![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
522 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What type of disease is mumps?
|
parotitis
|
|
|
|
Where does the trachea divide into the main bronchi?
|
T4/T5; just below manubriosternal joint
|
|
|
|
What is the etiology of mumps?
|
caused by a paramyxovirus; spread via respiratory droplets; usually affects children
|
Current p1250
|
|
|
Which main bronchus is more susceptible to foreign body aspiration and why?
|
RT main bronchus
shorter, wider, more vertical than LT main bronchus |
|
|
|
What is the clinical presentation of mumps?
|

incubation 2-3 weeks before onset
fatigue and fever → variable parotid gland enlargement → unilateral or bilateral, usually one enlarges before the other stenson's duct → erythematous, edematous parotid tenderness facial edema +/- trismus +/- submaxillary and sublingual gland involvement |
Current p1250
|
|
|
What are the primary respiratory muscles?
|
diaphram, external intercostals, and internal intercostals
|
|
|
|
What is the diagnostic work-up of mumps?
|
usually diagnosed clinically; swab parotid duct for confirmation via NAAT (more sensitive), viral culture or serum IgM
|
Current p1250
|
|
|
What is the function of the diaphram?
|
moves inferiorly during inspiration to increase intrathoracic pressure
|
|
|
|
What are the complications of mumps?
|
pancreatitis →affects children; upper abdominal pain, nausea, vomiting
orchitis → affects 25-40% postpubertal men, high fever, testicular swelling and tenderness oophoritis → affects 5% of postpubertal women, lower abdominal pain, ovarian enlargement meningitis → high fever, headache, stiff neck, lethargy |
Current p1250
|
|
|
What are the function of the external intercostals?
|
increase AP chest diameter during inspiration
|
|
|
|
Mumps is the most common cause of what disease in children?
|
pancreatitis
|
Current p1250
|
|
|
What are the function of the internal intercostals?
|
decrease transvere chest diameter during expiration
|
|
|
|
What is the management of mumps?
|
Symptomatic:
1. topical compresses 2. bed rest until afebrile 3. isolation until swelling subsides (9 days following onset) |
Current p1250
|
|
|
What are the accessory respiratory muscles?
|
sternocleidomastoid
trapezius |
|
|
|
What is the ddx for parotidis?
|
dehydration → stasis of salivary flow
sialolithiais of stenson's duct bacterial infection viral infection cyst or tumor etc |
Current p1250
|
|
|
Where is the carotid body found?
|
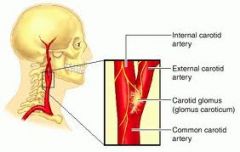
bifurcation of the common carotid arteries
|
|
|

|
mumps
|
|
|
|
What is the function of the carotid body?
|
contains chemoreceptors that respond to changes in arterial [O2] and [CO2] → send signal to respiratory center in medulla oblongata → medulla oblongata sends nerve impulses to pons → pons regulates respiratory muscles
|
|
|

|
mumps
|
|
|
|
What is the function of the medulla oblongata in respiration?
|
contains chemoreceptors that respond to changes in blood/CSF [H+] → sends signals to respiratory center in medulla oblongata → medulla oblongata sends nerve impulses to pons → pons regulates respiratory muscles
|
|
|
|
What is the etiology of diphtheria?
|
caused by corynebacterium diphtheriae; spread via respiratory droplets; rare due to TDAP vaccine; infectious disease emergency
|
Current p204
|
|
|
What 2 types of chemoreceptors help regulate respiration?
|
medual oblongata chemoreceptors → respond to changes in blood/CSF [H+]
carotid body chemoreceptors → respond to changes in arterial [O2] and [CO2] |
|
|
|
What is the clinical presentation of pharyngeal diphtheria?
|
mild fatigue, fever, sore throat; gray tonsillar pseudomembrane covering tonsils and pharynx
|
Current p204
|
|
|
Where should you begin counting ribs?
|
2nd rib
find manubriosternal joint since this is where 2nd rib articulates |
|
|
|
Where should you begin counting vertebra?
|
vertebra prominens (C7)
more easily palpated if neck flexed *but remember the rib you feel in association with a spinous process is that spinous process + 1 |
|
|
|
What is the diagnostic work-up of diphtheria?
|
diagnosis made clinically but can be confirmed by culture
|
Current p1302
|
|

|

|
|
|
|
What are the complications of diphtheria and their associated symptoms?
|
myocarditis → cardiac arrhythmias, heart block, heart failure
neuropathy → initally affects CNs → diplopia, dysphagia, slurred speech |
Current p1302
|
|

|

|
|
|
|
What is the management of diphtheria?
|
1. antitoxin (obtained from CDC)
2. if potential or current airway obstruction → remove pseudomembrane via laryngoscopy or bronchoscopy 3. penicillin 250mg PO 4x daily x 14 days or erythromycin 500mg PO 4x daily x 14 days 4. isolation until 3 consecutive cultures at completion of therapy confirm elimination 5. treat patient contacts → erythromycin 500mg PO 4x daily x 7 days; diphtheria booster |
Current p1302
|
|
|
Where are the lung apices anteriorly and posteriorly?
|
anteriorly → 4cm above 1st rib
posteriorly → T1 |
|
|
|
Where are the lung bases anteriorly and posteriorly?
|
anteriorly → 6th rib at midclavicular line
posteriorly → T12 on deep inspiration, T9 on forced expiration |
|
|
|
What is the prevention of diphtheria?
|
TDAP vaccination
|
|
|
|
What is the equipment needed for the respiratory exam?
|
stethoscope
marking pencil cm ruler cm measuring tape |
|
|
|
List signs of respiratory distress.
|
cyanosis → skin, lips, tongue, nipples, nails
nostril flaring pursed lip breathing accessory respiratory muscle use → sternocleidomastoid, trapezius retractions → visible on inspiration clutching tripodding tachypnea grunting stridor wheezing anxiety |
|
|
|
retractions and tripodding → respiratory distress
|
|
|
|
Compare and contrast the clinical presentation of the common cold, influenza, and H1N1.
|
common cold → gradual onset, sneezing, nasal congestion, watery rhinorrhea, sore throat, cough
influenza → rapid onset, fatigue, high fever, headache, body aches, chills, nasal congestion, rhinorrhea, sore throat, cough H1N1 → fatigue, fever, headache, body aches, chills, nasal congestion, rhinorrhea, sore throat, cough, vomiting, diarrhea |
|
|
|
Breath that smells like cinnamon may indicate?
|
pulmonary TB
|
|
|
|
How long does a SPUTC remain positive?
|
possibly several weeks
*do not give additional antituberculous drugs b/c you think the patient is not responding to tx |
Interpreting Laboratory Data p7
|
|
|
How long does a SPUTC remain positive?
|
possibly several weeks
*do not give additional antituberculous drugs b/c you think the patient is not responding to tx |
Interpreting Laboratory Data p7
|
|
|
What is another name for pneumococcal pneumonia?
|
strep pneumonia
|
|
|
|
Breath that smells sweety or fruity may indicate?
|
diabetic ketoacidosis
starvation ketosis |
|
|
|
What is the etiology of pneumococcal pneumonia?
|
caused by streptococcus pneumoniae; community-acquired and hospital-acquired pneumonia
|
|
|

|
pericardial effusion
|
Current ch10
|
|
|
What is the diagnostic work-up of pneumococcal pneumonia?
|
BC
sputum gram → gram-pos diplococci sputum culture CXR → consolidating lobar pneumonia |
|
|
|
Breath that smells fishy or stale may indicate?
|
uremia
|
|
|
|
What is the definition of a good sputum sample?
|
<10 epithelial cells and >25 PMNs per high-power field
|
Current p1252
|
|
|
Breath that smells like ammonia may indicate?
|
uremia
|
|
|
|
What are the complications of pneumococcal pneumonia?
|
parapneumonic effusion
empyema pericarditis endocarditis |
Current p1252
|
|
|
Feculant smelling breath may indicate?
|
GI obstruction
|
|
|
|
What is the clinical presentation of pneumococcal pneumonia?
|
high fever, chills, dyspnea, productive cough, +/- hemoptysis, pleuritic chest pain, bronchial breath sounds
|
Current p1252
|
|
|
Breath that smells foul or putrid may indicate?
|
nasal/sinus pathology → foreign body, infection, cancer
respiratory pathology → insistent bronchitis, bronchiectasis, empyema, lung abscess, anaerobic infection |
|
|
|
What is the management of pneumococcal pneumonia?
|
1. empiric treatment until isolation of s. pneumo
2. if uncomplicated → amoxicillin 3. if penicillin-resistant strain → vancomycin |
Current p1252
|
|
|
Breath that smells fishy or like clover may indicate?
|
portal vein thrombosis, hepatic failure
|
|
|
|
What is the common name for pertussis?
|
whooping cough
|
Current p1308
|
|
|
Halitosis may indicate?
|
gingivits, necrotizing ulcerative gingivitis, tonsillitis, respiratory infection, GERD
|
|
|
|
What is the etiology of pertussis?
|
caused by bordetella pertussis; spread via respiratory droplets; 50% before 2y/o
|
Current p1308
|
|

|
sternal indentation → pectus excavatum
|
|
|
|
What is the prevention of pertussis?
|
TDAP vaccination
|
Current p1308
|
|
|
What is the common name for pectus excavatum?
|
funnel chest
|
|
|
|
What is the management of pertussis?
|
1. erythromycin 500mg PO 4x daily x 7 days
2. offer erythromycin to contacts if exposed within 3 weeks of onset |
Current p1308
|
|
|
What is the common name for pectus carinatum?
|
pigeon chest
|
|
|
|
What is the clinical presentation of pertussis?
|
1. catarrhal stage → fatigue, lacrimation, sneezing, rhinorrhea, hacking night cough, anorexia
2. paroxysmal stage → whooping cough 3. convalescent stage → decrease in severity of whooping cough, 4 weeks after onset entire illness lasts 6 weeks |
Current p1308
|
|

|
sternal protrusion → pectus carinatum
|
|
|
|
What is the diagnostic work-up of pertussis?
|
collect nasopharyngeal dacron swab
pertussis PCR or pertussis culture with bordet-gengou agar |
Current p1308
|
|
|
Define pectus carinatum.
|
sternal protrusion
|
|
|
|
What is the etiology of legionnaire's disease?
|
caused by bacteria legionella pneumophilia; transmitted via contaminated water sources like heating and cooling systems of hospitals; not spread via person-to-person; increased risk in smokers, chronic lung disease, immunocompromised
|
Current p1310
|
|
|
Define pectus excavatum.
|
sternal indentation
|
|
|
|
What is the clinical presentation of legionnaire's disease?
|
fatigue, fever, chills, HA, cough
atypical pneumonia → scant sputum, pleuritic chest pain |
Current p1310
|
|
|
Define lordosis.
|
anterior spinal deviation
|
|
|
|
What type of pneumonia is legionnaire's disease?
|
community acquired
atypical |
Current p1310
|
|
|
Define kyphosis.
|
posterior spinal deviation
|
|
|
|
What is the diagnostic work-up of legionnaire's disease?
|
sputum GRAM → no bacteria
sputum PCR or culture CXR → patchy infiltrates or consolidation, often bibasal consolidation |
Current p1310
|
|
|
Define gibbus.
|
extreme kyphosis
|
|
|
|
Where is legionella naturally found?
|
water
|
|
|
|
Define scoliosis.
|
lateral spinal deviation
|
|
|
|
What is the management for legionnaire's disease?
|
1. azithromycin 500mg PO 1x daily x 10-14 days
2. if immunocompromised → extend treatment to 21 days 3. DO NOT prescribe erythromycin |
Current p1311
|
|

|
anterior spinal deviation → lordosis
|
|
|
|
Is legionnaire's contagious from person-to-person?
|
no
|
|
|

|
posterior spinal deviation → kyphosis
|
|
|
|
What is the etiology of hemophilus influenzae pneumonia?
|
caused by bacteria hemophilus influenzae; community-acquired pneumonia
|
|
|

|
lateral spinal deviation → scoliosis
|
|
|
|
What is the diagnostic work-up of hemophilus influenzae pneumonia?
|
sputum GRAM → gram-neg coccobacilli
sputum PCR or culture CXR |
|
|
|
Describe the respiratory exam.
|
1. introduce self
2. wash hands 3. ask patient to lower gown to waist 4. assess general appearance → gender, age, acutely or chronically ill, signs of respiratory distress, breath odor 5. BP and HR 6. respiratory rate and pattern 7. inspect anterior, lateral, and posterior chest while patient breathing normally, then while breathing deeply → shape, symmetry, AP diameter, deformities 8. inspect for supernumerary nipples (sign of congenital disorders), superficial venous patterns (sign of heart or vascular disease), rib prominence/fat (nutritional deficiencies) 9. inspect nails for cyanosis and clubbing at eye level 10. measure chest wall expansion 11. palpate for tracheal deviation |
|
|
|
What is the general presentation of community-acquired pneumonia?
|
acute fever, dyspnea
cough +/- sputum fatigue, chills, rigors, sweats, HA, hemoptysis, pleuritic chest pain, abdominal pain, myalgia, altered breath sounds, crackles, dullness to percussion if parapneumonic pleural effusion |
Current p246
|
|
|
Define barrel chest.
|

