![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
What are the Mendelian forms of blood pressure abnormality?
|
- Syndrome of Apparent Mineralocorticoid Excess (AME)
- Liddle Syndrome - Gitelman and Bartter Syndromes |
|
|
How does a patient with Syndrome of Apparent Mineralocorticoid Excess (AME) present?
|
- Low birth weight
- Failure to thrive - Severe HTN in early childhood - Extensive organ damage - Renal failure |
|
|
Clinically, what lab findings are associated with Syndrome of Apparent Mineralocorticoid Excess (AME)?
|
- HTN
- Hypokalemia - Metabolic alkalosis - Low plasma renin activity - Low plasma aldosterone levels |
|
|
How do you diagnose Syndrome of Apparent Mineralocorticoid Excess (AME)?
|
- Measure urine cortisol to cortisone ratio
* Very low or undetectable urinary free cortisone levels |
|
|
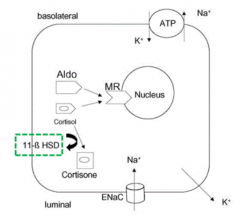
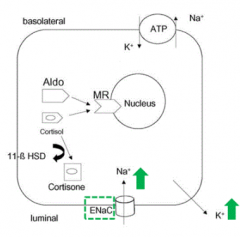
What mutation is responsible for Syndrome of Apparent Mineralocorticoid Excess (AME)? Normal function?
|
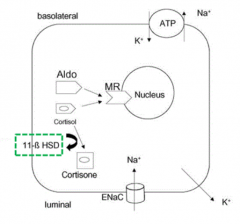
11β-HSD2 - normally functions to convert cortisol to cortisone
|
|
|
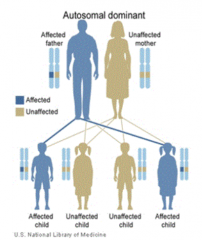
How is the mutation in Syndrome of Apparent Mineralocorticoid Excess (AME) inherited?
|
- Autosomal recessive
- Very rare mutation, so often from consanguineous relationship (same ancestors) |
|
|
What will a pedigree show for a patient with Syndrome of Apparent Mineralocorticoid Excess (AME)?
|
- May reveal affected siblings (autosomal recessive mutation - 25% chance)
- Not likely in previous generations |
|
|
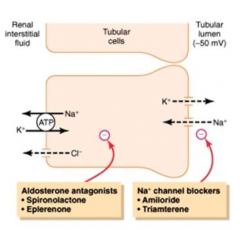
What happens if there is a mutation in 11β-HSD2 gene?
|
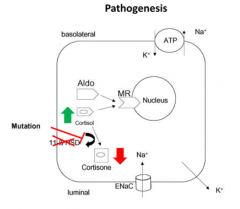
- Syndrome of Apparent Mineralocorticoid Excess (AME)
- Cortisol is not being converted to Cortisone - Build up of cortisol leads to binding to Mineralocorticoid Receptor (MR) |
|
|
What is Liddle Syndrome also known as?
|
Pseudo-aldosteronism
|
|
|
Clinically, what lab findings are associated with Liddle Syndrome? How does this compare to Syndrome of Apparent Mineralocorticoid Excess (AME)?
|
- HTN (young onset, severe)
- Hypokalemia - Metabolic alkalosis - Low plasma renin activity - Low plasma aldosterone levels * Urinary aldosterone All of the same findings as in AME, except * is new |
|
|
What mutation is responsible for Liddle Syndrome? Normal function?
|
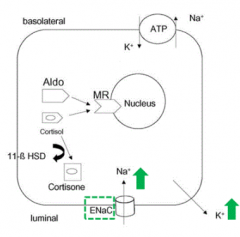
- Gain-of-function mutation in renal epithelial Na+ channel (either β or γ subunit): SCNN1G and SCNN1B genes
- Leads to constitutive expression of ENaC - Normally it is not expressed all of the time, limiting the amount of intracellular Na+ |
|
|
How do you diagnose Liddle Syndrome?
|
Gene sequencing of SCNN1G and SCNN1B genes to confirm diagnosis
|
|
|
How is the mutation in Liddle Syndrome inherited?
|
Autosomal Dominant
|
|
|
What will a pedigree show for a patient with Liddle Syndrome?
|
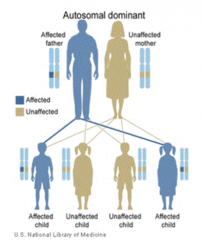
One of the parents will be affected (possibly other siblings) because it is Autosomal Dominant
|
|
|
What are the transport characteristics in the principal cells of the late distal tubule and cortical collecting duct? Regulation?
