVC or FEV1 increases at least 12% and 200 mLs
- Do for all patients w/ spirometry showing low FEV1/FVC ratio - Do for all patients suspected of asthma or chronic obstructive lung disease |
|
|
What can cause obstructive ventilation in the large conducting airways?
|
- Tumors
- Foreign bodies |
|
|
What can cause obstructive ventilation in the peripheral airways?
|
- Asthma
- Chronic Bronchitis - Cystic Fibrosis |
|
|
What can cause obstructive ventilation in pulmonary parenchymal disease?
|
Emphysematous changes from cigarette smoking
|
|
|
What can cause restrictive ventilatory defects?
|
- Interstitial lung disease: sarcoidosis, collagen vascular disease, pulmonary fibrosis
- Pneumonectomy (surgical removal of one lung) - Pleural disease: pleural effusion - Chest wall disease: kyphosis, neuromuscular disorders - Extrathoracic conditions: obesity, ascites, pregnancy |
|
|
What is the true hallmark of a restrictive ventilatory defect?
|
Reduced Total Lung Capacity
|
|
|
How do you rank the Restrictive Ventilatory Defects if a patient has a normal FEV1/FVC ratio and a decreased FVC?
|
Based on % of Predicted TLC:
- >70%: Mild - 60-69%: Moderate - <60%: Moderately Severe Restrictive Ventilatory Defect |
|
|
How do you rank the Restrictive Ventilatory Defects if you cannot obtain lung volumes?
|
Grade FVC via the obstructive FEV1 criteria
Based on % of Predicted FEV1: - >99%: physiologic variant - 70-99%: mild - 60-69%: moderate - 50-59%: moderately severe - 34-49%: severe - <34%: very severe Restrictive Ventilatory Defect |
|
|
If the FEV1/FVC ratio is normal and the TLC is low and you are following the FVC to assess Restrictive Lung Disease, how do you rank the severity?
|
Degree of restriction is based upon the percent of predicted FVC:
- 70-79%: Mild - 60-69%: Moderate - 50-59%: Moderately Severe - 34-49%: Severe - <34%: Very Severe Restrictive Ventilatory Defect |
|
|
What can the FEF50/FIF50 ratio tell you?
|
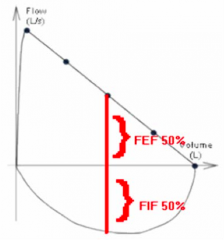
- < 1.0: Normal
- > 1.0: Variable Extrathoracic Airway Obstruction - A little > 1.0: Fixed Extrathoracic Airway Obstruction |
|
|
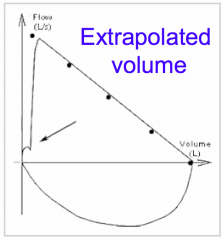
What makes a spirogram (spirometry test) acceptable?
|
- Free from artifacts such as cough or early termination
- Good start: extrapolated volume is <5% of FVC or 0.15 L, whichever is greater or time to PEF is < 120 ms - Satisfactory exhalation: 6 second of exhalation and/or a plateau int eh volume-time curve |
|
|
What makes a spirogram (spirometry test) repeatable?
|
- After 3 acceptable spirograms: are the 2 largest FVCs within 0.2L of each other? Are the 2 largest FEV1s within 0.2L of each other?
- If both of these criteria are not met, test until: both are met or a total of 8 tests - Save the 3 best maneuvers |
|
What is wrong with this spirogram?
|
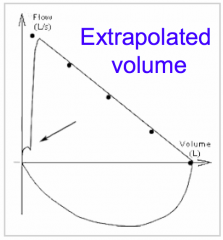
Patient hesitated at the start of the flow-volume loop: kink in curve
|
|
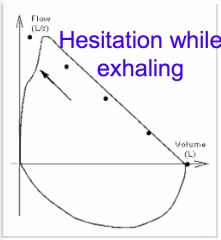
What is wrong with this spirogram?
|
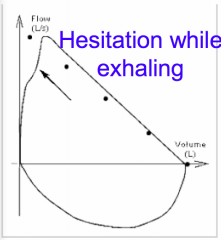
Start is too slow: the peak is not within the first 100 ms and there is a dent in the loop
|
|
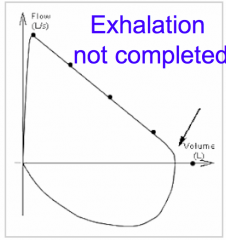
What is wrong with this spirogram?
|
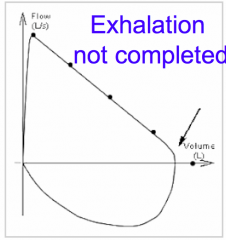
Incomplete expiration: a sudden drop at the right end of the loop, the loop is cut off
|
|
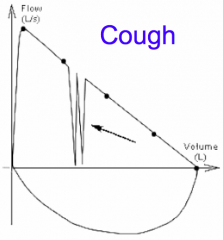
What is wrong with this spirogram?
|
Coughing during forced expiration: the loop is interrupted because of a sudden stop of flow
|
|
|
Case: A 25 year old woman who is 9 months pregnant and has a history of well-controlled asthma comes into the ED complaining of SOB and labor pains - lung examination shows some basilar rales that clear with cough and deep inspiration.
What would you expect her spirogram to look like? |
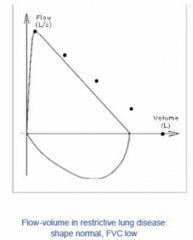
Restrictive Lung Disease:
- Shape normal - Low FVC |
|
|
Case: A 45 yo man who was in a car accident 4 years ago and suffered major blood loss and a respiratory arrest at the scene, who last month had an allergic reaction to a bee sting that required the EMS to insert an endotrachial tube to maintain his airway- he comes into the office with worsening exercise intolerance and “wheezing”.
What would you expect his spirogram to look like? |

Extrathoracic Airway problem causes problems with inspiration
- FEF50 > FIF50 |
|
|
Case: A 65 year old woman who comes into your office for a routine visit who has smoked a pack a day of cigarettes since she was 18 and has no complaints of SOB with routine activities, but when she carries groceries up the stairs she has chest tightness and sweating – lungs show no wheezes, rhonchi or rales.
What would you expect her spirogram to look like? |

She has no pulmonary issues that we can tell right now, so she should have a normal spirogram
|
|
|
Case: A 6 yo boy who gets recurrent colds that settle into his chest 2 times a year comes into the office for a back-to-school check-up – his mother feels he is doing well now that he is not sick and would not like for him to have any inhalers for fear of him being stigmatized by the other children – he is quiet but breathing comfortably reading a book, his lungs show a prolonged expiratory phase and occasional wheezing.
What would you expect her spirogram to look like? |

Obstructive Ventilatory Disease (Asthma):
- Concave expiratory phase (because problem emptying the smaller airways |