increase in AP chest diameter
ratio of AP and transverse chest diameter is 1:1 instead of 1:2 |
|
|
|
What are the most common causes of community-acquired pneumonia?
|
1. pneumococcal pneumoniae
2. mycoplasmal pneumoniae 3. hemophlius influenza 4. legionnairese 5. aspiration 6. respiratory viruses |
|
|
|
What are the characteristics of barrel chest?
|
increase in AP chest diameter
manubriosternal joint more prominent ribs more horizontal spine more kyphotic trachea may be posteriorly displaced |
|
|
|
What are the most common causes of hospital-acquired pneumonia?
|
1. streptococcal pneumoniae
2. staph aureus 3. legionnaires |
|
|
|
Define flail chest.
|
chest wall fracture with complete detachment
|
|
|
|
Define diaphragmatic paradox.
|
paradox movement of chest wall
during inspiration, segment of chest wall moves inward instead of expanding during expiration, segment of chest wall moves outward instead of retracting |
|
|
|
Diaphragmatic paradox may indicate?
|
flail chest
|
|
|
|
What is the cause of flail chest?
|
trauma
|
|
|
|
Asymmetrical lung expansion may indicate?
|
if unequal or limited → pneumothorax, pleural effusion, mass, collapsed lung
if unilateral bulging → obstruction if prolonged expiration + bulging on expiration → obstruction, mass, aneurysm, cardiomegaly |
|
|
|
What is a common complication of flail chest?
|
pneumothorax
|
|
|
|
What is the ddx for decreased tactile fremitus?
|
pneumothorax
pleural effusion/empyema pleural thickening asthma emphysema bronchial obstruction atelectasis pulmonary edema |
|
|
|
What is egophony?
|
patient says "EEEEE" and you hear "AAAAA" when
ascultating lungs present in pneumonia present above area of pleural effusion absent in pneumothorax |
|
|
|
What is the ddx for increased tactile fremitus?
|
consolidation → heavy bronchial secretions, pneumonia, mass
|
|
|
|
What sound is normal when percussing the lung fields?
|
resonance
|
|
|
|
Dullness/flatness to percussion of lung fields may indicate?
|
pleural effusion
pneumonia mass |
|
|
|
What are 5 indicators that chest pain probably does not originate in heart?
|
1. needle-like pain 1-2 seconds long
2. constant achiness 3. pain in shoulders or between shoulder blades 4. pain does not radiate 5. pain worsens when press precordium |
Mosbys
|
|
|
What is the ddx for diminished breath sounds?
|
splinting (shallow breathing due to pain)
hyperinflated lungs bronchi obstruction pleural effusion |
|
|
|
What is the ddx for heightened breath sounds?
|
consolidation
mass |
|
|
|
Define ventilation.
|
movement in and out of lungs
|
Interpreting Laboratory Data p191
|
|
|
Define perfusion.
|
movement of blood through lungs
|
Interpreting Laboratory Data p191
|
|
|
What body systems regulate homeostasis?
|
lungs and kidneys
|
Lab p179
|
|
|
Define cheyne-stokes respiration.
|

