![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back

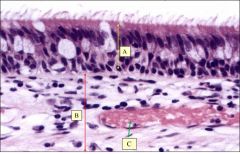
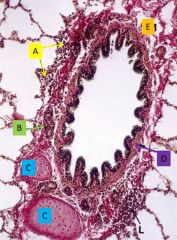
Structures and their functions |
A - venous sinuses adjust air to body temp by heat exchange B - Serous glands and D - Mucous glands secretions trap particulate matter and humidify inspired air C - pseudostratified columnar epithelium
|
|
|
What are the (5) cell types in the respiratory epithelium and what are their functions? |
Goblet cells contribute to mucous Ciliated cells move mucous Neuroendocrine cells are regulatory Brush cells are chemosensory Basal cells resupply other cell types |
|
|
A - Epithelium B - Lamina propia C - Venule |
|
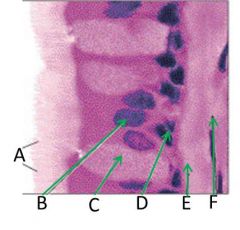
Structures (B is a nucleus) |
A - Cilia B - Columnar epithelial cell nucleus C - Goblet cell D - Stem cell E - Basement membrane F - Lamina propria |
|
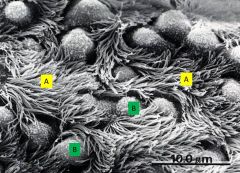
Surface of the respiratory epithelium - whole structure represents what? |
Mucociliary elevator A - Cilia B - Goblet cells |
|
|
How does the mucociliary elevator work? |
Mucous gel moves over the immobile ciliary layer as it is continually swept up and swallowed. The tethered movement of the cilia propels the mobile gel. |
|
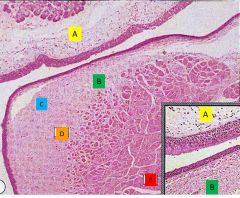
Histology of the larynx |
A - ventricular folds (respiratory epithelium and glands) B - vocal folds (stratified squamous epithelium, C - Reinke's spaces with few lymphatic vessels, D - vocal ligament fibroelastic tissue, E - vocalis skeletal muscle) |
|
|
How do epithelial and subepithelial components of the airway change as the airway approach the alveoli |
There are decreases in mucous producing cells, epithelial height and subepithelial connective tissue |
|
|
Regions of the pharynx and larynx exposed to high speed airflow are lined by... |
stratified squamous epithelium (NOT respiratory epithelium) |
|
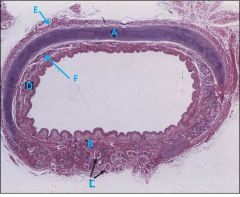
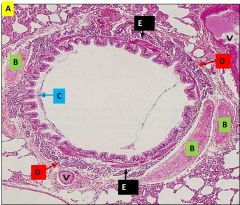
Organization of the tracheal wall |
A - cartilagenous layer C-shaped ring B - Trachealis muscle (where the cartilage is incomplete posteriorly) closes the ring C - Longitudinal muscle may be present behind the trachealis D - mucosa (respiratory epithelium and lamina propria) E - adventitia (connective tissue, blood vessels, lymphatics, nerves) |
|
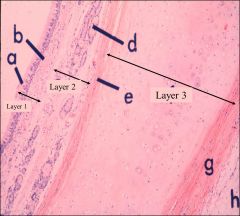
Tracheal wall |
Layer 1 (innermost) = mucosal, Layer 2 = submucosal, Layer 3 = cartilage A - epithelium B - lamina propria D - tracheal glands E - perichondrium G - perichondrium H - adventitia
|
|
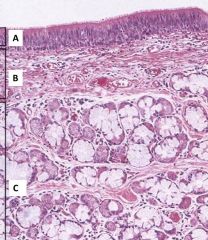
Respiratory epithelium - layers and their components |
A - respiratory epithelium (ciliated, goblet, neuroendocrine, basal, brush) B - Lamina propria (loose connective tissue and venous sinuses) C - Submucosa (mixed mucous and serous glands, relatively loose connective tissue) |
|
|
Changes in cellular makeup from the upper to lower trachea |
Increase in relative proportion of ciliated cells due to decreased relative proportion of goblet and basal cells |
