![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
471 Cards in this Set
- Front
- Back
|
Homeostasis |
The maintenance of nearly constant conditions in the internal environment |
|
|
Na+ and K+ - relative position in periodic table? distinguishing characteristics for membrane channels?
|
Na+ above (smaller) K+ |
|
|
Glycocalyx
a. Composition (3) b. Function (4) |
a. Glycoproteins (most integral proteins), proteoglycans (most are attached only to the outside), glycolipids (ca. 10%) |
|
|
Temperature
a. The core temperature remains within ... of the normal, except in febrile illness b. Normal core temperature c. Physiological range during extreme heat and cold |

a. +- 0.6 C
b. Range from 36-37.5 C. (Average is 36.7-37 C when measured orally and 0.56 (1F) higher when measured rectally) c. 35.6-40 C (Guyton) |
|
|
How is the relative heat conducting capacity of fat compared to other tissue?
|
1\3
(Guyton) |
|
|
Blood flow to the skin from the body core provides heat transfer
a. How much can the rate of blood flow into the skin venous plexus vary? b. How many times can the heat conductance increase from the fully vasoconstricted state to the vasodilated state at 42C |
a. From barely above zero to as high as 30% of cardiac output.
b. 8 times (Guyton) |
|
|
Heat regulation
a. Mechanisms of heat loss from the skin surface (3) b. What is the only mechanism possible to cause heat loss when the air temperature is higher than the body temperature? |
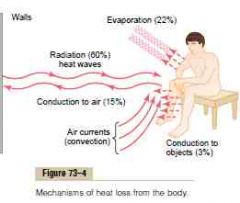
a. 1. Radiation
(60%, loss in the form of infrared heat rays. All objects that are not at absolute zero temperature radiate such rays. Also works in the other direction on the body from a warmer object) 2. Conduction a. Conduction by solid objects (3%, due to the principle that heat = molecular movement which can be spread) b. Conduction to air (15%, Convection of air refers to the phenomenon where heated air rise away from the skin (higher kinetic energy involved in the collisions of gas particles in a gas cause the gas to increase in volume -> increase length between particles -> decrease density) (Cooling effect of wind: when the body is exposed to wind, the layer of air immediately adjacent to the skin is replaced by new air much more rapidly than normally, and heat loss by convection increases accordingly. The cooling effect of wind at low velocities is about proportional to the square root of the wind velocity) 3. Evaporation (Evaporation occurs when a liquid (such as sweat) changes phase to a vapor (sweat vapor). This phase change requires heat.) (Insensible evaporative water loss is 600-700 ml\day, from uncontrollable diffusion of water molecules)) b. Evaporation (Guyton) |
|
|
Specific heat
a. Definition b. Relation to heat loss to water and to air |
a. The amount of heat required to raise any substance through 1 C of temperature, compared with that of raising the same volume of water 1 C.
b. Water has a specific heat several thousand times as great as that of air, so that each unit portion of water adjacent to the skin can absorb far greater quantities of heat than air can. (Explains why it is so important to avoid wet clothing in a person suffering from hypothermia) (Guyton) |
|
|
Sweating and its regulation by the autonomic nervous system
a. Stimulation of which brain area cause sweating b. Pathway |
a. The anterior hypothalamus-preoptic area
(When stimulated electrically or by heat) b. Sympathetic nervous system -> cholinergic fibers -> stimulate sweat glands (Circulating epinephrine and norepinephrine can also stimulate sweat glands. Important during exercise) (Guyton) |
|
|
Sweat secretion
a. Mechanism b. How is the sweating mechanism acclimatized to heat |

a.
1. The coiled portion secrete primary secretion which is like plasma besides the protein (Elicited by cholinergic sympathetic nerve fibers) 2. The duct portions reabsorbs a regulated amount of it. Increased stimuli -> increased precursor fluid production -> increased flow -> less of the sodium and chloride have time to get reabsorbed (Thus with low amount of primary secretion much of the sodium and chloride has time to be absorbed with water subsequently following it. Low output sweat can have sodium concentration of 5 mM while high output (less modified) can have sodium concentration of 60 mM) b. Increased ability of the sweat glands to excrete a higher volume and an decreased concentration of sodium and chloride due to increased secretion of aldosterone. (An unacclimatized person can lose 15-30g of salt per day, after 4-6 weeks the loss is usually 3-5g per day) (Guyton) |
|
|
A normal nude person is able to maintain normal core temperature within what range of external temperature?