respiratory pattern characterized by alternating periods of crescendo-decrescendo hyperventilation and apnea
|
|
|
|
What is the ddx for tracheal deviation?
|
Contralateral Deviation:
pneumothorax pleural effusion mass hiatal hernia Ipsilateral Deviation: pulmonary fibrosis atelectasis lobectomy/pneumonectomy lung agenesis Anterior Deviation: mediastinitis Other: kyphoscoliosis (toward compressed lung) retrosternal thryoid thoracic aortic aneurysm (usually toward RT side) malignancy → thyroid, trachea, lungs, mediastinum |
|
|
|
Describe the pattern for percussion and auscultation of the lungs.
|
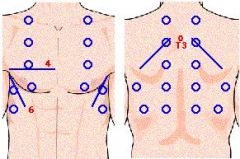
|
|
|
|
Define apnea.
|
absence of respirations
|
|
|
|
Define hypopnea.
|
abnormally slow or shallow respirations
|
|
|
|
Define hyperpnea AKA hyperventilation.
|
tachypnea + abnormally deep respirations
|
|
|
|
Define ataxic respirations.
|
disordered respirations characterized by varying rates and depths and may include periods of apnea
|
|
|
|
Ataxic respirations may indicate?
|
increased ICP, medulla damage, drug overdose
|
|
|
|
|
vesicular breath sounds
|
|
|
|
|
vesicular breath sounds
|
|
|
|
Define lingula.
|
tongue-like projection of the LUL
|
|
|
|
List the fissures of the lungs.
|
LT oblique fissure → divides LUL and LLL
RT horizontal fissure → divides RUL and RML RT oblique fissure → divides RML and RLL |
|
|
|
What is anterior and posterior to the trachea?
|
isthmus of thyroid lies anteriorly
esophagus lies posteriorly |
|
|
|
What is another name for the manubriosternal junction?
|
angle of Louis
|
Current p366
|
|
|
Define platypnea.
|
SOB when sitting upright that is relieved when lying down
|
Current p374
|
|
|
Define kussmaul respirations.
|
pattern of respiration characterized by rapid, deep, labored breaths
|
|
|
|
Kussmaul breathing is associated with?
|
metabolic acidosis
|
Current p375
|
|
|
What is the ddx for Cheyne-Stokes respirations?
|
may affect children and older adults during sleep
otherwise affects seriously ill → cerebral brain damage, drug-induced respiratory compromise |
Current p375
|
|
|
Define biot respiration.
|
irregular respirations varying in depth and interspersed with periods of apnea
(less severe that ataxic respiration) |
Current p375
|
|
|
What is the ddx for biot respiration?
|
severe and persistent increased ICP
medulla brain damage drug-induced respiratory compromise |
Current p375
|
|
|
Compare signs of airway obstruction above and below glottis.
|
Above glottis:
stridor quieter hot potato voice no cough swallowing more difficult head may be positioned awkwardly to presevere airway (extended with retropharyngeal abscess; head to affected side with peritonsillar abscess) Below glottis: stridor louder voice is hoarse barking cough positioning of head not a factor |
Current p377
|
|
|
Retractions may indicate?
|
respiratory distress
if unilateral + no suprasternal notch involvement → foreign body in bronchi if lower chest → asthma, bronchiolitis |
Mosbys p377
|
|
|
What is normal diaphragmatic excursion?
|
3-6cm
|
|
|
|
|
coarse crackles
|
|
|
|
|
bronchovesicular breath sounds
|
|
|
|
Where are bronchovesicular breath sounds heard?
|
over main bronchi → adjacent to sternum, posterior RT lung field
|
Mosbys p384
|
|
|
Where are bronchial breath sounds heard?
|
over trachea
|
Mosbys p385
|
|
|
Where are vesicular breath sounds heard?
|
over lesser bronchi, bronchioles, and lobes
(i.e. everywhere except trachea and main bronchi) |
Mosbys p385
|
|
|
Bronchial breath sounds over lung fields that are normally vesicular may indicate?
|
consolidation
|
Current p386
|
|
|
Which types of adventitious breath sounds are continuous?
|
wheezes
rhonchi |
Current p387
|
|
|
Which types of adventitious breath sounds are discontinous?
|
crackles
|
Current p387
|
|
|
Bronchial breath sounds over lung fields that are normally vesicular may indicate?
|
consolidation
|
Current p386
|
|
|
Increased vocal resonance (bronchophony, whispered pectoriloquy, egophony) indicates?
|
consolidation
|
Mosbys p388
|
|
|
Decreased vocal resonance (bronchophonoy, whispered pectoriloquy, egophony) indicates?
|
respiratory obstruction → emphysema etc.
|
Mosbys p388
|
|
|
How do you distinguish rhonchi from crackles?
|
rhonchi tend to disappear after coughing whereas crackles do not
|
Mosbys p388
|
|
|
What is bronchiolitis?
|
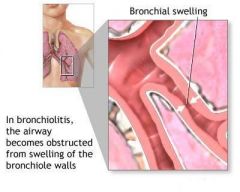
lower respiratory tract infection
inflammation of the bronchioles usually d/t viral infection |
|
|
|
Define dyspnea.
|
SOB; subjective difficulty in breathing
|
|
|
|
BRONCHIOLITIS:
|
ETIOLOGY:
lower respiratory tract infection characterized by inflammation of the bronchioles usually caused by RSV other causes include Parainfluenza, human metapneumovirus, influenza, adenovirus, Mycoplasma, Chlamydia, Ureaplasma, Bocavirus, and Pneumocystis usually affects children <2y/o most common serious acute respiratory illness in young children CLINICAL PRESENTATION: irritability, poor feeding, coughing, vomiting labored breathing, tachypnea, hypoxia prolonged expiration, wheezing, crackles usual course → 1-2 days fever, rhinorrhea, and cough followed by respiratory distress (nasal flaring, retractions, cyanosis), tachypnea (shallow and rapid), and wheezing DIAGNOSTIC WORKUP: CBC → may be normal or mild lymphocytosis CXR not indicated in children if temperature not elevated, no significant respiratory distress, or bilateral symmetrical findings on exam MANAGEMENT: 1. supportive care → fluids, humidifier, rest, no smoking near child 2. hospitalization indicated if: a. history of apnea b. marked respiratory distress with retractions c. moderate tachypnea with feeding difficulties d. hypoxemia on room air 3. hospital supportive care → frequent suctioning, fluids to maintain hydration, supplemental O2 if hypoxemia present 4. do not prescribe antibiotics unless evidence of associated bacterial pneumonia 5. do not prescribe bronchodilators or corticosteroids (have not been shown to change severity or duration of illness) 6. PREVENTION: proper handwashing reduce exposure to potential environmental risk factors → cigarette smoke, crowded conditions PATIENT EDUCATION: cigarette smoke makes a child more susceptible to infection |
|
|
|
Define orthopnea.
|
SOB while lying down that is relieved when upright
|
|
|
|
ASPIRATION OF FOREIGN BODY:
|
ETIOLOGY:
aspiration of foreign body into any part of respiratory tract history of running with food in mouth (seeds, peanuts, popcorn, hot dogs, hard candy) or playing with small coins or toys highest risk at 6 months to 4 years CLINICAL PRESENTATION: aspiration rarely observed abrupt onset of coughing, choking, or wheezing symptoms depend on location of obstruction (laryngospasm if above glottis) foreign body in upper respiratory tract: partial upper respiratory tract obstruction → ability to vocalize, drooling, stridor complete upper respiratory tract obstruction → acute onset of choking, inability to vocalize or cough, cyanosis with marked distress lower respiratory tract aspiration → abrupt onset of coughing, wheezing, or respiratory distress, asymmetrical decreased breath sounds, localized wheezing, chronic cough, persistent wheezing or recurrent pneumonia DIAGNOSTIC WORKUP: CXR → inspiratory and forced expiratory views, asymmetrical findings, 25% normal in setting of aspiration MANAGEMENT: if partial upper airway obstruction → initially allow child to use cough reflex to remove foreign body, intervene if does not resolved as brief observation if complete upper airway obstruction → intervene immediately 1. open airway, if foreign body is visualized carefully remove object, do not perform blind sweeps of mouth 2. if <1 y/o → place infant face down over rescuer’s arm with head positioned below trunk, deliver 5 rapid blows between scapulae with heel of hand, if obstruction persists roll child over and deliver 5 rapid chest compressions, repeat sequence until obstruction relieved 3. if >1 y/o → perform Heimlich maneuver with special care to prevent abdominal organ injury 4. if persistent inadequate ventilation → tracheotomy, cricothyrotomy, or intubation depending on skill and setting if lower airway aspiration → hosptitalization, bronchoscopy for removal of foreign body, nebulizer treatments and chest physiotherapy to treat bronchospasm and clear mucus PREVENTION: teach children not to run with food in mouth or swallow small objects teach older children not to give certain foods to younger children PATIENT EDUCATION: |
|
|
|
Define paroxysmal nocturnal dyspnea (PND).
|
sudden waking at night with SOB
|
|
|
|
RESPIRATORY SYNCYTIAL VIRUS:
|
ETIOLOGY:
RSV causes 70% of bronchiolitis and 40% of pneumonia in young children CLINICAL PRESENTATION: epidemics in late fall to early spring (January–February peak) upper respiratory symptoms (low-grade fever for 2-4 days, cough, difficulty feeding) followed by tachypnea and diffuse wheezing for 3-7 days hyperinflation, retractions, prolonged expiration, wheezing, crackles may manifest with apnea complicated by otitis media, bacterial pneumonia DIAGNOSTIC WORKUP: RSV antigen in nasal or pulmonary secretions (fluorescent antibody or ELISA) CXR → diffuse hyperinflation, peribronchiolar thickening, +/- patchy infiltrates and atelectasis MANAGEMENT: outpatient: self-limiting hospitalization: 1. hospitalize if respiratory distress prevents feeding, hypoxia 2. tube or IV feedings 3. supplemental O2 4. trial of bronchodilator therapy, d/c if no improvement 5. corticosteroids and ribavirin controversial PREVENTION: proper handwashing respiratory isolation during peak season RSV monoclonal antibody IM monthly during peak season in high-risk children PATIENT EDUCATION: 90% of children infected by age 2 years reinfection common but generally only causes upper respiratory symptoms may increase risk of asthma later in life |
|
|
|
Define hemoptysis.
|
coughing up blood
|
|
|
|
What is Sudden Infant Death Syndrome (SIDS)?
|
sudden death of an infant <1y/o without explanation despite a thorough case investigation (autospy, examination of death scene, review of clinical history)
|
|
|
|
Define eupnea.
|
normal respiratory rate
12-20 respirations/minute |
|
|
|
SUDDEN INFANT DEATH SYNDROME:
|
ETIOLOGY:
sudden death of infant <1y/o without explanation diagnosis of exclusion after thorough case investigation (autopsy, examination of death scene, review of clinical history) affects <1:1000 infants, affects male:female 3:2, usually occurs between few weeks and 6 m/o, peak at 2-4 m/o risk factors include mothers who are racial minorities, teenagers, drug-addicted, low SES, smokers; FH of SIDS; low birth weight; prone sleeping position CLINICAL PRESENTATION: history of mild upper respiratory infection symptoms before death death usually occurs between midnight and 8am while sleeping DIAGNOSTIC WORKUP: autopsy examination of death scene MANAGEMENT: counseling and support groups → The National SIDS Resource Center (http://www.sidscenter.org) PREVENTION & PATIENT EDUCATION: do not smoke when pregnant place infant on back to sleep firm sleep surface pacifier use during nap or bedtime avoid overheating quit smoking educate family members, friends, and childcare providers on proper sleep position recent immunizations do not increase risk |
|
|
|
Define bradypnea.
|
abnormally slow respiratory rate
<12 respirations/minute |
|
|
|
What is the etiology of CF?
|
autosomal recessive genetic disorder → abnormalities in cell membrane chloride channels → causing exocrine glands to produce abnormal mucus → causing obstruction of glands and ducts → causing glandular dilation and tissue damage
abnormalities occur in respiratory, GI, and male reproductive systems affects 1:3200 (1:25 is carrier) most common cause of severe lung disease in young adults most common fatal hereditary disorder in whites in U.S. |
|
|
|
Define tachypnea.
|
abnormally fast respiratory rate
>20 respirations/minute |
|
|
|
What is the clinical presentation of CF?
|
meconium ileus at birth virtually diagnostic of CF
failure to thrive chronic or recurrent productive cough chronic or recurrent respiratory infections (sinusitis, bronchitis, pneumonia) purulent rhinorrhea, nasal polyps dyspnea, exercise intolerance hemoptysis bulky greasy malodorous stools and steatorrhea (d/t pancreatic insufficiency) increased AP diameter hyperresonance wheezing apical crackles clubbing also consider CF if severe dehydration + hypochloremic alkalosis, unexplained bronchiectasis, cirrhosis, or pancreatitis, rectal prolapse |
|
|
|
What is the ddx for hyperresonance?
|
pneumothorax
COPD acute asthma attack pleural effusion (if percuss superior to effusion) |
|
|
|
What is the diagnostic workup of CF?
|
nutritional deficiencies → hypoproteinemia, anemia, fat-soluble vitamin deficiencies
CXR → hyperinflation, mucus plugging, bronchiectasis, focal atelectasis, pnuemothorax PFTs → mixed obstruction and restriction; reduced FVC, airflow rates, TLC, air trapping, reduced diffusing capacity chloride sweat test → >60 mEg/L on two occasions genotyping → CF gene mutation positive NBS should be confirmed with chloride sweat test or genotyping false-negative NBS can occur |
|
|
|
Define adventitious breath sounds.
|
abnormal sounds heard over normal breath sounds
|
|
|
|
What is the management of CF?
|
1. refer to CF center
2. high calorie, protein, fat, and salt diet 3. daily multivitamin 4. pancreatic enzyme supplement prior to eating 5. clear lower airway secretions via manual chest compressions etc. 6. treat active airway infections via antibiotics 7. inhaled bronchodilators 8. influenza and pneumococcal immunizations 9. lung transplant if end-stage lung disease 10. screen family members 11. genetic counseling and support groups |
|
|
|
What are examples of normal breath sounds?
|
bronchial
vesicular |
|
|
|
What is the prevention of CF?
|
none → genetic disorder
|
|
|
|
What are examples of adventitious breath sounds?
|
stridor
wheezes (rhonchi) crackles (rales) pleural friction rubs |
|
|
|
What is the prognosis for CF?
|
median survival age is >35y/o
death occurs from pulmonary complications (pneumonia, pneumothorax, hemoptysis), chronic respiratory failure, or cor pulmonale |
|
|
|
Define digital clubbing.
|
enlargement of terminal phalanges of fingers and/or toes
|
|
|
|
APNEA:
|
ETIOLOGY:
unexplained breathing cessation for ≥20 seconds or shorter period of breathing cessation associated with bradycardia, pallor, cyanosis, or hypotonia central apnea: characterized by respiratory cessation 2° to diminished muscular activation occurs in newborns (especially preterm infants) d/t infection, metabolic abnormalities, anemia, hypoxia, CNS injury obstructive apnea: characterized by cessation of airflow despite respiratory effort (movement of chest wall and abdomen present) occurs in later infancy and childhood d/t obstructive upper airway conditions (tonsillitis, laryngitis, laryngomalacia, masses) CLINICAL PRESENTATION: breathing cessation DIAGNOSTIC WORKUP: central apnea → CBCDP, BMP, ionized calcium, magnesium, BC, UAC, URNC, toxicology studies; CT if abnormal mental status, bulging fontanelle, focal neurological sxs; LP if lethargic or toxic-appearing obstructive apnea → CXR, laternal neck radiograph, sleep study MANAGEMENT: hospitalization for observation and full workup pulse oximeter and apnea monitor supplemental O2 IV fluids if dehydrated |
|
|
|
True or false, asthma and emphysema are associated with clubbing?
|
FALSE
|
|
|
|
What disorders comprise croup syndrome?
|
laryngotracheal bronchitis
epiglottitis bacterial tracheitis |
|
|
|
What is the ddx for bradypnea?
|
obesity
metabolic alkalosis cerebrum lesion narcotic overdose |
|
|
|
What is the ddx for acute stridor?
|
laryngeal or esophageal foreign body
croup → laryngotracheobronchitis, epiglottitis, bacterial tracheitis spasmodic croup retropharyngeal abscess angioedema |
|
|
|
What is the ddx for tachypnea?
|
hypoxemia
metabolic acidosis pons lesion splinting aspirin overdose anxiety |
|
|
|
What is croup?
|
group of disorders characterized by acute inflammation of the larynx
|
|
|
|
What is the ddx for PND?
|
RESPIRATORY:
COPD cor pulmonale NON-RESPIRATORY: obesity snoring sleep apnea cardiomyopathy valvular disease HF → pulmonary edema panic disorder |
|
|
|
Laryngotracheal Bronchitis (AKA viral croup)
|
usually caused by parainfluenza viruses
also caused by RSV, human metapneumovirus, influenza virus, rubeola virus, adenovirus, and Mycoplasma pneumoniae usually affects younger children in fall and early winter edema in subglottic space results in signs of upper airway obstruction, though inflammation of entire airway is usually present prodrome of upper respiratory tract symptoms barking cough stridor usually no fever no drooling lateral neck radiograph treatment based on symptoms mild croup = barking cough, no stridor at rest → supportive therapy with oral hydration severe croup = barking cough, stridor at rest → supplemental O2, nebulized racemic epinephrine, dexamethasone (corticosteroid), recurrent nebulized racemic epinephrine if respiratory distress persists, intubation if impending respiratory failure most children improve within few days |
|
|
|
What is the ddx for orthopnea?
|
RESPIRATORY:
bronchitis pneumonia asthma COPD pulmonary HTN cor pulmonale NON-RESPIRATORY: obesity snoring sleep apnea GERD superior vena cava syndrome cardiomyopathy valvular disorders HF → pulmonary edema polycystic liver disease panic disorder |
|
|
|
EPIGLOTTITIS:
|
usually d/t Haemophilus influenzae in unimmunized children, nontypeable Haemophilus influenza, Neisseria meningitides, or Streptococcus
sudden onset of high fever, dysphagia, drooling, muffled voice cyanosis, inspiratory retractions, soft stridor sitting-dog position (provides best airway) lateral neck radiographs reveal “thumbprint” sign swollen cherry red epiglottis and swollen arytenoids management: 1. immediate intubation in children once diagnosis established 2. BC 3. epiglottis culture 4. IV antibiotics covering Haemophilus influenza and Streptococcus → cefriaxone x 2-3 days 5. oral antibiotics x 7 days 6. extubation within 24-48 hours if reduction in swelling |
