![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
33 Cards in this Set
- Front
- Back
|
What is the equation for Q_filt (filtration flow)?
|
![Q filt = GFR * [serum]](https://images.cram.com/images/upload-flashcards/98/08/79/2980879_m.png)
Q filt = GFR * [serum]
|
|
|
What is the equation for Q_excr (excretion flow)?
|
![Q excr = UFR (urine flow rate) * [urine]](https://images.cram.com/images/upload-flashcards/98/08/82/2980882_m.png)
Q excr = UFR (urine flow rate) * [urine]
|
|
|
What is the equation for GFR? What is it dependent on?
|
![GFR = (UFR * [urine]) / [serum]
If Q filt = Q excr](https://images.cram.com/images/upload-flashcards/98/08/88/2980888_m.jpg)
GFR = (UFR * [urine]) / [serum]
If Q filt = Q excr |
|
|
Why is creatinine used to assess GFR?
|
- Creatinine is produced on constant basis by metabolism of muscle creatine
- Freely filtered by glomeruli and minimally secreted by tubules - Good marker for GFR |
|
|
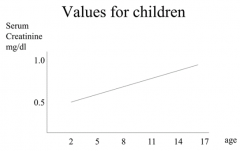
What are the normal values for serum creatinine in men? Women? Children?
|
Men: 0.9 - 1.3 mg/dl
Women: 0.8 - 1 mg/dl Children: 0.5 - 1 mg/dl (starts low and gets greater with age, d/t increased muscle mass) |
|
|
How much can serum creatinine vary based purely on analytical technique?
|
10%
|
|
|
Why are serum creatinine levels lower in women and children?
Men: 0.9 - 1.3 mg/dl Women: 0.8 - 1 mg/dl Children: 0.5 - 1 mg/dl |
Women and children have less muscle mass on average than men
|
|
|
How do you calculate Creatinine Clearance?
|
Cr Cl = (UFR * [urine]) / [serum]
UFR needs to be in ml/min |
|
|
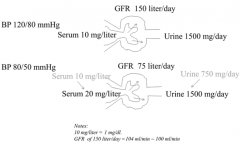
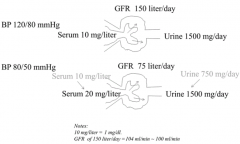
How does halving the glomeruli area affect GFR? Serum conc. of creatinine? Urine conc. of creatinine?
|
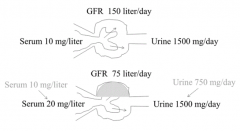
- GFR will be halved
- Serum conc. will eventually double - Urine conc. will initially halve, but eventually returns to normal value |
|
|
What is another way to estimate GFR? How does it compare to Creatinine?
|
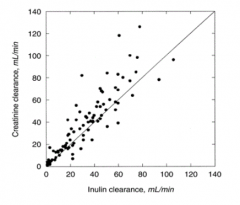
- Inject inulin because it is freely filtered and not secreted or reabsorbed
- More accurate than creatinine clearance (creatinine slightly overestimates d/t some secretion) - Rarely done in real life, but often in research |
|
|
What GFR values correspond to stages of chronic kidney disease?
|
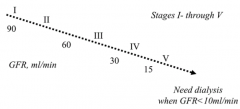
- Normal: >100 ml/min
- Stage I: ≥90 ml/min - Stage II: 60-89 ml/min - Stage III: 30-59 ml/min - Stage IV: 15-29 ml/min - Stage V: <15 ml/min |
|
|
At what GFR do you need dialysis (or kidney transplant)?
|
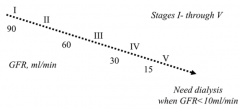
GFR < 10 ml/min
|
|
|
How is GFR related to serum creatinine?
|
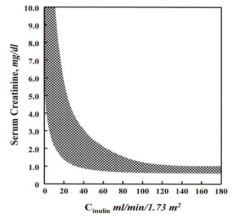
Inverse relationship between serum creatinine and GFR (inulin clearance)
|
|
|
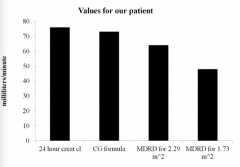
How is GFR calculated in the medical setting?
