![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back
|
What is the pathway of renal failure?
|
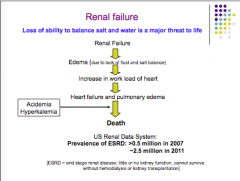
Renal failure --> edema --> increase in heart workload --> heart failure and pulmonary edema --> death
|
|

Label each.
|
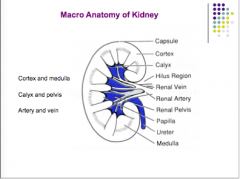
From top to bottom:
Capsule, cotrex, calyx, hilus region, renal vein, renal artery, renal pelvis, papilla, ureter, medulla |
|

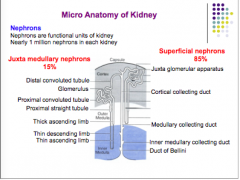
Label each:
What is the functional units of the kidney What percent are juxta medullary? What percent superficial? |
|
|

Label each:
|
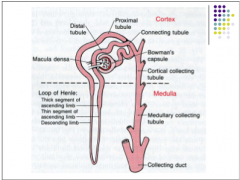
|
|
|
Describe the pathway of the vasculature of kidneys:
|
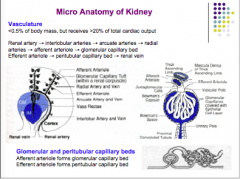
Renal artery --> interlobular arteries --> arcuate arteries --> radial arteries --> afferent arteriole --> glomerular capillary bed...efferent arteriole --> peritubular capillary bed --> renal vein
|
|
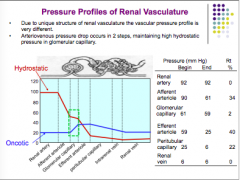
Review this:
|
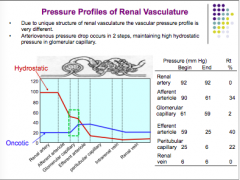
Review this:
|
|
|
What are the three processes of urine formation?
|
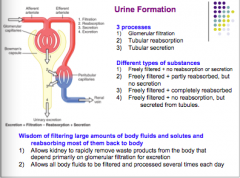
1. Glomerular filtration
2. Tubular reabsorption 3. Tubular secretion |
|
|
What are the four different types of substances in urine formation?
|
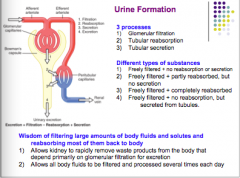
1. Freely filtered + no reabsorption or secretion
2. Freely filtered + partly reabsorbed, but no secretion 3. Freely filtered + completely reabsorbed 4. Freely filtered + no reabsorption, but secreted from tubules |
|
|
Why do you filter large amounts and reabsorb most?
|
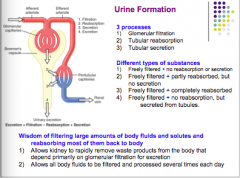
1. Allows kidneys to remove waste products from body that depend primarily on glomerular filtration rate for excretion
2. Allows all body fluids to be filtered and process several times each day |
|
|
What is the GFR?
What is the filtration fraction? |
130 mL/min (180 L/day --> decreases with age and renal disease)
FF = GFR/renal plasma flow (RPF) |
|
|
What are factors that reduce GFR?
What are factors that reduce RPF? |
Uretal obstuction --> reduced FF
Renal artery stenosis --> increases FF |
|
|
What are three filtration barriers?
|
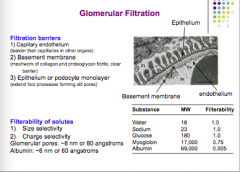
Capillary endothelium
Basement membrane Epithelium or podocyte monolayer |
|
|
Rank the following in terms of filterability.
Water, sodium, glucose, myoglobin, albumin |
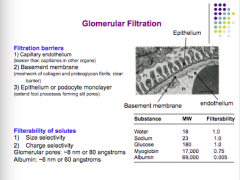
|
|
|
What is the equation GFR? (Starling)
What affects Kf? Disease? |
GFR = Kf * net filtration pressure
Kf = hydraulic conductivity x surface area of glomerular capillary Diabetes mellitus: reduced Kf, increased thickness of basement membrane, and damaged capillaries. |
|
|
What is the equation for net filtration pressure?
|
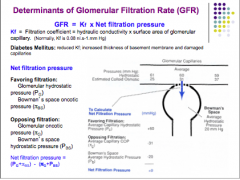
Net filtration pressure = (Pglom-Pbs) - (osmotic glom - osmotic bowmans)
Assume osmotic bowmans = 0, no protein in the space |
|
|
What is the effect of Rt higher in afferent or lower in efferent?
What is the effect of low Rt inafferent or high in efferent? |
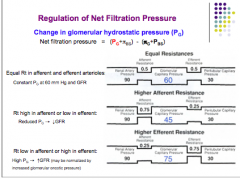
Reduced Pg --> decreased GFR
High Pg --> increased GFR (may be normalized by increased glomerular osmotic pressure) |
|
Complete the chart.
|
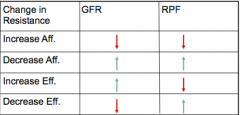
|
|
|
What are some things that can affect Pbs (Bowman's hydrostatic pressure)?
What is the effect of an increase in Pbs? What can cause a decrease in Pbs? |
Pbs = resistance of nephron and rate of urine flow
Obstruction in lower urinary tract = kidney stone, tumor, hypertrophic prostate in elderly Increase Pbs --> decrease in net filtration pressure --> decrease in GFR Frequent emptying of bladder --> decreased Pbs --> increase net filtration pressure --> increase GFR |
|
|
What are the two endocrine functions of the kidney?
|
1. conversion of vitamin D3 to calcitrol
2. Synthesis of erythopoietin (sole source) |
|
|
What can cause a change in the glomerular osmotic pressure?
What is the effect of low capillary flow on this? |
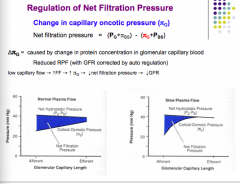
Change in protein concentration in the glomerular capillary bed
Low capillary flow --> increased filtered fraction --> increased glomerular osmotic pressure --> decreased net filtration pressure --> decreased GFR |
|
|
True or false.
Auto regulation is independent of systemic influences and can occur in an isolated kidney. What are some things that cause activation of GFR auto regulation? |
True
Mean arterial pressure, venous pressure, obstruction changes |
|
|
In the absence of autoregulation, what would happen to GFR if there was an increase in arterial pressure? Urine?
|
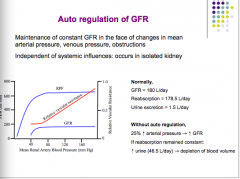
Increase arterial pressure --> increase GFR
If reabsorption constant: Increased urine --> depletion of blood volume |
|
|
What is the MAIN control of auto regulation?
Draw the pathway. |
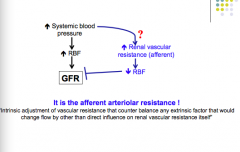
AFFERENT ARTERIOLE RESISTANCE!
|
|
|
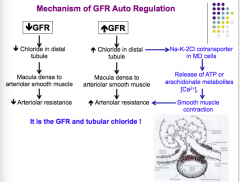
What are the two theories of the changing vascular tone of autoregulation? Explain each.
|
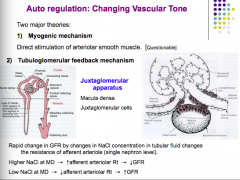
1. Myogenic: Direct stimulation of arteriolar smooth muscle (think stretch and opening of Ca2+ channels which leads to increased muscle contraction)
2. Tubuloglomerular feedback mechanism: Macula densa senses changes in NaCl and secretes metabolites to adjust arteriolar resistance. |
|
|
What are the mechanisms of renin release?
|