|
|
|
What should you ask a patient who complains of orthopnea?
|
how many pillows do you use to relieve your orthopnea?
can be documented as 1, pillow orthopena, 2, pillow orthopena, 3 pillow orthopnea and so on. |
|
|
|
What is the most common cause of cor pulmonale?
|
COPD
|
|
|
|
What is the ddx for hemoptysis?
|
PULMONARY:
secondary to chronic cough bronchitis pneumonia TB PE lung neoplasm NON-RESPIRATORY: mitral stenosis HF |
|
|
|
Define cyanosis.
|
blue discoloration of skin or mucous membranes due to deficient oxygenation of blood
*must be 5g of reduced hemoglobin per 100mL of blood for presentation |
|
|
|
Define pulsus paradoxus.
|
pulse weaker during inspiration and stronger during expiration
|
|
|
|
List common signs and symptoms of a pulmonary disorder.
|
dyspnea
orthopnea paroxysmal nocturnal dyspnea cough hemoptysis pleuritic chest pain hemoptysis tachycardia pulsus paradoxus hyperpnea hyperventilation hyperresonance adventitious breath sounds stridor wheezing cyanosis clubbing hypoxemia |
|
|
|
Define hyperpnea.
|
breathing that is faster or deeper than normal
occurs after exercise or in response to low O2 |
|
|
|
Define hyperventilation.
|
rapid deep breathing that results in abnormal CO2 loss
|
|
|
|
Define pleuritic chest pain.
|
chest pain that occurs or worsens synchronously with the respiratory cycle
|
|
|
|
Define hyperresonance.
|
abnormally increased resonance on percussion of the lungs, often lower in pitch
|
|
|
|
Define hypoxemia.
|
abnormally low pO2
|
|
|
|
Define hypoxia.
|
either tissue or body deprived of adequate O2
|
|
|
|
What is the ddx for clubbing?
|
CF
chronic fibrotic changes within the lung chronic cyanosis of congenital heart disease |
Mosbys p377
|
|
|
Define wheezing.
|
adventitious breath sound; whistling, musical, squeaking, or puffing sound that occurs during expiration
|
|
|
|
Define stridor.
|
adventitious breath sound; high-pitched, noisy respiratory like blowing of the wind; sign of respiratory obstruction
|
|
|
|
Define empyema.
|
pus accumulation within naturally existing cavity
|
|
|
|
Define abscess.
|
pus accumulation within newly formed cavity
|
|
|
|
List signs of upper airway obstruction.
|
nasal flaring
retraction at suprasternal notch inspiratory stridor hoarse cough or cry If severe: cyanosis retractions also involving intercostal and subcostal spaces barking cough inspiratory and expiratory stridor |
Current p377
|
|
|
|
mild stridor
|
|
|
|
|
severe stridor
|
|
|
|
What is the ddx for stridor?
|
airway obstruction →
foreign body aspiration narrowing due to trauma, allergic reaction, infection or neoplasm inhalation of caustic agent |
|
|
|
What is the ddx for pleuritic chest pain?
|
trauma → blunt or penetrating chest wall trauma, chest wall fracture, thorax or back muscle strain/sprain, pneumothorax
infection → pleural effusion, pleuritis, pneumonia, pulmonary TB malignancy spleen injury |
|
|
|
What are the differences between chronic OBSTRUCTIVE pulmonary disease and chronic RESTRICTIVE pulmonary disease?
|
chronic obstructive pulmonary disease
-difficulty in getting air out -caused by: 1. mechanical obstruction → foreign body, mucus plug of chronic bronchitis, tumor 2. increased resistance of airways → inflammation of chronic bronchitis 3. increased tendency for bronchoconstriction → asthma, emphysema chronic restrictive lung disease -difficult to get air in -caused by: 1. stiff lungs → interstitial lung disease 2. stiff chest wall → obesity, kyphoscoliosis, ankylosing spondylitis 3. respiratory muscle weakness → neurological or neuromuscular diseae |
|
|
|
List chronic obstructive pulmonary diseases and chronic restrictive pulmonary diseases.
|
Chronic Obstructive Pulmonary Diseases:
1. asthma 2. COPD → chronic bronchitis, emphysema 3. CF 4. bronchiectasis Chronic Restrictive Pulmonary Diseases: 1. stiff lungs → interstitial fibrosis -idiopathic -connective tissue disorder → RA, SLE, scleroderma, myositis -environmental → pneumoconiosis, asbestosis, silicosis, hypersensitivity pneumonitis -drugs 2. stiff chest wall -obesity -kyphoscoliosis -ankylosing spondylitis 3. respiratory muscle weakness -spinal cord injury -Guillain-Barre -MS -ALS -muscular dystrophies -myasthenia gravis |
|
|
|
What is the pathophysiology of restrictive lung disease?
|
if due to stiff lungs:
alveolar walls become thin and inflexible → alveoli contract more quickly and forcefully and are less likely to collapse → decreases residual volume |
|
|
|
What is the Patient Outcome Research Team (PORT) Score?
|
scoring system used to predict severity of adult community acquired pneumonia and thus determine appropriate treatment
|
|
|
|
What is included in the PORT score?
|
Age? (1 point per year)
Female? (-10) Nursing home resident? (+10) History of neoplasm? (+30) CHF? (+10) Liver disease? (+20) Kidney disease? (+10) Cerebrovascular disease? (+10) Altered mental status? (+20) systolic BP <90? (+20) HR >124? (+10) RR >29? (+20) temp <95 or >103.8? (+15) Hct <30? (+10) Na+ <130? (+20) GLUC >249 (+10) BUN >29? (+20) pH <7.35? (+30) PO2 <60 (+10) pleural effusion on CXR? (+10) |
|
|
|
What is the clinical usefulness of the PORT score?
|
can determine mortality rate of adult patient with community acquired pneumonia and if this patient should be admitted or not
|
|
|
|
Describe the recommendations for the influenza vaccine.
|
1. includes H1N1
2. get if >6 m/o 3. get yearly during flu season 4. get especially if high risk for developing flu complications or spreading flu: -children <5y/o -pregant women -adults >50y/o -nursing home residents -chronic medical conditions -household contacts of at-risk persons -caregivers -healthcare workers |
CDC
|
|
|
Describe the recommendations for the pneumococcal vaccine.
|
PVC13 vaccine:
get 4-dose series at 2, 4, 6, and 12 months get 1 dose if didn't get 4-dose series and 2-5y/o PPSV vaccine: get if >65 y/o get if nursing home resident if 2-64 y/o → get if chronic medical problem or immunosuppresion if 19-64 y/o → get if smoke or have asthma |
CDC
|
|
|
Describe the recommendations for the haemophilus influenzae type (hib) vaccine.
|
prevents epiglottitis, pneumonia, meningitis,etc.
get 4-dose series at 2, 4, 6, and 12 months |
CDC
|
|
|
What are the 5 A's of smoking cessation?
|
1. ask → identify tobacco users
2. advise → urge to quit 3. assess → determine willingness to quit within next 30 days 4. assist → aid in quitting → set quit date, tell family/friends, remove products from environment 5. arrange → follow-up on progress |
|
|
|
How much pleural fluid is normally found in the pleural cavity?
|
5-15mL
|
|
|
|
Define pleuritis.
|
pain caused by inflammation of the pleura
|
|
|
|
What does a pleural friction rub indicate?
|
pleuritis
|
|
|
|
Describe a pleural friction rub.
|
coarse grating sound
usually heard on inspiration indicative of pleuritis |
|
|
|
What is another name for pleuritis?
|
pleurisy
|
|
|
|
What is the etiology of pleuritis?
|
irritation of the parietal pleura
if young and otherwise healthy → viral respiratory infections, pneumonia rib fracture pneumothorax pleural effusion |
Current ch9
|
|
|
What is the clinical presentation of pleuritis?
|
pain → localized, sharp, fleeting; aggravated by breathing, coughing, sneezing, moving; may refer to ipsilateral shoulder if central portion of diaphragmatic parietal pleura irritated
pleural friction rub |
Current ch9
|
|
|
What is the management of pleuritis?
|
1. treat underlying disease
2. for pain relief → NSAIDs → indomethacin 25mg PO 2-3x daily 3. for cough relief → codeine 30-60mg PO q8hr (only if retention of airway secretions unlikely to cause complications) |
Current ch9
|
|
|
Define pleural effusion.
|
abnormal accumulation of fluid in pleural space
|
|
|
|
Define parapneumonic effusion.
|
pleural effusion associated with pneumonia
|
|
|
|
Define empyema.
|
pus accumulation within naturally existing cavity
|
|
|
|
Define hemothorax.
|
blood in pleural space
|
|
|
|
Define pneumothorax.
|
air in pleural space
|
|
|
|
What is the pathophysiology of pleural effusion?
|
transudate – ↑ production due to ↑ hydrostatic pressure or ↓ colloid osmotic pressure; due to systemic factors that alter formation and absorption of pleural fluid
exudate – ↑ production due to abnormal capillary permeability or ↓ lymphatic drainage; due to local factors that alter formation and absorption of pleural fluid |
|
|
|
Define transudate.
|
any fluid that passes through a membrane wall due to ↑ hydrostatic pressure or ↓ colloid osmotic pressure
|
|
|
|
Define exudate.
|
any fluid that is exuded out of a tissue or its capillaries due to inflammation, infection, or malignancy
|
|
|
|
Define pyothorax (pleural empyema).
|
pus in pleural space
|
|
|
|
What is a tension pneumothorax?
|
pneumothorax where air enters pleural space but cannot exit → can lead to lung collapse and compression of mediastinal structures which can be fatal
|
|
|
|
What is the etiology of a pneumothorax?
|
air enters pleural space:
1. spontaneous → rupture of an alveolus ○ primary if idiopathic → commonly occurs in 10-30 y/o tall thin males; risk increased if smoker or positive FH ○ secondary if associated with underlying lung disease → occurs as complication of CF, asthma, COPD, interstitial lung disease, Pneumocystis pneumonia, TB 2. trauma → blunt or penetrating chest wound, rib fracture 3. iatrogenic → thoracentesis, lung biopsy, central line placement, mechanical ventilation *tension pneumothorax often due to penetrating trauma, lung infection, CPR, or mechanical ventilation |
|
|
|
What is the clinical presentation of a pneumothorax?
|
• acute onset of dyspnea and chest pain
• symptoms begin during rest and often resolve after 24 hours even if pneumothorax persists • if pneumothorax small, findings are minimal except for mild tachycardia • if pneumothorax large, findings include cyanosis, unilateral chest expansion, decreased tactile fremitus, hyperresonance, and diminished breath sounds on affected side • suspect tension pneumothorax if marked tachycardia, hypotension, tracheal/mediastinal shift, or absent breath sounds on affected side • if associated with asthma or COPD, may present with life-threatening respiratory failure |
|
|
|
What is the diagnostic workup of a pneumothorax?
|
• CXR reveals visceral pleural line; may only be seen on expiratory view
• if tension pneumothorax, CXR reveals large amount of air on affected side and contralateral shift of mediastinum • if suspected tension pneumothorax, do not delay treatment waiting for CXR results |
|
|
|
What is the general management of a pneumothorax?
|
• treatment depends on severity of pneumothorax and underlying disease
• if primary + small + stable pneumothorax – observation; will often resolve spontaneously • if secondary pneumothorax, large pneumothorax, tension pneumothorax, associated with severe symptoms, or due to mechanical ventilation – place chest tube, order serial CXR every 24 hours, and provide symptomatic relief • if bilateral pneumothorax, refractory to treatment, or recurrence – surgery • encourage smoking cessation – 50% risk of recurrence if smoking continued • avoid exposure to high altitudes, flying in unpressurized aircrafts, scuba diving • spontaneous pneumothorax has 30% recurrence rate |
|
|
|
What is a parapneumonic effusion?
|
exudative pleural effusion associated with pneumonia
|
|
|
|
What are the different types of parapneumonic effusion?
|
○ simple parapneumonic effusion = modest-sized exudate, sterile, free-flowing
○ empyema = pus in pleural space ○ complicated parapneumonic effusion = large-sized exudate, inflammatory or loculated |
|
|
|
What is the etiology of a parapneumonic effusion?
|
bacterial pneumonia
|
|
|
|
What is the clinical presentation of a parapneumonic effusion?
|
• fever, cough, dyspnea, pleuritic chest pain
• decreased fremitus, dullness to percussion, decreased breath sounds |
|
|
|
What is the diagnostic workup of a parapneumonic effusion?
|
• CXR – order PA and lateral decubitus views
• PA view reveals meniscus-like opacity (though not if large effusion) • lateral decubitus view reveals flattening of opacity (though not if loculated) • thoracentesis and pleural fluid analysis – order cell count/diff, glucose, LDH, pH, gram stain, culture • empyema indicated by positive gram stain or culture • complicated parapneumonic indicated by frank pus, glucose <20 mg/dL, pH <7.20, LDH >1000 units/mL, positive gram stain or culture, or loculation |
|
|
|
What is the general management of a parapneumonic effusion?
|
• if simple effusion – prescribe antibiotics; no drainage needed
• if empyema – prescribe antibiotics; place chest tube and drain • if complicated effusion – prescribe antibiotics; place chest tube and drain ideally before loculation occurs • if loculation – place chest tube with VATS or CT guidance; intrapleural injection of fibrinolytic agents may improve drainage but use is controversial |
|
|
|
What is the etiology of a hemothorax?
|
most commonly caused by blunt or penetrating chest trauma
non-traumatic and iatrogenic causes uncommon |
|
|
|
What is the clinical presentation of a hemothorax?
|
symptoms similar to pleural effusion
dyspnea chest pain decreased fremitus dullness to percussion decreased breath sounds |
|
|
|
What is the diagnostic workup of a hemothorax?
|
CXR → pleural effusion
*<25% of traumatic hemothoraces do not show up on initial CXR → repeat in 3-6 hours and make sure patient is sitting (not supine) *62-83% have concurrent pneumothorax thoracentesis/pleural fluid analysis → hct >50% of that of peripheral blood |
|
|
|
What is the general management of a hemothorax?
|
1. place chest tube with large bore tube to minimize clotting within tube → drain blood
2. quantify and monitor bleeding 3. if bleeding >200mL/hr without diminishing → surgical evacuation of blood via VATS 4. timeliness is essential to prevent fibrothorax |
|
|
|
What is the etiology of sarcoidosis?
|
unknown
|
|
|
|
What is sarcoidosis?
|
systemic inflammatory disorder of unknown etiology characterized most often by granulomatous inflammation of the lung
|
|
|
|
What is the clinical presentation of sarcoidosis?
|
insidious onset of fatigue, fever, and dyspnea
other systems involved include skin, eyes, heart, liver, kidney, and peripheral nerves erythema nodosum iritis arthritis peripheral neuropathy may be asymptomatic and found on CXR → bilateral hilar and RT paratracheal lymphadenopathy |
|
|
|
What is the diagnostic workup of sarcoidosis?
|
CBC → leukopenia
↑ ESR hypercalcemia hypercalciuria ↑ ACE PFTs → restrictive lung changes with decreased lung volume and diffusing capacity CXR: stage 1 → bilateral hilar adenopathy stage 2 → hilar adenopathy + parenchymal involvement stage 3 → parenchymal involvement → usually diffuse reticular infiltrates diagnosis requires biopsy → noncaseating granulomas + exclusion of other granulomatous disorders |
|
|
|
What is the general management of sarcoidosis?
|
1. oral prednisone usually for months to years if:
-disabling constitutional symptoms -cutaneous lesions -iritis -uveitis -cardiac involvement -progressive pulmonary lesions -granulomatous hepatitis -arthritis -CNS involvement -hypercalcemia |
|
|
|
What is the pathophysiology of interstitial lung disease?
|
injury to alveoli epithelium or capillary endothelium → obliteration of alveolar capillaries → reorganization of lung parenchyma → fibrosis
|
|
|
|
What is the clinical presentation of interstitial lung disease?
|
insidious onset of progressive dyspnea
chronic dry cough tachypnea bilateral basilar dry crackles Right HF clubbing hypoxemia with exercise |
|
|
|
What is the diagnostic workup of interstitial lung disease?
|
PFTs → restrictive changes → reduced lung volumes, diffusing capacity, 6min walk distance
CXR → reduced lung volumes patchy distribution of ground glass, reticular, nodular, and cystic opacities |
|
|
|
What is the clinical presentation of idiopathic pulmonary fibrosis (usual interstitial pneumonia)?
|
inspiratory crackles
|
|
|
|
What is the diagnostic workup of idiopathic pulmonary fibrosis (usual interstitial pneumonia)?
|
PFTs → restrictive changes
CXR → diffuse patchy fibrosis; progressive over several years CT → pleural-based honeycombing |
|
|
|
What is the general management of idiopathic pulmonary fibrosis (usual interstitial pneumonia)?
|
Controversial!
Prednisone NOT recommended for UIP |
|
|
|
What is the clinical presentation of pulmonary vasculitis (Wegener Granulomatosis)?
|
triad of upper respiratory tract disease + lower respiratory tract disease + glomerulonephritis
vasculitis of small arteries, arterioles, and capillaries necrotizing granulomatous lesions of upper and lower respiratory tract glomerulonephritis suspect if refractory nasal congestion or sinusitus upper respiratory tract → otitis media, nasal congestion, sinusitis, gingivits, mastoiditis, stridor due to subglottic stenosis lower respiratory tract → dyspnea, cough, hemoptysis |
|
|
|
What is the diagnostic workup of pulmonary vasculitis (Wegener Granulomatosis)?
|
ANCA
biopsy CXR/CT |
|
|
|
What is the general management of pulmonary vasculitis (Wegener Granulomatosis)?
|
prednisone
cyclophosphamide |
|
|
|
What is the clinical presentation of pulmonary vasculitis (Churg-Strauss)?
|
vasculitis of small and medium arteries that occurs in asthma patients
often involves skin and lungs may also involve paranasal sinuses, heart, liver, GI, peripheral nerves |
|
|
|
What is the diagnostic workup of pulmonary vasculitis (Churg-Strauss)?
|
CBC → eosinophil count → >1500 cells/mcL or >10% of WBCs
CXR → transient opacities, mutiple nodules biopsy |
|
|
|
What is the general management of pulmonary vasculitis (Churg-Strauss)?
|
prednisone and cyclophosphamide
|
|
|
|
What is bronchiectasis?
|
permanent abnormal dilation and destruction of bronchial walls
|
|
|
|
What is the most common cause of bronchiectasis?
|
CF
|
|
|
|
What is the ddx for barrel chest?
|
CF, asthma, emphysema
|
|
|
|
What is the normal ratio of AP and tranverse chest diameter?
|