|

- Reabsorbs Na+ (ENaC)
- Secretes K+ - Regulated by aldosterone - Water permeability regulated by ADH |
|
|
What drugs antagonize aldosterone? What cells / location in nephron do they affect?
|
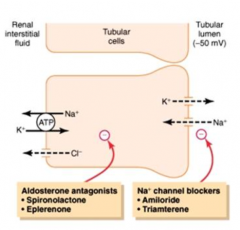
- Spironolactone and Eplerenone
- Target Principal cells of Late Distal Tubule and Cortical Collecting Duct |
|
|
What drugs antagonize Na+ Channels (ENaC)? What cells / location in nephron do they affect?
|
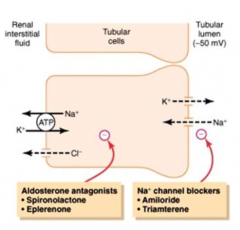
- Amiloride and Triamterene
- Target Principal cells of Late Distal Tubule and Cortical Collecting Duct |
|
|
What is the action of Aldosterone? Location of action?
|
- Increases NaCl reabsorption
- Increases K+ secretion - Increases H2O reabsorption - Acts in principal cells of late distal tubule and collecting duct |
|
|
What hormones bind the Mineralocorticoid Receptor?
|
- Aldosterone
- Cortisol (but not cortisone) |
|
|
What are the effects of Aldosterone or Cortisol binding to the Mineralocorticoid Receptor (MR)?
|
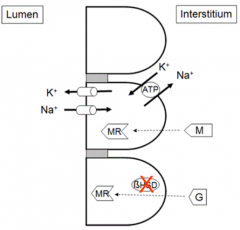
Movement of ENaC to apical membrane of principal cells (which causes more reabsorption of Na+)
|
|
|
How do you treat Apparent Mineralocorticoid Excess (AME)?
|
- Reduce endogenous cortisol production
- Decrease Na+ channel activity: Amiloride or Triamterene - Block mineralocorticoid receptor: Spironolactone or Eplerenone - K+ repletion - Dexamethasone for ACTH suppression |
|
|
What is the prognosis for Apparent Mineralocorticoid Excess (AME)?
|
Poor because of advanced progression of disease at time of diagnosis
|
|
|
How do you treat Liddle Syndrome?
|
Agents that decrease ENaC activity: Amiloride or Triamterene
|
|
|
What is the prognosis for Liddle Syndrome?
|
- Good prognosis w/ treatment w/ Amiloride or Triamterene (block ENaC)
- Without tx, cardiovascular and renal complications from uncontrolled HTN |
|
|
How does a patient with Bartter Syndrome present?
|
- Early childhood
- Growth and mental retardation - Polyuria and polydipsia (great thirst) - Hypercalciuria |
|
|
How does a patient with Gitelman Syndrome present?
|
- Adolescence / adulthood
- Cramping of arms and legs - Fatigue - Hypomagnesemia - Polyuria and nocturia |
|
|
Clinically, what lab findings are associated with Bartter and Gitelman Syndromes? How does this compare to AME and Liddle Syndrome?
|
- Hypokalemia (same)
- Metabolic alkalosis (same) * Hyper-reninemia (vs low renin activity) * Hyper-aldosteronism (vs low aldosterone activity) |
|
|
How is the mutation in Bartter and Gitelman Syndromes inherited?
|
- Autosomal recessive
- Often from consanguineous relationship (same ancestors) |
|
|
What will a pedigree show for a patient with Bartter and Gitelman Syndromes?
|
- May reveal affected siblings (autosomal recessive mutation - 25% chance)
- Not likely in previous generations (same as AME) |
|
|
What are the transport characteristics in the principal cells of the thick ascending loop of Henle? Regulation?
|
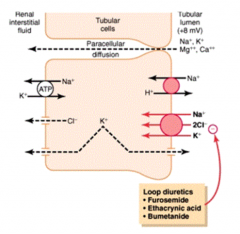
- Rabsorbs 25% of filtered Na+ by Na+/K+/2Cl- transporter
- Lumen positive potential drives paracellular reabsorption of Na+, K+, Mg2+, Ca2+ - Impermeable to H2O (dilutes tubular fluid) |
|
|
What drugs target the Na+/K+/2Cl- transporter? Location?
