![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
154 Cards in this Set
- Front
- Back
|
Definition of joint mobilization |
Manual therapy techniques that are used to modulate pain and treat joint dysfunctions that limit ROM by specifically addressing the altered mechanics of the joint. |
|
|
What is the difference between the 5 grades of peripheral joint mobilizations? |
1 - Small amplitude at beginning of available joint motion 2 - Larger amplitude in the middle of available joint motion 3 - Large amplitude from the mid-range to end-range of available joint motion 4 - Small amplitude at the end-range of available joint motion 5 - High velocity thrust |
|
|
Indications for joint mobilization |
|
|
|
Contraindications for joint mobilization |
Hypermobility Joint Effusion Inflammation |
|
|
What is the concave/convex rule and how does it apply to joint mobilization? |
If the surface of the moving bone is convex, sliding is in the opposite direction of the segment's movement If the surface of the moving bone is concave, sliding is in the direction of the segment's movement |
|
|
What are patient/therapist considerations when choosing interventions that affect soft tissue? |
|
|
|
Posterior glide of the humerus increases what? |
Flexion |
|
|
Anterior glide of the humerus increases what? |
Extension |
|
|
Inferior (caudal) glide of the humerus increases what? |
Abduction |
|
|
Dorsal glide of the wrist increases what? |
Flexion |
|
|
Volar glide of the wrist increases what? |
Extension |
|
|
Ulnar glide of the wrist increases what? |
Radial Deviation |
|
|
Radial glide of the wrist increases what? |
Ulnar Deviation |
|
|
Posterior glide of the tibia increases what? |
Knee Flexion |
|
|
Anterior glide of the tibia increases what? |
Knee Extension |
|
|
Anterior glide of the femur increases what? |
Extension and ER
|
|
|
Posterior glide of the femur increases what? |
Flexion and IR
|
|
|
Long axis distraction of the hip increases what? |
Pain control, general mobility
|
|
|
Reasons for altered mechanics: |
|
|
|
Purpose of joint mobilizations? |
Replicate the desired normal joint mechanics Minimize the abnormal stresses on the cartilage/joint. |
|
|
Conditions requiring special precautions for joint mobilization: |
Pregnancy, bone disease, unhealed fractures, total joint replacements, acute post op, systemic connective tissue diseases (RA), elderly |
|
|
What are some signs and symptoms of excessive fatigue? |
Dyspnea Dizziness Increased Pain Intermittent claudication Pallor/Diaphoresis
|
|
|
What is the role of the PTA in a cardiac rehab phase one? |
PTA sees 2nd treatment (PT is 1st) Obtain permission from nurse to treat pt - they have the most up to date vital info and knows how the pt faired overnight Progress from initial eval status as indicated - Alert PT/nurse if anything changes for the worse |
|
|
Cardiac Rehab: Phase One Patient Education |
|
|
|
Cardiac Rehab Transfer precautions |
|
|
|
Cardiac Rehab Gait precautions |
|
|
|
Cardiac Rehab: Phase Two |
|
|
|
Example visit protocol: Phase Two Cardiac Rehab |
|
|
|
Phase Three Cardiac Rehab |
|
|
|
Phase Three: Strengthening exercise guidelines |
|
|
|
Components of a typical physical therapy evaluation for a patient who has a cardiac and/or pulmonary impairment: |
(Phase One Rehab) - usually begins 1 day s/p CABG PT eval: PMH, social situation, pain, cognition, strength of all extremities, monitor vitals, transfer ability, gait ability, begin pt/family education, set goals ,declare rehab potential, set d/c plan |
|
|
Goals for Acute Care with cardiac diseases: |
|
|
|
Cardiac Conditioning for the Healthy population: |
*** MHR for cardiac patients is symptom limited |
|
|
Pulmonary Diseases - PT eval: |
PMH, social situation, pain, cognition, strength of all extremities, monitor vitals, transfer ability, gait ability, begin pt/family education, set goals, declare rehab potential, set d/c plan |
|
|
Goals for Acute Care with Pulmonary Diseases |
|
|
|
PT Interventions for pulmonary diseases |
|
|
|
Pulmonary Disease - Patient Education |
|
|
|
Diaphragmatic technique: |
Tactile input at diaphragm; verbal cues to decrease use of accessory muscles. Quick stretch then applied prior to inhalation; graded manual resistance PRN |
|
|
Lateral expansion technique |
Tactile input at lateral inferior borders of chest wall; verbal cues to feel that section expand with inhalation. Quick stretch then applied prior to inhalation; graded manual resistance PRN |
|
|
Postural Drainage Precautions: |
|
|
|
Postural Drainage Contraindications: |
Broken Ribs, Osteoporosis
|
|