1:2
|
|
|
|
What 3 criteria are assessed to determine asthma severity?
|
FEV1/FVC ratio
asthma symptoms medication use |
Interpreting Laboratory Data p194
|
|
|
What is status asthmaticus?
|
medical emergency in which asthma symptoms are refractory to bronchodilator therapy
|
|
|
|
What is the etiology of CF?
|
autosomal recessive genetic disorder → abnormalities in cell membrane chloride channels → causing exocrine glands to produce abnormal mucus → causing obstruction of glands and ducts → causing glandular dilation and tissue damage
affects 1:3200 (1:25 is carrier) most common cause of severe lung disease in young adults most common fatal hereditary disorder in whites in U.S. |
|
|
|
What is the clinical presentation of CF?
|
history of chronic or recurrent infections, pancreatitis, or infertility
dyspnea purulent rhinorrhea chronic or recurrent cough with sputum recurrent hemoptysis wheezing decreased exercise tolerance increased AP diameter hyperresonance apical crackles clubbing |
|
|
|
What is the diagnostic workup of CF?
|
CXR → hyperinflation, mucus plugging, bronchiectasis, focal atelectasis, pnuemothorax
PFTs → mixed obstruction and restriction; reduced FVC, airflow rates, TLC, air trapping, reduced diffusing capacity chloride sweat test → >60 mEg/L on two occasions genotyping → CF gene mutation |
|
|
|
What is the management of CF?
|
1. refer to CF center
2. clear lower airway secretions → manual chest percussion etc. 3. antibiotics → treat active airway infections 4. inhaled bronchodilators 5. influenza and pneumococcal immunizations 6. screening of family members 7. genetic counseling 8. lung transplant |
|
|
|
What is the prevention of CF?
|
none → genetic disorder
|
|
|
|
What is the prognosis for CF?
|
median survival age is >35y/o
death occurs from pulmonary complications (pneumonia, pneumothorax, hemoptysis), chronic respiratory failure, or cor pulmonale |
|
|
|
What is the etiology of bronchiectasis?
|
congenital or acquired
caused by recurrent inflammation or infection of airways → 50% caused by CF, other causes include abnormal lung defense mechanisms, localized airway obstruction, lung infection |
|
|
|
What is the clinical presentation of bronchiectasis?
|
chronic cough with sputum → copious, purulent, foul-smelling
dyspnea hemoptysis pleuritic chest pain wheezing weight loss anemia basilar crackles if severe → clubbing |
|
|
|
What is the diagnostic workup of bronchiectasis?
|
CXR →
dilated thickened bronchi → may appear as "tram-tracks" or ring-like markings scattered irregular opacities atelectasis focal consolidation CT is preferred diagnostic tool PFTs → obstructive dysfunction with hypoxemia |
|
|
|
What is the etiology of asthma?
|
genetic predisposition
risk factors include obesity and atopy (dust mites, dander, pollen) other precipitating factors include cold weather, exercise, URTI, GERD, stress affects 5% of population more common in male children and female adults |
|
|
|
What is the clinical presentation of asthma?
|
chronic or recurrent symptoms of airflow obstruction
airflow obstruction reversible → either sponatneously or with bronchodilator therapy dyspnea cough chest tightness prolonged expiration episodic wheezing symptoms often worse at night if allergic asthma → enalarged nasal mucosa, nasal secretions, nasal polyps, eczema, atopic dermatitis |
|
|
|
What is the diagnostic workup of asthma?
|
PFTs → measure before and after use of bronchodilator
*significant reversibility of airflow obstruction = ≥12% and 200mL in FEV1 and ≥15% and 200mL in FVC after inhaling SABA bronchoprovacation challenge → if PFTs non-diagnostic exercise challenge → if exercise-induced asthma suspected allergy testing GERD workup |
|
|
|
What is the prevention of asthma attacks?
|
1. develop asthma action plan
2. identify aggravating factors and reduce exposure 3. stop smoking |
|
|
|
What is an Asthma Action Plan?
|
plan develped between provider and patient to control asthma
-what medications to take daily -how to handle asthma long-term → what to avoid -how to handle asthma attacks → what additional medications to take, when to call provider or go to ER |
http://tiny.cc/AsthmaActionPlan
|
|
|
Does wheezing on forced expiration indicate airflow obstruction?
|
no, wheezing during normal breathing or prolonged expiration indicates obstruction
|
|
|
|
A reduced FEV1/FVC ratio indicates?
|
airflow obstruction
|
|
|
|
Describe the stepwise management of asthma.
|