1. Baroreceptor mechanism: increased pressure in AFFERENT arterioles inhibits renin release from JG cells
2. Sympathetic nerves: B-1 adrenergic nerves stimulate renin release 3. Macula densa mechanism: Increased NaCl in distal nephron inhibits renin release, decreased load promotes renin release. |
|
|
What are the two pathways that relate increases or decreases in GFR to changes in arteriolar resistance?
|
|
|
|
What are the renin-angiotensin system pathways for how decreased GFR eventually leads to an increase or decrease in GFR?
|
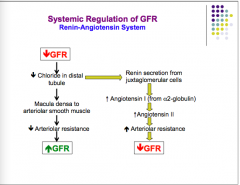
|
|
|
What is the effect of sympathetic activation on GFR (pathway)? What does it stimulate? Is this important under normal conditions? Is it important under severe ECFV loss? Does this decrease Kf?
|
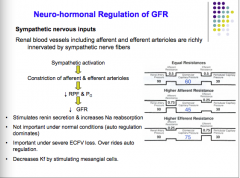
|
|
|
What are the effects of adrenaline, endothelin-1, and NO/prostaglandins on GFR (pathways)?
|
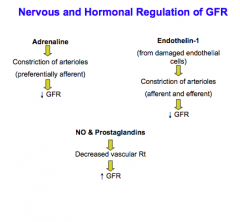
|
|
|
What are two causes of proteinuria?
What is the difference between NEPHRITIC syndrome and NEPHROTIC syndrome? |
Barrier failure:
Visible barrier breakdown: "large pore" --> nephritic syndrome (loss of blood?) Invisible barrier breakdown: "loss of charge selectivity" --> nephrotic syndrome (loss of protein?) |
|
|
Another cause of proteinuria (circulation)?
|
Abnormal circulating protein from breakdown of tissue or from production of abnormal proteins (cancer, tumor cells)
|