|
Duration of postural drainage percussions: |
3-5 minutes, followed by 1 minute of shaking |
|
|
Positions for postural drainage: |
|
|
|
Indications for aquatic therapy: |
|
|
|
Contraindications for aquatic therapy: |
|
|
|
Aquatic therapy precautions: |
|
|
|
Specific Heat |
Slow to heat up, slow to cool down |
|
|
Thermal conductivity |
Transfers heat quickly, therefore able to to heat (or cool) the body quickly |
|
|
Buoyancy |
Upward thrust on the body, opposite of gravity |
|
|
Archimede's Principle |
A body will have an upward thrust equal to the amount of water displaced. Offers "active assistance" to ther ex. Affected by the object's density |
|
|
Surface Tension |
Molecules at the surface have a greater tendency to stick to each other - therefore the surface will have a higher tension than below
|
|
|
Adhesion |
Tendency of water molecules to stick to other surfaces (why you drip dry)
|
|
|
Viscosity |
Resistance to the flow of a liquid due to friction created among the molecules when disturbed. Creates turbulence when water sis disturbed - Streamlined effects vs drag
|
|
|
Streamline |
A teardrop line of count our offering the least possible resistance to a current of air, water, etc |
|
|
Turbulence |
Movement of water in a circular pattern to create eddy currents - opposite of streamline - disruption of water molecules from resting position |
|
|
Hydrostatic pressure |
Pressure exerted by a fluid on a body immersed in that fluid - good for edema control |
|
|
Pascal's Law |
The deeper the body is immersed, the greater the pressure - a submerged segment has equal pressure to all parts |
|
|
Benefits of shallow water |
Weight reduction (25% at knee deep, 50% at waist deep) |
|
|
Benefits of deep water |
Weight reduction (75% at chest deep)
|
|
|
Water temp for rehab/therapy |
90-95 |
|
|
Water temp for arthritis |
83-90 |
|
|
Water temp for cool water vigorous exercise |
83-86 |
|
|
Water temp for competitive swimming |
78-82 |
|
|
Water temp for the obese |
80-86 |
|
|
Cardiovascular and pulmonary changes that occur with submersion in water |
Pulmonary - decreased VC, increased energy expenditure to breathe Cardiovascular - hydrostatic pressure displaces venous blood proximally, which increases cardiac volume, stroke volume, and cardiac output |
|
|
Patient education for aquatic therapy |
|
|
|
What is an example of a buoyancy resisted exercise? |
Pushing noodle down through the water
|
|
|
What is an example of a buoyancy assisted exercise? |
Allowing the water to help bring a noodle back to the surface
|
|
|
Gait Cycle |
Heel strike of one foot to the next heel strike of the same foot. Always measured as the same side, same portion of gail phase (may not always be heel strike) 60% stance phase, 40% swing phase, and two periods of double support (heel strike-toe off) |
|
|
Stance Phase |
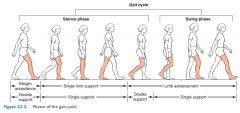
60% of Gait Cycle
|
|
|
Swing Phase |
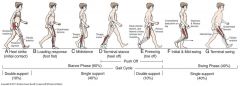
40% of Gait Cycle
|
|
|
Double Support Phase |
Both feet touching ground
|
|
|
Step Cadence |
Number of steps taken in a given period of time |
|
|
Step Length |
Point of heel strike of one LE to the point of heel strike of the other LE |
|
|
Stride Length |
Distance covered during the gait cycle |
|
|
Foot Slap |
Weakness of anterior tibialis; foot slaps ground due to no eccentric control |
|
|
Lack of heel strike |
Leg length discrepancy, heel cord contracture, heel pain |
|
|
Toe drag |
Lack of DF; toes never clear the ground due to lack/weakness of anterior tibialis |
|
|
Excessive knee flexion |
Weakness in quads, flexion contracture, muscle guarding with knee pain, leg length discrepancy |
|
|
Genu recurvatum |
Knee hyperextension due to lack of joint stability; locked into hyperextension by ligamental and bony support |
|
|
Excessive hip flexion (steppage) |
Used with foot drop to try to avoid toe drag - like you're trying to step over something |
|
|
Hip Circumduction |
Weak iliopsoas, weak anterior tibialis; circumducts rather than forward advancement |
|
|
Hip hiking |
Weak hamstrings, weak anterior tibialis, fused or braced knee
|
|
|
Trendelenburg |
Excessive trunk lateral flexion to compensate for weak glute meds on stance side, and prevent pelvic drop on swing through side; or protect a painful hip |
|
|
Antalgic |
Protective of painful area, shortened step length; uneven cadence, may coincide with additional abnormal patterns |
|
|
Ataxic |
Unsteadiness due to lack of control of proprioception |
|
|
Festinating |
Repetitive tip-toe pattern for patients with Parkinson's Disease. Uncontrollable gait, comes to an abrupt halt at an object |