|
|
|
|
Describe the classifications of asthma severity.
|

|
|
|
|
What is the etiology of COPD?
|
1. 80% due to smoking
3. 20% due to environmental exposure to tobacco smoke, dusts, chemicals, pollution; allergies, infection; hereditary factors 3. alpha-1-antitripsin deficiency |
|
|
|
What is the clinical presentation of COPD?
|
chronic cough with thick white sputum
dyspnea pursed lip breathing increased AP diameter hyperresonance prolonged expiration decreased breath sounds expiratory wheezing decreased heart sounds d/t hyperinflation of lungs acute exacerbation → anxious-appearing, tachypnea, accessory muscle use, cyanosis, wheezing, crackles advanced disease → pneumonia, pulmonary HTN, cor pulmonale, chronic respiratory failure |
|
|
|
What is the diagnostic workup of COPD?
|
PFTs → non-reversible obstructive changes → decreased FEV1/FVC, decreased FEV1, normal or decreased FVC, normal or increased RV, normal or increased TLC
CXR → hyperinflation, flattening of diaphragm sputum culture |
|
|
|
What is the management and patient education of COPD?
|
1. encourage smoking cessation
2. supplemental O2 3. bronchodilator for symptomatic relief → 1st-line is anticholinergic, SABA, or LABA, 2nd line is ICS, 4th line is theophylline 4. antibiotics if concomitant infection 5. pullmonary rehabilitation if severe dyspnea, reduced quality of life, or frequent hospitalizations despite medical treatment 4. influenza and pneumococcal immunizations |
|
|
|
What is the prevention of COPD?
|
do not smoke!
|
|
|
|
What is emphysema?
|
abnormal permanent enlargement of air spaces distal to terminal bronchioles
with destruction of their walls but without fibrosis |
|
|
|
Prolonged expiration indicates?
|
obstruction
|
|
|
|
What is COPD?
|
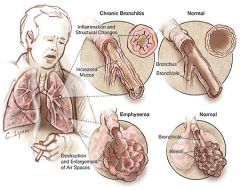
airflow obstruction due to chronic bronchitis or emphysema → usually mixed
|
|
|
|
What is chronic bronchitis?
|
excessive secretion of bronchial mucus → daily productive cough for ≥3 months in ≥2 consecutive years
|
|
|
|
What is the prognosis for COPD?
|
poor
degree of pulmonary dysfunction when first seen is important predictor of survivial FEV1 ≤1L = median survival of 4 years |
|
|
|
Which therapy methods reduce rate of decline in COPD?
|
Reduce rate of decline:
smoking cessation supplemental O2 pulmonary rehabilitation DO NOT reduce rate of decline: bronchodilators |
|
|
|
Discuss acute bronchitis vs chronic bronchitis.
|
ACUTE:
due to infection lasts few weeks CHRONIC: usually due to chronic smoke exposure also due to genetics, environmental exposures chronic cough for at least 3 months in 2 consecutive years productive cough |
|
|
|
What is another name for obesity hypoventilation syndrome?
|
Pickwickian syndrome
|
|
|
|
What is the etiology of obesity hypoventilation syndrome?
|
obesity → blunted ventilatory drive + increased mechanical load imposed upon chest
|
|
|
|
What is the clinical presentation of hypoventilation syndrome?
|
obesity
sleep apnea hypersomnolence chronic hypercapnea, hypoxemia, polycythemia, pulmonary HTN, RT HF |
|
|
|
What is the diagnostic workup of hypoventilation syndrome?
|
sleep studies
|
|
|
|
What is the management of obesity hypoventilation syndrome?
|
weight loss
smoking cessation eliminate sleep apnea NPPV (non-invasive positive pressure ventilation) respiratory stimulants → theophylline, acetazolamide, progesterone) |
|
|
|
What is acute respiratory failure?
|
respiratory dysfunction resulting in abnormalities in oxygenation or ventilation severe enough to threaten the function of vital organs
hypoxemia → dyspnea, restlessness, confusion, anxiety, delirium, HTN, tachycardia or bradycardia, tachypnea, cyanosis, tremor, arrhythmias hypercapnea → dyspnea, HA, impaired consciousness, HTN, tachycardia, tachypnea, hyperemia, papilledema, asterixis (wrist tremor) obtain ABG treat underlying disease ensure adequate ventilation → supplemental O2, NPPV, intubation, mechanical ventilation |
|
|
|
What is acute respiratory distress syndrome?
|
acute hypoxemic respiratory failure following systemic or pulmonary insult without evidence of heart failure
|
|
|
|
What is the etiology of pulmonary HTN?
|
idiopathic
secondary → lots of causes including any disease that causes chronic hypoxemia |
|
|
|
What is the clinical presentation of pulmonary HTN?
|
fatigue
dyspnea chest pain exertional syncope narrow spitting of S2 with loud pulmonic valve closure if advanced → RT ventricular hypertrophy, HF |
|
|
|
What is the diagnostic workup of pulmonary HTN?
|
PFTs → hypoxemia, increased wasted ventilation
EKG → RT ventricular hypertrophy, RT atrial hypertrophy CXR → enlarged central pulmonary arteries polycythemia if chronic hypoxemia |
|
|
|
What is the initial management of pulmonary HTN?
|
treat underlying disorder
phlebotomy if polycythemia anticoagulants if primary or secondary + high risk for PE |
|
|
|
What is the prognosis of pulmonary HTN?
|
dependent on underlying disease and severity when diagnosed
cor pulmonale = poor prognosis |
|
|
|
What is the etiology of cor pulmonale?
|
1. pulmonary disease + associated hypoxia → most commonly COPD
2. pulmonary HTN both result in right ventricular systolic and diastoic HF |
|
|
|
What is the clinical presentation of cor pulmonale?
|
dependent on underlying disease → often COPD symptoms
parasternal lift cyanosis clubbing elevated JVD dependent edema hepatomegaly ascites |
|
|
|
What is the diagnostic workup of cor pulmonale?
|
CXR → enlarged RT ventricle and pulmonary artery
EKG → tall peaked P waves, RT ventricular hypertrophy polycythemia |
|
|
|
What is the initial management of cor pulmonale?
|
1. treat underlying condition
2. supplemental O2 3. diuretics for edema 4. low salt diet |
|
|
|
What is the prognosis for cor pulmonale?
|
same as underlying disease if compensated
if congestive signs → 2-5 years unless uncomplicated emphysema |
|
|
|
What is the etiology of PE?
|
embolism → commonly thromboembolism caused by DVT
*PE occurs in 50-60% of DVTs risk factors: Virchow triad → venous stasis + injury to vessel wall + hypercoagulability venous stasis → immobility (bed rest, flying, polycythemia) injury to vessel wall → trauma, prior thrombosis, surgery hypercoagulability → oral contraceptives, FVL, protein S deficiency, protein C deficiency, AT3 deficiency, presence of ACL or lupus antibody |
|
|
|
What is the clinical presentation of PE?
|
dyspnea
hemoptysis chest pain syncope tachypnea |
|
|
|
What is the diagnostic workup of PE?
|
if low risk → DDQ → if positive → helical CT
if high risk → helical CT → if still unsure → venous ultrasonagraphy or pulmonary angiography VQ scan |
|
|
|
What is the initial management of PE?
|
1. initially heparin or LMWH
2. then warfarin x 6 months 3. warfarin duration dependent on clinical picture -6 months if reversible risk factor -12 months if idiopathic -6 months to indefinitely if non-reversible risk factor or recurrence thrombolytics may given but shown no difference in outcomes |
|
|
|
What is the prognosis of PE?
|
good if PE recognized and appropriately treated
50,000 deaths annually |
|
|
|
What is Virchow triad?
|
venous statis + injury to vessel wall + hypercoagulability
|
|
|
|
What are the clinical features of typical vs atypical pneumonia?
|
TYPICAL:
acute onset prostration high fever cough with sputum lobar consolidation ATYPICAL: insidious onset little to no fever cough without sputum hazy diffuse infiltrates (no signs of consolidation) |
|
|
|
What are the CDC guidelines for prevention of active TB in a patient with history of exposure or positive PPD?
|
1. most people with latent TB never develop active TB
2. certain populations with latent TB are at an increased risk for developing active TB -infected within last 2 years -young children -elderly -IV drug users -HIV+ -immunocompromised -people not correctly treated for TB in past 3. treatment can reduce risk of active TB by 90% 4. treatment consists of isoniazid x 9 months (longer if child or HIV+) 5. directly observed therapy recommended 6. prevention if exposure to active multi-drug resistant TB may not be an option |
http://tiny.cc/TBprevention
|
|
|
What is diagnostic workup of TB?
|
CXR →
small homogenous infiltrates → often apical hilar and paratracheal lymph node enlargement segmental atelectasis possible pleural effusion, cavitation miliary TB → diffuse small nodular densities → seen if hematogenous or lymphatic spread PPD 3 consecutive morning sputum samples AFB → not diagnostic of TB, may be positive with other mycobacteria bronchoscopy if suspicion but negative sputum pleural fluid analysis if associated pleural effusion biopsy → granulomatous inflammation |
|
|
|
Extrapulmonary TB is most common in what population?
|
HIV+ → who display lymphadenitis and miliary TB
|
|
|
|
PPD distinguises between latent and active TB, true or false?
|
false
|
|
|
|
How is interpretation of a PPD affected if previous BCG vaccination?
|
interpretation is the same as if no BCG vaccination received
|
|
|
|
IGRA can distinguish between latent and active TB, true or false?
|
true
|
|
|
|
What are the advantages of IGRA vs PPD?
|
IGRA
-requires single patient visit -results in 24 hours -distinguishes between latent and active TB -prior BCG does not cause false-pos -does not cause "boosting" |
|
|
|
What are the reporting requirements for TB?
|
report suspected and confirmed cases of TB to local health department within 1 day
|
http://www.oregon.gov/DHS/ph/tb/docs/investigativeguide.pdf
|
|
|
What is the clinical presentation of extrapulmonary TB?
|
vague symptoms
fatigue, intermittent fever, night sweats, weight loss, reduced appetite, pain/abscess most often affects kidneys and lymph nodes also affects bones, brain, abdominal cavity, pericardium, joints, and reproductive organs meningitis pericarditis |
|
|
|
Discuss community acquired pneumonia vs hospital acquired pneumonia.
|
CAP:
occurs outside hospital or within 48 hours of admission in patient who is ambulatory and did not reside in long-term care facility HAP: occurs in hopsital after 48 hours of admission excludes infections at time of admission common in patients requiring mechanical ventilation |
|
|
|
What are the risk factors for anaerobic pneumonia?
|
aspiration risk factors → unprotected airway (alcoholics, drug overdose, seizure disorders) + gingivitis
|
|
|
|
What are the complications of anaerobic pneumonia?
|
parapneumonic effusion
empyema abscess |
|
|
|
What are pneumoconioses?
|
chronic fibrotic lung diseases caused by inhalation of inorganic dusts (coal, silica, asbestos, others)
|
|
|
|
List diseases that fall under the category of pneumoconiosis.
|
coal miner's pneumoconiosis
silicosis asbestosis |
|
|
|
What is the etiology of coal worker's pneumoconiosis?
|
inhalation of coal dust (which contains silica and carbon)
associated with coal mining |
|
|
|
"Black lung" is another name for what disorder?
|
coal worker's pneumoconiosis
|
|
|
|
What is the pathophysiology of coal worker's pneumoconiosis?
|
inhalation of coal dust → coal dust ingested by alveolar macrophages → formation of coal macules
|
|
|
|
What is the clinical presentation of coal worker's pneumoconiosis?
|
1. if simple → asymptomatic, little to no pulmonary dysfunction, coal macules 1-2mm in diameter
2. if complicated → dyspnea, cough, pulmonary dysfunction, possible cor pulmonale, large black necrotic nodules >2 mm in diameter, extensive fibrosis |
|
|
|
What is the diagnostic workup of coal worker's pneumoconiosis?
|
PFTs → normal if simple; abnormal if complicated
CXR → diffuse small opacities, 1-2mm if simple, 2-5mm + fibrosis if complicated, more common in upper lung |
|
|
|
What is the initial management, patient education, and prevention of coal worker pneumoconiosis?
|
1. treatment is symptomatic
2. encourage job change within mine to reduce dust exposure 3. encourage smoking cessation (smoking has additive effect) 4. influenza and pneumococcal immunizations 4. serial CXRs to monitor progression 5. O2 as needed 6. consult with pulmonologist |
|
|
|
What is the prognosis for coal miner pneumoconiosis?
|
removal from job does not halt progression of disease once it progresses to massive pulmonary fibrosis
|
|
|
|
What is the etiology of silicosis?
|
inhalation of silica (found in rocks)
associated with: construction workers coal miners glassblowers sandblasters stonecutters quarry workers |
|
|
|
What is the pathophysiology of silicosis?
|
inhalation of silica → silica ingested by alveolar macrophages → inflammation → fibrosis
|
|
|
|
What is the clinical presentation of silicosis?
|
if simple → often asymptomatic, normal pulmonary function, often detected incidentally on CXR
if complicated → fatigue, weight loss, dyspnea, cough with sputum, tachypnea, prolonged expiration, wheezing, rhonchi, crackles, possible cor pulmonale, obstructive and restrictive pulmonary dysfuction, large conglomerate densities in upper lung |
|
|
|
What is the diagnostic workup of silicosis?
|
PFTS:
normal if simple restrictive and obstructive pulmonary dysfunction if complicated CXR: silicotic nodules throughout lung → small rounded opacities eggshell calcification → calcification of periphery of hilar lymph nodes |
|
|
|
Eggshell calcification on CXR indicates?
|
silicosis
|
|
|
|
What is the initial management, patient education, and prevention of silicosis?
|
1. treat symptoms
2. prevent further exposure 3. encourage smoking cessation 4. influenza and pneumococcal immunizations 5. PPD + current CXR (due to increased susceptibility to TB) 6. lung transplant 7. consult with pulmonologist |
|
|
|
What is the etiology of asbestosis?
|
long-term inhalation of asbestos fibers (typically 10-20 years)
associated with: construction workers shipyard workers pipefitters insulators |
|
|
|
What is the clinical presentation of asbestosis?
|
usually presents after 15 years
exertional dyspnea progressive dyspnea dry cough inspiratory crackles possible cyanosis and clubbing possible cor pulmonale |
|
|
|
What is the diagnostic workup of asbestosis?
|
PFTs
restrictive pulmonary dysfunction reduced diffusing capacity CXR: linear streaking at lung bases diffuse interstitial fibrosis → opacities of various shapes and sizes honeycombing if advanced *pleural calcification begins in lower lobes and subpleural areas CT best imaging method for asbestosis histology required for diagnosis → reveals asbestos bodies, ferruginous bodies |
|
|
|
What is the initial management, patient educaiton, and prevention of asbestosis?
|
1. treat symptoms
2. refer to smoking cessation clinic → risk of bronchogenic carcinoma increases 5-fold for asbestos workers 3. advise on work-related causation and report to state or federal agency 4. influenza and pneumococcal immunizations 5. prescribe O2 if needed 6. frequency of FUVs, PFTs, and CXRs dependent on severity and functional impairment 7. risk of malignant mesothelioma (cancer of pleura or peritoneum) 1000 x greater than general population |
|
|
|
What is the etiology of hypersensitivity pneumonitis?
|
inhalation of organic antigens → acute illness
associated with: farmers, pigeon breeders, office workers farmers lung → moldy hay humidifier lung → contaminated humidifier, heating systems, air conditioners pigeon-breeder's disease → bird serum and excrement moldy sugarcane, redwood sawdust, compost, cork dust detergent lung → enzyme additives rotting maple tree |
|
|
|
What is the clinical presentation of hypersensitivity pneumonitis?
|
acute onset of fatigue, fever, chills, dyspnea, and cough
nausea after 4-8 hours tachycardia, tachypnea, bilateral basilar crackles, possible cyanosis |
|
|
|
What is the diagnostic workup of hypersensitivity pneumonitis?
|
CBC → leukocytosis, shift to the left, antigens
PFTs → restrictive pulmonary dysfunction, reduced diffusing capacity CXR → small nodular densities sparing apices and bases |
|
|
|
What is the initial management, patient education, and prevention of hypersensitivity pneumonitis?
|
1. treated by identifying offending agent and avoiding further exposure
2. if severe or long duration → oral corticosteroids x 2 weeks |
|
|
|
What is the etiology of psittacosis?
|
recent contact (7-14 days) with bird infected with Chlamydophila psittaci
|
|
|
|
What is the clinical presentation of psitticosis?
|
exposure 1-2 weeks prior
fever, HA, chills, dry cough, myalgia atypical pneumonia → dullness to percussion, crackles possible endocarditis |
|
|
|
What is the diagnostic workup of psitticosis?
|
complement-fixing antibodies present after 2 weeks
CXR → interstitial and diffuse |
|
|
|
What is the management, patient education, and prevention of psitticosis?
|
tetracycline x 2-3 weeks
|
|
|
|
What is the most prevalent chronic occuptational lung disease worldwide?
|
silicosis
|
|
|
|
What is the etiology of histoplasmosis?
|
1. inhalation of fungal spores of histoplasma capsulatum by disturbing soil contaminated with bird or bat droppings
2. endemic areas include central and eastern U.S. → along river valleys → Ohio River and Mississippi River → 3. common in AIDs or immunocompromised patients |
Current ch36
|
|
|
What is the pathophysiology of histoplasmosis?
|
inhalation of fungus spores → spores convert to small budding cells → budding cells ingested by alveolar macrophages → organisms proliferate and spread hematogenously
|
Current ch36
|
|
|
What is the clinical presentation of histoplasmosis?
|
often asymptomatic and discoved incidentally on CXR
if mild → influenza-like infection x 1-4 days if severe → fever, cough, sternal chest pain x 5-15 days acute → prostration, fever, few pulmonary complaints disseminated → AIDs or immunocompromised patients, prostration, fever, dyspnea, cough, weight loss, oropharynx ulcers, hepatosplenomegaly |
Current ch36
|
|
|
What is the diagnostic workup of histoplasmosis?
|
serum or urine antigen
CXR → if acute, CXR usually normal |
Current ch36
|
|
|
What is the initial management, patient education, and prevention of histoplasmosis?
|
1. if asymptomatic or mild symptoms → no treatment
2. if prolonged symptoms → itraconazole 6-12 weeks 3. if severe symptoms → amphotericin B x 1-2 weeks then itraconazole x 1 year 4. monitor treatment with periodic CXRs 2. if AIDs patient → itraconazole prophylaxis for life |
Current ch36
|
|
|
What is another name for a solitary pulmonary nodule?
|
coin lesion
|
|
|
|
What is the clinical presentation of a solitary pulmonary nodule?
|
usually asymptomatic and detected incidentally on CXR or CT
|
|
|
|
What is the diagnostic workup of a solitary pulmonary nodule?
|
CXR →
isolated round marginated opacity <3 cm in diameter not associated with infiltrate, atelectasis, or adenopathy |
|
|
|
What is the initial management of a solitary pulmonary nodule?
|
1. order CT
2. determine if low, medium, or high risk of malignancy 3. if low risk → observe, order serial CXR every 3 months x 2 years, resect if grows 4. if medium risk → biopsy 5. if high risk → resect *management dependent on risk, contraindications to invasive procedures, and patient preference |
|
|
|
What is the etiology of a solitary pulmonary nodule?
|
95% are:
infectious → granuloma benign → hamartoma malignant → primary •Neoplastic (malignant or benign) ◦Bronchogenic carcinoma ■Adenocarcinoma (including bronchoalveolar carcinoma) ■Squamous cell carcinoma ■Large cell lung carcinoma ■Small cell lung cancer ◦Metastasis ◦Lymphoma ◦Carcinoid ◦Hamartoma ◦Connective-tissue and neural tumors - Fibroma, neurofibroma, blastoma, sarcoma •Inflammatory (infectious) ◦Granuloma - TB, histoplasmosis, coccidioidomycosis, blastomycosis, cryptococcosis, nocardiosis ◦Lung abscess ◦Round pneumonia ◦Hydatid cyst •Inflammatory (noninfectious) ◦Rheumatoid arthritis ◦Wegener granulomatosis ◦Sarcoidosis ◦Lipoid pneumonia •Congenital ◦Arteriovenous malformation ◦Sequestration ◦Bronchogenic cyst •Miscellaneous ◦Pulmonary infarct ◦Round atelectasis ◦Mucoid impaction ◦Progressive massive fibrosis |
|
|
|
How do you determine if low, medium, or high risk for malignancy for solitary pulmonary nodules?
|

Establish if benign or malignant:
1. risk factors -risk increases with age if >30y/o -risk increases with number of cigarettes smoked per day -risk increases with history of malignancy 2. size 2-5mm = 1% malignancy rate 6-10mm = 24% 11-20mm = 33% 21-45mm = 80% >80% lesions >5mm are malignant 3. margination -if smooth and well-defined, most likely benign -if lobular and ill-defined on CXR, most likely malignant -if spiculated (spiked) or peripheral halo on CT, most likely malignant 4. calcification pattern -if dense calcification in diffuse, central, laminated, or popcorn pattern, most likely benign -if sparse calcification in stippled or eccentric pattern, most likely malignant 5. cavitation -both benign and malignant lesions cavitate -if cavitary lesion with thick wall (>16mm), most likely malignant 6. location -most malignancies located in upper lobes 7. doubling time -review old radiographs -if size doubles in <30 days, most likely infection -if size doubles in >465 days, most likely benign -most malignancies double in 6 weeks to 16 months |
|
|
|
What is the ddx for a mediastinal mass?
|
• masses may be caused by developmental, traumatic, infectious, cardiovascular or neoplastic disorders
• anterior compartment ddx = thymoma, teratoma, thyroid lesions, lymphoma, mesenchymal tumors (lipoma, fibroma) • middle compartment ddx = lymphadenopathy, pulmonary artery enlargement, aortic aneurysm, developmental cyst (bronchogenic, enteric, pleuropericardial), dilated azygous or hemiazygous vein, foramen of Morgagni hernia • posterior compartment ddx = hiatus hernia, neurogenic tumor, meningocele, esophageal tumor, foramen of Bochdalek hernia, thoracic spine disease, extramedullary hematopoiesis |
|
|
|
What is the clinical presentation of a medistinal mass?
|
• 50% of cases are asymptomatic and detected on routine CXR
• signs/symptoms are nonspecific and usually caused by effects of mass on surrounding structures • insidious onset of dysphagia, dyspnea, and retrosternal chest pain • physical exam findings vary depending on type and location of mass |
|
|
|
What is the diagnostic workup of a mediastinal mass?
|
• CXR
• barium swallow if suspected esophageal disease • tissue biopsy if suspected neoplastic disorder • other possibilities include CT, MRI, ultrasound, and angiography |
|
|
|
What is the general management of a mediastinal mass?
|
dependent on underlying cause of mediastinal mass
|
|
|
|
What is superior vena caval syndrome?
|
clinical manifestation of superior vena caval obstruction → severe reduction in venous return from head, neck, and upper extremities
|
|
|
|
What is the etiology of superior vena caval syndrome?
|
usually caused by malignant tumors:
lung cancer 85% lymphoma → suspect if young adult metastatic cancer → often breast or testicular cancer other causes include benign tumor, aortic aneurysm, thyromegaly, thrombosis, and fibrosing mediastinitis |
|
|
|
What is the clinical presentation of superior vena caval syndrome?
|