|
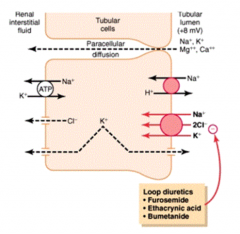
- Loop diuretic: Furosemide, Ethacrynic Acid, Bumetanide
- Thick Ascending Loop of Henle |
|
|
What are the transport characteristics in the principal cells of the early distal tubule? Regulation?
|
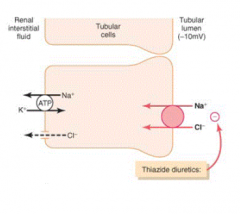
- Reabsorbs Na+, Cl-, Ca2+, and Mg2+
- Not permeable to H2O |
|
|
What drugs target the Na+/Cl- transporter? Location?
|
- Thiazide diuretics
- Early Distal Tubule |
|
|
Where are the mutations for Bartter Syndrome?
|
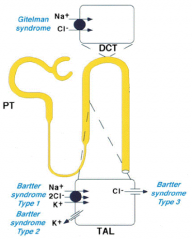
All in Thick Ascending Loop of Henle
- Type 1: Na+/K+/2Cl- transporter - Type 2: K+ channel - Type 3: Cl- channel |
|
|
Where are the mutations for Gitelman Syndrome?
|
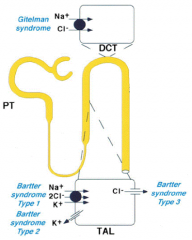
Early Distal Tubule (Convoluted)
- Na+/Cl- transporter |
|
|
Mutations in Na+/Cl- transporter cause what? What diuretic acts like this?
|
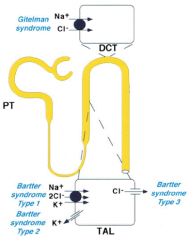
- Gitelman Syndrome
- Thiazide Diuretics |
|
|
Mutations in Na+/K+/2Cl- transporter cause what? What diuretic acts like this?
|
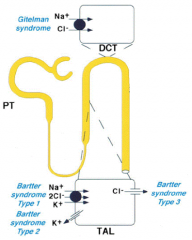
- Bartter Syndrome Type 1
- Loop Diuretics: Furosemide, Ethacrynic Acid, Bumetanide |
|
|
Mutations in K+ channel of thick ascending limb of loop of Henle cause what?
|
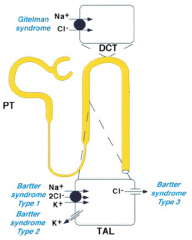
Bartter Syndrome Type 2
|
|
|
Mutations in Cl- channel of thick ascending limb of loop of Henle cause what?
|
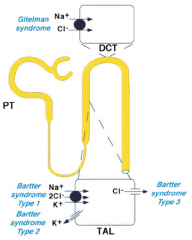
Bartter Syndrome Type 3
|
|
|
How do Bartter and Gitelman Syndromes affect salt conc., BP, Renin-Ang system? Implications?
|
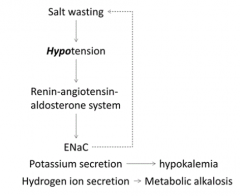
- Salt wasting
- Hypotension - Activation of Renin-Angiotensin-Aldosterone system: → Movement of ENaC channels to membrane to reabsorb Na+ (inhibits salt wasting) → K+ secretion (hypokalemia) → H+ secretion (metabolic alkalosis) |
|
|
Why do Bartter and Gitelman Syndromes cause hypokalemia?
|
Activation of Renin-Angiotensin-Aldosterone system leads to K+ secretion
|
|
|
What acid-base disturbance do Bartter and Gitelman Syndromes cause? Why?
|
Metabolic Alkalosis because activation of Renin-Angiotensin-Aldosterone system causes H+ secretion
|
|
|
What are the mutations in Bartter Syndrome?
|
- BSND
- CLCNKA - CLCNKB - KCHJ1 - SLC12A1 (genes that encode proteins in ascending part of Henle's loop) |
|
|
What are the mutations in Gitelman Syndrome?
|
- SLC12A3 gene (thiazide-sensitive Na-Cl cotransporter)
- CLCNKB (less commonly) |
|
|
What does Bartter Syndrome mimic? Gitelman Syndrome?
|
- Bartter: chronic Loop diuretic ingestion
- Gitelman: chronic Thiaxide diuretic ingestion |
|
|
What is the prognosis for Bartter and Gitelman Syndromes?
|
- Bartter: reduced in severe cases, prognosis is poor
- Gitelman: good prognosis w/ proper treatment |