|
|
Hemiplegic |
Circumduction of hip for momentum to advance the flaccid extremity |
|
|
Parkinsonian |
Flexed knees and trunk, shuffling gait (with occasional festination) |
|
|
Scissor |
Leg crosses midline during swing through |
|
|
Spastic Diplegia |
Cerebral Palsy "controlled fall" pattern (40-50% of patients with CP) Typically with hip add, hip IR, hip flexion, knee flexion, PF Momentum and velocity maintain upright posture with gait |
|
|
What is Rhythmic Auditory Stimulation? |
Using music to elicit rhythmical step patterns and cues - can be used to relax fear of falling prior to or during treatment - can also be used as a stimulating or inhibiting cue
|
|
|
Partial toe amputation |
Excision of any part of one or more toes
|
|
|
Toe disarticulation |
Disarticulation at the metatarsal phalangeal joint
|
|
|
Partial foot/ray resection |
Resection of the 3rd, 4th, 5th metatarsals and digits
|
|
|
Transmetatarsal amputation |
Amputation through the midsection of all metatarsals
|
|
|
Ankle disarticulation (SYMES) |
Ankle disarticulation with attachment of heel pad to distal end of tibia; may include removal of malleoli and distal tibial/fibular flares
|
|
|
Long transtibial amputation |
BKA - More than 50% of tibial length
|
|
|
Short transtibial amputation |
BKA - Less than 20% of tibial length
|
|
|
Knee disarticulation |
Amputation through the knee joint; femur intact
|
|
|
Long transfemoral amputation |
AKA - More than 60% of femoral length
|
|
|
Transfemoral amputation |
AKA - Between 35% -60% of femoral length
|
|
|
Short transfemoral amputation |
AKA - Less than 35% of femoral length
|
|
|
Hip disarticulation |
Amputation through hip joint; pelvis intact
|
|
|
Hemipelvetomy |
Resection of lower half of the pelvis
|
|
|
Hemicorportectomy |
Amputation of both lower limbs and pelvis below L4-L5 level
|
|
|
Posterior flap closure |
Leaves a scar line anteriorly across the limb |
|
|
Equal flap closure |
Equal length anterior/posterior closures - leaves a horizontal scar at midline of the limb. |
|
|
What are the 2 leading causes of amputation? |
PVD - leading cause for LE amputations, especially when coupled with smoking and diabetes
Trauma - most commonly from MVA or gunshot/military trauma |
|
|
Neuroma |
A bundle of nerve tissue - painful if compressed. Must sufficiently pad the area |
|
|
Phantom pain |
Cramping, squeezing, shooting/burning pain in an area that no longer exists |
|
|
Phantom sensations |
Tingling, burning, itching, pressure or numbness in an area that no longer exists |
|
|
How can mirror therapy help decrease the phantom pains of a RL? |
It allows the mind to "see" the missing limb and can potentially help decrease the noxious sensations by "treating" the reflected limb.
|
|
|
Rigid compression dressing |
Plaster casting molded to keep limb in desired shape - not removable Advantages: decreased edema, decreased pain, earlier ambulation, earlier transition to permanent prosthesis |
|
|
Removable rigid compression dressing |
Plaster or plastic that can be removed to checking healing/signs of infection/wounds Advantages: decreased edema, decreased pain, earlier ambulation, earlier transition to permanent prosthesis |
|
|
Semi-rigid compression dressing |
Unna style boot. Provides medicinal protection against infection, not as much support as rigid |
|
|
Soft compression dressing |
Elastic wraps or shrinker sock Advantages: inexpensive, light weight, clean Disadvantages: poor edema control, can cut off circulation if wrapped incorrectly or slips with movement, frequent reapplication needed |
|
|
What is a Syme's prosthesis? |

|
|
|
What is a partial foot prosthesis? |

|
|
|
Exoskeletal prosthetic device |
Made of hard, shiny plastic. Obvious external hardware at knee joint. Most durable cover, but least cosmetic. Most commonly used as training leg prior to final prosthesis. |
|
|
Endoskeletal prosthetic device |
Uses a central metal shank covered with soft plastic or foam rubber "skin-like" substance. More natural appearance. Easier to adjust. Most commonly use as final prosthesis. |
|
|
What is the purpose of reliefs and build-ups in prosthetic limbs? |
Reliefs are concave surfaces that allow decreased pressure over bony areas
Buildups are convex surfaces that allow increased pressure to more tolerant areas, such as muscle, tendons, and less prominent bony areas |
|
|
Quadrilateral containment (TFA) |
Lower posterior and medial shelf for ischial tuberosity and gluteals, higher lateral and anterior wall to direct forces to the posterior.