facial and neck swelling
dyspnea cough other symptoms include pain, lethargy, HA, dizziness, syncopy, nasal congestion, epistaxis, tongue swelling, hoarseness, dysphagia, hemoptysis symptoms may be aggravated by bending over or lying down BP higher in upper extremities than lower extremities cyanosis edema of face, arms, and chest dilated neck veins increased number of collateral veins covering anterior chest wall |
|
|
|
What is the diagnostic workup of superior vena caval syndrome?
|
diagnosis made clinically
CXR may reveal superior RT mediastinal widening or RT pleural effusion other options include CT and bronchoscopy |
|
|
|
What is the general management of superior vena caval syndrome?
|
Symptomatic treatment includes:
1. head elevation 2. diuretics 3. supplemental O2 4. low-salt diet Treatment of underlying cause may include corticosteroids, radiation therapy, chemotherapy, surgery, or stenting |
|
|
|
Grey pseudomembrane in posterior orpharynx indictes?
|
diphtheria
|
Mosbys p343
|
|
|
What is the etiology of bronchogenic carcinoma?
|
90% due to smoking
others include environmental tobacco smoke, radon gas, asbestos, industrial carcinogens familial predisposition increased risk with COPD, interstitial lung disease, sarcoidosis |
|
|
|
What is the clinical presentation of bronchogenic carcinoma?
|
night sweats
anorexia weight loss dyspnea new cough or change in chronic cough hemoptysis clinical presentation depends on type, location, spread, metastasis |
|
|

|
grey pseudomembrane → diphtheria
|
|
|
|
What is the diagnostic workup of bronchogenic carcinoma?
|
CXR → enlarging nodule or mass; persistent opacity, atelectasis, or pleural effusion
pleural fluid biospy |
|
|
|
What is the prognosis of bronchogenic carcinoma?
|
41% survive first year
17% survive first 5 years |
|
|
|
What is the prevention of bronchogenic carcinoma?
|
do not smoke!
avoid environmental exposures! |
|
|
|
What is the common name for bronchogenic carcinoma?
|
lung cancer
|
|
|
|
What is the leading cause of cancer death?
|
lung cancer
|
|
|
|
What should you order to assess ventilation?
|
PFTs
|
|
|
|
What should you order to assess oxygenation?
|
pulse oximetry
ABG |
|
|
|
What does ABG stand for?
|
arterial blood gas
|
|
|
|
What are the indications for ordering an ABG?
|
dyspnea, tachypnea
suspected respiratory, renal, metabolic, or acid-base disorder |
|
|
|
What are the components of an ABG?
|
1. arterial pH
2. plasma oxygen (PO2) 3. plasma carbon dioxide (CO2) 4. plasma bicarbonate (HCO3−) 5. base excess/deficit 6. anion gap |
|
|
|
What is the procedure for performing an ABG?
|
1. perform Allen test
2. if patient on O2 → turn off O2 for 20-30 minutes before performing ABG for room air test or document amount of O2 being taken 2. draw blood from radial artery into syringe 3. place syringe on ice 4. deliver to lab immediately |
|
|
|
Why must an ABG be transported on ice?
|
to prevent continued in vitro changes in PaO2, PaCO2, and pH
|
Lab Data p.6
|
|
|
What is the normal range for blood pH?
|
7.34-7.45
|
|
|
|
If pH is ≤7.35, what is this called?
|
acidemia
|
Interpreting Laboratory Data p179
|
|
|
If pH is ≥7.45, what is this called?
|
alkalemia
|
Interpreting Laboratory Data p179
|
|
|
Is CO2 an acid or base?
|
acid
|
|
|
|
True or false, obstructive pulmonary diseases decrease air flow and volume?
|
false, only decrease air flow
|
Interpreting Laboratory Data p192
|
|
|
True or false, restrictive pulmonary diseases decrease air flow and volume?
|
true
|
Interpreting Laboratory Data p192
|
|
|
What is the definition of FVC (forced vital capacity)?
|
total volume of air exhaled as fast as possible after maximal inhalation
|
Interpreting Laboratory Data p194
|
|
|
What is the normal FEV1?
|
>80% of predicted normal value (based on gender, age, and height)
|
Interpreting Laboratory Data p194
|
|
|
For best results when performing spirometry ...
|
Patient should:
loosen/remove restrictive clothing (ties, belts) wear nose clip to minimize air loss through nose sit/stand up straight completely fill and empty lungs There should be no: hesitation/false start coughing during first second early termination evidence of leak (mouth not tightly around mouthpiece) evidence of obstruction (glottic closure, tongue, false teeth) |
|
|
|
Is HCO3 an acid or a base?
|
base
|
|
|
|
What is the normal range for PCO2?
|
35-45 torr
|
|
|
|
How would you describe the results of an ABG?
|
acidosis or alkalosis?
respiratory or metabolic? compensated or uncompensated? |
|
|
|
What patient population should not be given O2?
|
COPD patients
|
|
|
|
What radiographic views should be ordered for suspected airway obstruction/foreign body?
|
PA view
lateral view |
|
|
|
What radiographic views should be ordered for suspected pneumothorax?
|
PA view
expiratory view |
|
|
|
What radiographic views should be ordered for suspected pleural effusion?
|
PA view
lateral decubitus view |
|
|
|
What radiographic views should be ordered for suspected apical lung tumors?
|
PA view
lordotic view |
|
|
|
What are Kerley B lines?
|
small linear opacities in periphery of lung
|
|
|
|
What are the characteristics of Kerley B lines?
|
1-2cm
water density extend to pleura perpendicular to pleura represent increased fluid density in interlobar septa |
|
|
|
What do Kerley B lines usually indicate?
|
↑ pulmonary venous pressure + pulmonary edema
|
|
|
|
What is the ddx for Kerley B lines?
|
pulmonary edema 2° to CHF
pulmonary fibrosis lymphangitis carinomatosis |
|
|
|
What is the silhouette sign?
|
chest imaging sign
characterized by loss of border between structures in thoracic cavity → density of structures is abnormally equal helps to localize disease → lung, lobe, segment |
|
|
|
What is the interpretation of silhouette sign?
|
loss of LT heart border → LUL affected
loss of LT hemi-diaphragm border → LLL affected loss of RT heart border → RML affected loss of RT hemi-diaphragm border → RLL affected |
|
|
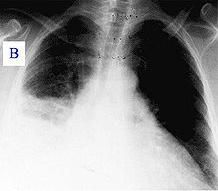
|
silhouette sign
loss of RT heart border indicates RML affected loss of RT hemi-diaphram border indicates RLL affected RML/RLL pneumonia |
|
|
|
What does PA stand for?
|
posteroanterior
|
|
|
|
What does AP stand for?
|
anteroposterior
|
|
|
|
Describe a PA view.
|
film place against anterior (chest) of patient; x-ray beam shot from posterior (back) of patient to anterior (chest) of patient
|
|
|
|
Describe an AP view.
|
film placed against back of patient; x-ray beam shot from anterior (chest) of patient to posterior (back) of patient
|
|
|
|
Which is better, AP view or PA view, and why?
|
1. PA view
2. heart and great vessels are situated more anteriorly 3. the closer the film is to structures, the less magnified and blurry those structures are |
|
|
|
What is a portable CXR?
|
AP CXR
film placed against back and x-ray beam shot from anterior to posterior |
|
|
|
What are the indications for a portable CXR?
|
patient incapable of standing or sitting for PA view
|
|
|
|
What are the limitations of a portable CXR?
|
since shot anterior to posterior, film further away from anterior structures (i.e. heart, great vessels)
the further away film is from structures, the more magnified and blurry they become thus heart is misleadingly magnified and heart borders are blurry |
|
|
|
What is a lordotic view?
|
CXR while patient leaning backwards
|
|
|
|
What is pulse oximetry?
|

noninvasive inexpensive method to monitor O2 saturation of hemoglobin
|
|
|
|
When is the clinical accuracy of pulse oximetry decreased?
|
1. severe anemia <5g/dL
2. abnormal hemoglobin moieties → carboxyhemoglobin, methemoglobin, fetal hemoglobin 3. intravascular dyes 4. motion artifact 5. lack of pulsatile arterial flow → hypotension, hypothermia, cardiac arrest, simultaneous use of BP cuff *pulse oximetry measures percent of bound hemoglobin but cannot distinguish the molecule that is actually bound (i.e. hemoglobin could be bound with carboxyhemoglobin following carbon monoxide poisoning and SaO2 would still be normal) |
|
|
|
What are the indications for pulse oximetry?
|
monitor oxygenation
|
|
|
|
What is polysomnography?
|
sleep study
tracks how often a person stops breathing (apnea) or breathing is blocked (hypopnea) |
|
|
|
What is bronchoscopy?
|