|
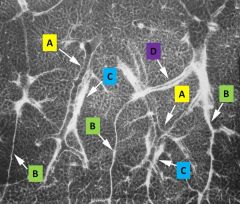
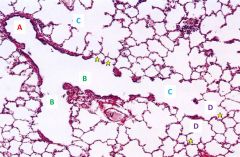
Lung parenchyma - secondary pulmonary nodule |
A - bronchioles are centrilobular B - interlobular septa contain (D) the pulmonary vein segments C - arteries are centrilobular |
|
|
Progressive changes along bronchial tree |
decrease in cartilage and glands (those two will disappear at bronchioles), goblet cells, and height of epithelium increase in smooth muscle and elastic tissue |
|
|
Epithelial transitions along the bronchioles |
There is a gradual transition from simple columnar epithelium (few goblet cells) to simple cuboidal epithelium (many cells with cilia) with a few club cells (Clara cells). There is a narrowing of the lamina propria with less smooth muscle but continuing elastic fibers. |
|
|
How do diameter, cross-sectional area, and airspeed change as you go deeper along the bronchioles? |
Although the diameter is shrinking, the total cross-sectional area is increasing because of the branching and therefore airspeed is slowed |
|
Intrapulmonary bronchus - identify and describe - what is in the lamina propria? |
Note the lamina propria is thin and with elastic fibers A - aggregations of lymphocytes B - glands in the submucosa (E) which blends with the adventitia C - cartilage in discontinuous plates D - smooth muscle is deep to the mucosa |
|
|
Epithelial changes as the bronchi get smaller |
Epithelium is less pseudostratified and more columnar and with less goblet cells |
|
Name this tube! (ignore A) |
Intrapulmonary bronchus B - cartilage plates C - respiratory epithelium D - glands in the submucosa E - smooth muscle deep to the mucosa V - blood vessels associate with the bronchus |
|

Name this tube Identify M and its function? Other identifying features |
Bronchiole M = smooth muscle layer is prominent and regulates air flow Thin submucosa without glands Connective tissue but no cartilage |
|
|
What are Clara cells? |
The non-ciliated, epithelial club cells occur in high frequency in the smaller bronchioles and produce a surfactant-like lipoprotein |
|
Transition from conducting to respiratory zone |
A - Terminal bronchioles (last part of conducting airway) B - Respiratory bronchioles C - alveolar ducts are linear arrangements of alveoli as they terminate in alveolar sacs (star) D -
|
|
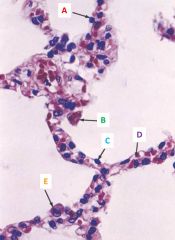
Components of the alveolar wall |
A - type I pneumocyte B - alveolar macrophage C - endothelial cells D - capillaries E - type II pneumocyte |
|

Components of the alveolar wall |
A - type II pneumocyte B - epithelial cell C - alveolar macrophage D - type I pneumocyte E - capillary |
|
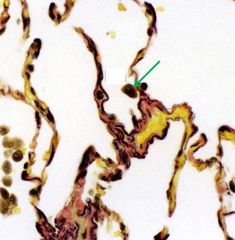
Alveolar wall - what are the structural components and the indicated cell? |
Structural components - elastin (black) and collagen (pink) Alveolar macrophage is indicated |
|
|
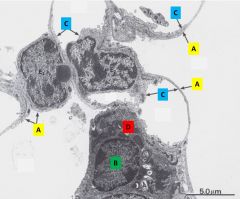
A - type I pneumocytes B - type II pneumocytes C - endothelial cells within the capillaries D - lamellar body within type II pneumocytes |
|