|
|
|
Ischial containment (TFA) |
Narrower med/lat borders, weight is shifted to med/lat sides and distal limb instead of ischial tuberosity
|
|
|
Vacuum suspension |
Removes all air molecules between liner, limb and socket - Allows consistent shape of limb, good for would healing, decreases shearing forces of movement, assists proprioception
|
|
|
Cuff (prosthetic attachment) |
Leather strap that surrounds the distal thigh
|
|
|
Corset prosthetic attachment |
Leather or flexible plastic attachment that laces up the thigh. Can be problematic due to pressure atrophy
|
|
|
Distal pin prosthetic attachment |
Liner has a pin attachment that locks into place on prosthesis
|
|
|
Suprochondylar brim prosthetic attachment |
Medial and lateral edges extend above the femoral epicondyles; also uses removable medial wedge.
|
|
|
Supercondylar/suprapatellar brim prosthetic attachment |
Also extends anteriorly above patella - good for short transtibial amputations
|
|
|
General acute care bed exercises for TKA: |
Immediatepost-op ex: GS, QS, SAQ, HS, SLR, hip abd, AP;(requires AAROM for SAQ, SLR, abd,& HS initially)
|
|
|
General acute care bed exercises for posterior THA: |
If posterior approach, NO SLR with bed exercises
Immediate post-op ex: GS, QS, SAQ, HS, hip abd, AP; (requires AAROM for SAQ, abd, & HS initially) JointCamp= standing mini-squats with RWx,4-way standing SLR with affected side, standing HS curls, standing heel raises,step-to’s on4 inch – 6 inch step |
|
|
General acute care bed exercises for anterior THA: |
|
|
|
General acute care bed exercises for spinal surgeries: |
Transfers - log roll
Ambulation as frequent as possible with assistance, RWX as needed NO SLR, bed ex progressed to standing |
|
|
What is the typical length of stay for a TKA? |
D/C usually 3-5 days to home or subacute rehab
|
|
|
What is the typical length of stay for a THA? |
D/C usually 3-5 days to home or subacute rehab
|
|
|
What is the typical length of stay for spinal surgeries? |
D/C usually 2-5 days - may require subacute rehab if not yet independent with self care, transfers and ambulation
|
|
|
When should you recommend subacute rehab placement for a patient who had elective orthopedic surgery? |
|
|
|
What is the PRE-op procedure for elective surgeries? |
|
|
|
What is the POST-op procedure for elective surgeries? |
|
|
|
COG |
|
|
|
What are the 6 gait determining factors? |
Pelvic Rotation Pelvic Tilt Pelvic Lateral Displacement Knee Flexion Hip Flexion Knee and Ankle Interaction |
|
|
SACH foot |
Sold Ankle Cushioned Heel; most commonly prescribed - comes in many sizes and angles for use in many shoes |
|
|
SAFE foot |
Stationary Attachment Flexible Endoskeleton; Allows some med/lat mobility for stability on uneven surfaces - more expensive and heavier than SACH |
|
|
What are some joint knee options for prosthetic limbs? |
Axis system (flex/ext or flex/ext/rotation) Friction Mechanism (modified speed of motion) Extension aid (elastic bands pull knee into extension) Mechanical stabilizer (manual lock into extension, delayed flexion) C leg Computerized leg (expensive, highest quality of mobility) |
|
|
Common post-surgical amputation complications? |
Infection DVT Neuroma |
|
|
Sample bed exercises after amputation? |
Positioning - avoid hip and knee flexion contractors - position pt in prone, no pillow in supine Prone/sidelying hip extension Supine/sidelying abduction Supine hip flexion Sidelying adduction SAQ (transtibial) Glute squeezes Quad sets Hip rotation stretches |
|
|
Shoulder in Sling Scenario |
|
|
|
THA with hip precautions Scenario |
|
|
|
TKA with Knee Immobilizer and CPM Scenario |
|
|
|
TTA and TFA Scenarios |
|
|
|
CABG Scenario |
|
|
|
COPD Scenario |
|
|
|
Lumbar Brace Scenario |
|