bronchoscope inserted into nose or mouth to view airways
bronchoscope may be rigid with light attached or flexible with video equipment |
|
|
|
What are the indications for ordering bronchoscopy?
|
FLEXIBLE BRONCHOSCOPY:
1. evaluate airway 2. remove foreign bodies or retained secretions 3. diagnose pulmonary disorders 4. bronchoalveolar lavage 5. diagnose and stage bronchogenic carcinoma 6. lung biopsy 7. evaluate hemoptysis (though not very effective since blood gets everywhere!) *contraindicated if severe bronchospasm or tendency to bleed RIGID BRONCHOSCOPY: 1. massive bleeding 2. removal of large obstructing objects → foreign bodies, blood clots, broncholiths, tumors 3. lung biopsy 4. laser therapy |
|
|
|
What is a ventilation and perfusion (VQ) scan?
|
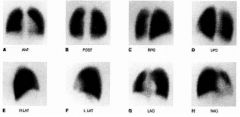
radiolabeled albumin injected into vein (to test perfusion) → patient breaths radioactive gas (to test ventilation) → distribution in lungs recorded
|
|
|
|
What are the VQ scan results for high probability of PE?
|
reduced perfusion + normal ventilation
|
|
|
|
What are the indications for ordering a VQ scan?
|
medium or high probability of PE
COPD pre- and post-lobectomy |
|
|
|
What are the indications for ordering a DDQ?
|
DVT
PE (only order if low probability of PE, if high probability of PE just order VQ scan) DIC |
|
|
|
What is a DDQ?
|
fibrin degradation product formed after a blood clot is degraded by fibrinolysis
|
|
|
|
What is a chloride sweat test?
|
induce sweating by placing pilocarpine on skin, placing electrode over it, and applying weak electrical current → clean area → collect sweat for 30 minutes with filter paper → measure chloride
|
|
|
|
What are the indications for ordering a chloride sweat test?
|
suspected CF
|
|
|
|
What is the gold standard for diagnosing CF?
|
chloride sweat test
|
|
|
|
What chloride sweat test results indicate CF?
|
PEDIATRIC:
≤29mmol/L = unlikely 30-59 mmol/L = possible ≥60 mmol/L = CF ADULT: ≤39 mmol/L = CF 40-59 mmol/L = possible ≥60 mmol/L = CF |
|
|
|
What are the indications for ordering polysomnography?
|
suspected sleep apnea
|
|
|
|
How do you determine if there is appropriate inflation on a CXR?
|
lungs should span 9 ribs
|
|
|
|
What is the anion gap?
|
anion gap = Na+ - (Cl- + HCO3-)
number of unmeasured anions normally exceeds number of unmeasured cations *anion = negative charged *cation = positively charged |
|
|
|
What does an increased anion gap indicate?
|
increase in negatively charged weak acids
loss og HCO3- without concurrent increase in Cl- bicarbonate consumed by unmeasured anion resulting in high anion gap increased anion gap indicates certain types of metabolic acidosis anion gap normal if metabolic acidosis caused by HCL production or excessive loss of bicarbonate anion gap elevated if metabolic acidosis caused by diabetic ketoacidosis, methanol intoxication, etc. (metabolic acidosis that leads to excess anions not in anion gap calculation) |
|
|
|
What is the base excess/deficit?
|
base excess = amount of strong acid that must be added to blood to return pH to 7.4
|
|
|
|
What does an abnormal base excess/deficit indicate?
|
abnormally high base excess = metabolic alkalosis
abnormally low base excess (i.e. base deficit) = metabolic acidosis |
|
|
|
What are the indications for ordering PFTs?
|
diagnostic, evaluation and monitoring of respiratory disease
diagnosis of asthma and COPD monitoring after thoracic radiation, lung transplantation, drugs with potential lung toxicity |
|
|
|
How is air flow affected in obstructive diseases?
|
decrease flow of air but not volume
|
|
|
|
How is air flow affected in restrictive diseases?
|
decrease flow and volume of air
|
|
|
|
What is forced vital capacity (FVC)?
|
total volume of air exhaled as hard and fast as possible after maximal inhalation
|
|
|
|
What is forced expiratory volume in 1 second (FEV1)?
|
amount of air exhaled after 1 second
|
|
|
|
What is the significance of the FEV1/FVC ratio?
|
used to estimate presence and amount of airway obstruction
ratio indicates amount of air mobilized in 1 second as a percentage of total amount of movable air normal = 50% in 0.5sec, 80% in 1sec, 98% in 3sec |
|
|
|
What is FEF(25-75)?
|
measures airflow rate during forced expiration from 25%-75% of vital capacity
25-75% is though to measure airflow in medium and small airways (bronchioles and terminal bronchioles) |
|
|
|
What is peak expiratory flow rate (PEFR)?
|
measure of maximum airflow rate (using peak flow meters)
|
|
|
|
What are the indications for peak flow meters (to measure peak expiratory flow rate)?
|
peak flow meters are useful indications of large airway function → monitor airway obstruction in asthmatics
|
|
|
|
What is body plethysmography?
|
method used to measure lung volume
patient sits in airtight box → told to inhale and exhale agaisnt a closed shutter → change in pressure measured during respiration → can calculate FRC, IC, RV, TLC |
|
|
|
What is residual volume (RV)?
|
volume of air remaining in lungs after forced expiration
|
|
|
|
What diseases have increased residual volume?
|
COPD
|
|
|
|
What is inspiratory capacity (IC)?
|
volume of air measured from beginning of inspiration to maximal inspiration
|
|
|
|
What diseases show increased/decreased functional residual volume (FRC)?
|
INCREASED:
hyperinflation → airway obstruction → obstructive lung diseases DECREASED: pneumonia restrictive lung diseases → pulmonary fibrosis |
|
|
|
What is total lung capacity (TLC)?
|
measure of total amount of gas in lungs at maximal inhalation
|
|
|
|
List 4 types of pharyngitis/tonsillits.
|
1. viral pharyngitis
2. group A beta-hemolytic streptococcal pharyngitis (GABHS) 3. mononucleosis 4. diphtheria |
|
|
|
What are the FEV1/FVC, FEV1, FVC, RV, and TLC results for obstructive and restrictive lung diseases?
|
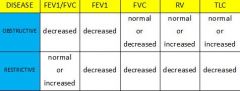
|
|
|
|
What is the air bronchogram sign?
|
normally bronchi are not visible because they are filled with air and surrounded by air
if surrounding alveoli become filled with fluid, bronchi become visible as dark branching markings surrounded by abnormal white lung may indicate pneumonia, pulmonary edema, or hemorrhage lesion must be in lung! |
|
|
|
What is the ddx for kerley B lines?
|
pulmonary edema → often due to CHF
lymphangitic carcinomatosis |
|
|
|
What is cephalization?
|
upper lobe vessels increase in size compared to lower lobe vessels → pulmonary venous hypertension (only if patient erect when CXR taken due to influence of gravity)
|
|
|
|
"Bat wing" appearance on CXR indicates?
|
pulmonary edema
|
|
|
|
List drug classes used to treat lung disease.
|
short-acting beta agonists → all asthma, COPD; bronchodilator
inhaled corticosteroids → mild, moderate, severe asthma; anti-inflammatory long-acting beta agonists → moderate, severe asthma; bronchodilator systemic corticosteroids → severe asthma; anti-inflammatory mast cell stabilizer → asthma prophylaxis; inhibitts histamine release anticholinergics → COPD; inhibits Ach → bronchodilation phosphodiesterase inhibitors → do not prescribe; bronchodilator leukotreine modifiers → asthma prophylaxis; inhibits arachidonic acid pathway |
|
|
|
List short acting beta agonists.
|
albuterol
pirbutelol terbutaline levalbuterol metaproterenol |
|
|
|
What is the MOA of short acting beta agonists?
|
B2 agonists → binding causes relaxation of airway smooth muscle → bronchodilation
effective in 5-30 minutes last 4-6 hours |
|
|
|
What is the MOA of long acting beta agonists?
|
B2 agonists → binding causes relaxation of airway smooth muscle → bronchodilation
*analogs to albuterol but possess lipophilic side chain that increases affinity for B2-adrenoreceptors → increasing duration last 12 hours |
|
|
|
What is are the indications for SABA?
|
prevention or treatment of bronchospasm in asthma
prevention of exericise-induced asthma |
|
|
|
List antitubercular drugs.
|
isoniazid
rifampin pyrazinamide ethambutol |
|
|
|
What is the treatment protocol for TB?
|
1. if latent TB → treat with isoniazid x 9 months
2. if active TB → treat with isoniazid + rifampin + ethambutol + pyrazinamide x 2 months → then isoniazid + rifampin x 4 months 3. add more drugs if previous TB or suspected resistant TB |
Pharmacology p400
|
|
|
What is the MOA for isoniazid?
|
inhibits enoyl acyl carrier protein reductase (InhA) and B-ketoacyl-ACP synthase (KasA) → inhibiting mycolic acid synthesis → inhibiting mycobacterial cell wall synthesis
|
Pharmacology p400
|
|
|
What are the indications for isoniazid?
|
latent TB
active TB |
Drug Information Handbook p820
|
|
|
What are the side effects of isoniazid?
|
hypersensitivity
peripheral neuritis (parasthesias of hands and feet) hepatitis and idiosyncratic hepatotoxicity inhibits metabolism of phenytoin → potentiating side effects of phenytoin → nystagmus, ataxia |
Pharmacology p401
|
|
|
What is the MOA of rifampin?
|
inhibits mRNA synthesis (transcription)
|
Pharmacology p402
|
|
|
What are the indications for rifampin?
|
active TB
meningitis prophylaxis OFF LABEL: h. flu prophylaxis legionella pneumonia leprosy |
Drug Information Handbook p1315
|
|
|
What are the side effects of rifampin?
|
nausea
vomiting rash hepatitis (rare) liver failure (rare) *beware if elderly, alcoholic, or chronic liver disease *make cause flu-like syndrome with fever, chills, myalgias *sometimes associated with acute renal failure, hemolytic anemia, and shock |
Pharmacology p402
|
|
|
What is the MOA of ethambutol?
|
inhibits arabinosyl transferase → inhibiting mycoplasma cell wall
|
Pharmacology p403
|
|
|
What are the indications for ethambutol?
|
adjunctive treatment of active TB
other mycobacterial diseases |
Drug Information Handbook p573
|
|
|
What are the side effects of ethambutol?
|
optic neuritis → decreased visual acuity and loss of ability to discriminate red and green
decreased uric acid secretion → gout |
Pharmacology p403
|
|
|
What is the MOA of pyrazinamide?
|
unknown
|
Pharmacology p403
|
|
|
What are the indications for pyrazinamide?
|
adjunctive treatment of active TB
|
Drug Information Handbook p1270
|
|
|
What are the side effects of pyranizamide?
|
fatigue, nausea, vomiting, anorexia, myalgia, arthralgia
liver dysfunction decreased uric acid secretion → gout |
Pharmacology p403
|
|
|
What are the symptoms of acute theophylline overdose?
|
MILD INTOXICATION:
nausea vomiting tachycardia tremors SEVERE INTOXICATION: hypotension seizures supraventricular tachy arrhythmias ventricular arrhythmias ACUTE OVERDOSE: hypokalemia hyperglycemia hypercalcemia hyperphosphatemia metabolic acidosis |
Current ch38
Pharmacology p325 http://emedicine.medscape.com/article/818847-treatment |
|
|
What is the management of acute theophylline overdose?
|
1. activated charcoal
2. if large ingestion involving sustained release preparations → whole bowel irrigation in addition to charcoal 3. benzodiazepines for seizures 4. B-blockers for hypotension and tachycardia |
Current ch38
http://emedicine.medscape.com/article/818847-treatment |
|
|
What are the indications for varenicline (Chantix)?
|
aid in smoking cessation
|
Drug Information Handbook p1548
|
|
|
What is the MOA of varenicline?
|
partial neuronal alpha4 beta2 nicotinic cholinergic receptor agonist → preventing nicotine stimulation of meso-limbic dopamine system associated with nicotine addiction
*stimulates dopamine secretion but too much smaller degree than nicotine → resulting in decreased craving and withdrawal symptoms |
Drug Information Handbook p1548
|
|
|
What are the contraindications of varenicline?
|
none
|
Drug Information Handbook p1548
|
|
|
What are the adverse effects and interactions of varenicline?
|
fatigue
HA nausea GI symptoms insomnia abnormal dreams/vivid nightmares mood changes suicidal thoughts no interactions |
Pharmacology p119
|
|
|
What is the patient education for varenicline?
|
may cause sedation so do not drive or operate heavy machinery
if experience any behavioral or mood changes stop treatment and contact provider immediately |
Drug Information Handbook p1548
|
|
|
What are the indications for prescribing buproprion?
|
major depressive disorder
seasonal affective disorder adjunct in smoking cessation |
Drug Information Handbook p223
|
|
|
What is the MOA of buproprion?
|
inhibits reuptake of dopamine and norepinephrine
|
Pharmacology p145
|
|
|
What are the contraindications for buproprion?
|
children
pregnancy lactation hypersensitivity seizure disorder anorexia/bulemia use of MAO inhibitors with 14 days abrupt discontinuation of alcohol or sedatives |
Drug Information Handbook p224
|
|
|
What are the adverse effects and interactions of buproprion?
|
HA
tachycardia insomnia dizziness weight loss nausea pharyngitis dry mouth sweating nervousness tremor sexual dysfunction seizures (increased risk at high doses) |
Pharmacology p145
|
|
|
What are the indications for prescribing buproprion?
|
major depressive disorder
seasonal affective disorder adjunct in smoking cessation |
Drug Information Handbook p223
|
|
|
What is the MOA of buproprion?
|
inhibits reuptake of dopamine and norepinephrine
|
Pharmacology p145
|
|
|
What are the contraindications for buproprion?
|
children
pregnancy lactation hypersensitivity seizure disorder anorexia/bulemia use of MAO inhibitors with 14 days abrupt discontinuation of alcohol or sedatives |
Drug Information Handbook p224
|
|
|
What are the adverse effects and interactions of buproprion?
|
HA
tachycardia insomnia dizziness weight loss nausea pharyngitis dry mouth sweating nervousness tremor sexual dysfunction seizures (increased risk at high doses) avoid concomitant use with MAO inhibitors, alcohol, antidepressants |
Pharmacology p145
|
|
|
What type of drug is cromolyn?
|
mast cell stabilizer
|
|
|
|
What are the indications for cromolyn?
|
inhaled → prophylaxis for allergic disorders including asthma; prevention of exercise-induced bronchospasm
nasal → prevention and treatment of allergic rhinitis |
|
|
|
What are the contraindications for cromolyn?
|
hypersensitivity
acute asthma attacks |
|
|
|
What is the MOA of cromolyn?
|
inhibits degranulation after contact with antigens → preventing mast cell release of histamine and leukotrienes
|
|
|
|
What is the adverse effects and interactions of cromolyn?
|
side effects low due to poor absorption
bitter taste irritation of pharynx and larynx |
|
|
|
What is the patient education for cromolyn?
|
only for prophylaxis!
not for acute asthma attacks! |
|
|
|
What is the patient education for use of metered dose inhalers?
|
inhale SLOWLY and DEEPLY
if improperly inhaled → 80-90% deposited in mouth, pharynx, or swallowed → systemic absorption → increase in adverse effects To use an MDI: Shake the inhaler well before use (3 or 4 shakes) Remove the cap Breathe out, away from your inhaler Bring the inhaler to your mouth. Place it in your mouth between your teeth and close you mouth around it. Start to breathe in slowly. Press the top of you inhaler once and keep breathing in slowly until you have taken a full breath. Remove the inhaler from your mouth, and hold your breath for about 10 seconds, then breathe out. If you need a second puff, wait 30 seconds, shake your inhaler again, and repeat steps 3-6. After you've used your MDI, rinse out your mouth and record the number of doses taken. |
|
|
|
What is the patient education for use of dry powder inhalers?
|
inhale QUICKLY and DEEPLY
"swish and spit" after use to prevent deposition on oral and laryngeal mucosa which can lead to hoarseness and candidiasis |
|
|
|
What type of drug is theophylline?
|
phosphodiesterase inhibitor
|
|
|
|
Describe theophylline.
|
bronchodilator
narrow therapeutic window lots of side effects and drug interactions overdose may cause seizures and arrhythmias |
|
|
|
List leukotriene modifiers.
|
zarfirlukast
montelukast zileuton |
|
|
|
What are the indications for leukotriene modifiers?
|
prophylaxis of asthma
NOT for acute asthma |
|
|
|
What are the adverse effects and drug interactions of leukotriene modifiers?
|
elevated liver enzymes → requires monitoring
Churg-Strauss HA dyspepsia |
|
|
|
What are the indications for anticholinergics?
|
oral inhalation → anticholinergic bronchodilator used in brochospasm associated with COPD
use in conjunction with SABA! may cause reflexive bronchospasm use with caution if myasthenia gravis, narrow-angle glaucoma, prostatic hyperplasia, or bladder neck obstruction |
|
|
|
What is the MOA of anticholinergics?
|
inhibits action of Ach at parasympathetic sites in bronchial smooth muscle → bronchodilation
|
|
|
|
List antiplatelets, anticoagulants, and thrombolytics used in the treatment of thrombotic/embolic cardiopulmonary disorders.
|
ANTIPLATELETS:
aspirin clopridogrel (Plavix) ticlodopine (Ticlid) ANTICOAGULANTS: heparin LMWH warfarin THROMBOLYTICS: alteplase (Activase) |
|
|
|
What is the clinical use of clopridogrel (Plavix)?
|
MOA → antiplatelet
clinical use → reduces rate of atherothrombotic events -unstable angina -NSTEMI -STEMI -PAD -stroke *risk of bleeding |
Drug Handbook p356
|
|
|
What is the clinical use of warfarin?
|
MOA → anticoagulant
clinical use -thrombosis/embolism → DVT, PE -reduce risk of embolic complications from atrial fibrillation or valve replacement -reduce risk of systemic embolism following MI |
Drug Handbook p1570
|
|
|
What is the clinical terminology for lung cancer?
|
adenocarcinoma of the lung
|
|
|
|
|
Pertussis
This is a young girl with whooping cough. You can hear her paroxysmal cough first without a whoop. Then you hear two more paroxysms, both followed by the distinctive whooping sound. It is the noise of breathing in, and comes from the larynx (voice box). |
|