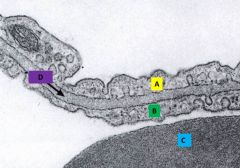
Blood air barrier |
A - type I pneumocyte (on the alveolar side) B - endothelial cell (on the capillary side) C - RBC inside the capillary D - fused BM of the epithelial pneumocyte and endothelial cell |
|
|
What do pulmonary arteries follow? |
Pulmonary arteries follow the bronchial tree |
|
|
What do pulmonary veins follow and where are they located? |
Pulmonary veins are located in the margins of the lobules and follow the larger bronchi |
|
|
What do bronchial arteries follow? |
Bronchial arteries follow the bronchial tree |
|
|
Where are bronchial veins? |
Bronchial veins are only evident near the hilus |
|
|
What do intrapulmonary nerves follow? |
Intrapulmonary nerves follow the bronchial tree |
|
|
What is the structural differences between pulmonary arteries, pulmonary veins, and bronchial arteries? |
Pulmonary veins are the largest and thin walled Pulmonary veins are large and thicker walled Bronchial arteries are small and within or closely associated with the wall of the bronchus |
|
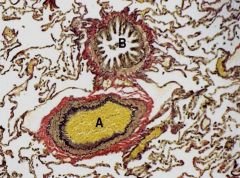
Name these tubes |
A - Pulmonary artery - lots of elastic tissue (in black) and relatively little smooth muscle (brown); the walls are fairly thin because of low pressure in pulmonary circulation B - Bronchiole - smooth muscle (brown) and collagen (pink) |
|
|
What three groups of nerves innervate the lungs? |
parasympathetic, sympathetic, and general visceral afferent nerves |
|
|
Where are the two lymphatic plexuses? Where do they interconnect? |
Superficial plexus in the pleura Deep plexus accompanies the blood vessels and the bronchi in the septa They meet at the hilum where the tracheobronchial lymph nodes are located |
|
|
Where are lymphatic vessels never found |
Lymphatic vessels are never found in the alveoli |
|
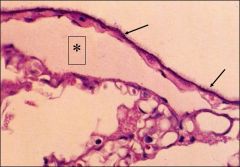
Structures of the surface lymphatics |
* = a pleural lymphatic vessel confirmed by the brush border (arrows) of mesothelial cells of the visceral pleura Note the thin wall and endothelial cells of the vessel with a modest amount of connective tissue below the mesothelial cells of the pleura |
|
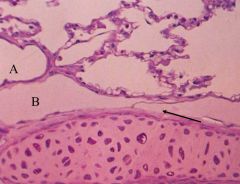
Identify the deep lymphatics vs the blood vessel Arrow? |
A - blood vessel B - lymphatic vessel alongside the bronchus (you can tell bc of the cartilage plate) Arrow indicates a valve that helps maintain centripetal flow of the lymph |
|
|
What aids lymph movement? |
Mostly the pulsations of the blood vessels with which they are intertwined Smooth muscle contraction in the walls of the large lymph vessels Respiratory movements
|
|
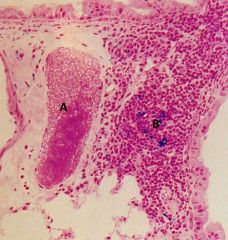
What are these immune structures? Cell type? Where does it exist? |
A - Lymphatic vessel B - Lymphatic nodule (associated with the vessel) full of lymphocyte Lymphoid tissue exists at bronchial branch points |
|
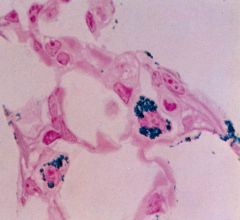
What are the jobs of the alveolar macrophages (blue stain is inhaled iron oxide) |
Fight contamination by organisms and particulates Ingest excess surfactant |