|
- MDRD Formula (don't need to know eqn)
- There are modifiers based on gender, race, and age to estimate GFR from serum creatinine - Also related to body surface area (BSA) - Also Cockcroft-Gault Formula (takes into account age, weight, gender, and serum creatinine) |
|
|
What is BUN? How does it relate to GFR?
|
- Nitrogenous waste product
- Increased BUN as GFR declines - Elevated BUN indicative of poor kidney function |
|
|
What do we need to understand as we are trying to calculate the GFR?
|
Estimates of GFR with equations are IMPRECISE
|
|
|
What can cause an acute (rapid) change in GFR?
|
Drop in BP, sepsis, etc.
|
|
|
What happens in response to an acute drop in GFR (eg, d/t suddenly low BP, sepsis)?
|
- Serum conc. gradually increases
- Urine flow of creatinine slows down but gradually recovers as serum conc. increases |
|
|
How can you assess for protein in urine?
|

- Urine dipstick
- Urinalysis |
|
|
What can you assess on urine dipstick?
|

- Proteinuria
- Hematuria - Urine pH |
|
|
How can you quantify urine protein?
|
- 24 hour urine collection (this is annoying)
- Spot urine sample (should be relatively stable, so this should be good representative of 24 hour collection) |
|
|
What causes proteinuria?
|
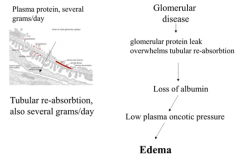
Glomerular disease → glomerular protein leak overwhelms tubular re-absorption
|
|
|
What are the outcomes of protein in urine (d/t glomerular disease)?
|
Glomerular protein leak overwhelms tubular reabsorption → loss of albumin → low plasma oncotic pressure → Edema
|
|
|
What causes edema?
|
- Glomerular Injury →
- Glomerular protein leak overwhelms tubular reabsorption → - Loss of albumin → - Low plasma oncotic pressure → - Edema |
|
|
What is the maximum amount of urine protein in healthy patients?
|
150 mg / day (not detected on urinalysis)
|
|
|
How is proteinuria graded?
|
Semi-quantitatively: 1, 2, 3, 4+
|
|
|
**What can cause nephrotic syndrome w/ edema?
|
**Urine protein more than 3g/day
|
|
What do the images on L and R represent?
|
L = normal
R = membranous GN (glomerulonephritis) - capillary loops are too thick, too much pink stuff |
|
|
What is the definition / diagnostic of micro-albuminuria?
|
- 30 - 300 mg albumin / 24 hours OR
- 20 - 30 µg / minute OR - 30 - 300 mg albumin / g of creatinine |
|
|
What does micro-albuminuria represent?
|
This does not mean "small albumin", rather it means levels of albumin that are not usually detectable on urine dipstick (30 - 300 mg albumin / g of creatinine)
= Gray zone (Precursor of kidney disease) |
|
|
What is the normal amount of albumin in urine?
|
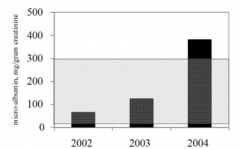
< 30 mg albumin / g of creatinine (below gray box)
|
|
|
How does the width of the glomerular basement membrane change in diabetes, micro-albuminuria, proteinuria? Implications?
|
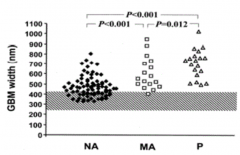
- Normal: ~300 nm
- Diabetes: some in normal range but some already w/ wider GBM - Micro-albuminuria: wider GBM - Proteinuria: widest GBM Protein leaks through GBM when thickened |
|
|
What is another possible explanation for proteinuria?
|
Not d/t kidney disease, but rather d/t overflow or overproduction of proteins (increased in multiple myeloma)
|