|
13-55 C
(Guyton) |
|
|
Regulation of body temperature
a. Location of temperature-regulating centers b. Location of temperature sensors c. Ways to increase body temperature (4) |
a. Bilaterally in posterior hypothalamus
(At level of mammillary bodies) (Primary motor center for shivering is in dorsomedial portion of the posterior hypothalamus) b. 1. Anterior hypothalamic-preoptic area (Large number of heat-sensitive neurons, 1\3 as many cold-sensitive neurons) 2. Temperature receptors in the skin (cold- and heat-sensitive sensors, 10 times as many cold-sensitive) 3. Temperature receptors in some specific deep tissues of the body (spinal cord, abdominal viscera, great veins in upper abdomen\thorax) (Detect mainly cold) c. 1. Increase in thermogenesis: a. Shivering (shivering begins when tone increase over a threshold - feedback oscillation of the muscle spindle stretch reflex mechanism), b. Sympathetic excitation of heat production - sympathetic chemical excitation of heat production (-> uncoupling)(10-15% increase in adults, 100% infants), c. Thyroxine secretion (The thyroid gland needs several weeks to hypertrophy sufficiently) (Higher incidence of toxic thyroid goiters in people who live in cold climates) 2. Stop sweating 3. Peripheral vasoconstriction (Stimulation of the posterior sympathetic centers) 4. Piloerection (Not important in humans, allow animals to entrap insulator air) (Guyton) |
|
|
Fever - causes (3)
|
1. Bacterial diseases
2. Brain lesions (Neurosurgeon touching hypothalamus, compression of hypothalamus by brain tumor) 3. Environmental conditions -> heatstroke (Guyton) |
|
|
Resetting the hypothalamic temperature-regulating centers in febrile diseases
a. Caused by which substances? examples? b. Mechanism |
a. Pyrogens
1. Many proteins and breakdown products of proteins 2. Lipopolysaccharide toxins from bacterial cell membranes (Only need ng of lipopolysaccharide) b. Some can act directly and some indirectly. Indirect way: 1. Endotoxins (gram -) -> 2. Phagocytosed by neutrohpils, macrophages, T lymphocytes -> release IL-1\Leukocyte pyrogen\endogenous pyrogen -> 3. Induce formation of prostaglandin E2 in hypothalamus -> fever (Explain function of aspirin as antipyretic) (Guyton) |
|
|
Chills and crisis\flushing
a. Mechanism of chills b. Mechanism of crisis\flushing |
a. Set-point is increased by pyrogen -> delay of a couple of hours before the new temperature is reached. Temperature below the new set-point cause feelings of cold.
(Skin becomes cold due to vasoconstriction)(Continue till the body reach the set-point or until the pyrogen stop havinge effect) b. Opposite. Sudden removal of stimuli for increased set-point -> delay for reduction to normal temperature. Feel warm, sweat to reduce temperature. (Guyton) |
|
|
Heatstroke
a. Depend on b. Critical body temperature threshold c. S&S (4) |
a. Depdent on
1. Humidity of air (Can withstand 54 C in low humidity, 34 C in high humidity) 2. Work performed (Can happen in as low as 29.5 C during heavy work) b. 40.5 C c. S&S 1. Dizziness 2. Abdominal distress with N&V 3. Hypovolemic shock 4. Delirium, LOC (Guyton) |
|
|
Harmful effects of high temperature
|
Local hemorrhages and parenchymatous (distinguishing\specific cell of an organ) degeneration of cells throughout the body, especially in the brain.
(Liver, kidneys can be damaged enough to cause organ failure) (Guyton) |
|
|
Why is temperature regulation lost at low temperatures (2)
|
The hypothalamus lose its ability to regulate the temperature below 29 C (start to lose its function at 34 C). <-
1. The rate of chemical heat production in each cell is depressed almost twofold for each 10 F decrease in body temperature. 2. Sleepiness followed by coma which depresses the activity of the CNS control mechanisms and prevent shivering. (Guyton) |
|
|
Neuron
a. Number of neurons in the central nervous system b. Number of synaptic connections per neuron c. Size of synaptic cleft |
a. More than 100 billion
b. Only a few to 200 000 (80-95% on dendrites, the rest on soma) c. 20-30 nm (Guyton) |
|
|
Levels of the central nervous system from which skeletal muscles can be controlled (5)
|
1. The spinal cord
2. The reticular substance (medulla, pons, mesencephalon) 3. The basal ganglia 4. The cerebellum 5. The motor cortex (Guyton) |
|
|
Major human evolutionary levels of the central nervous system (3)
|
1. The spinal cord level
(Control centers of the cord can cause walking movements, reflexes that withdraw portions of the body from painful objects, reflexes that stiffen the legs to support the body against gravity, reflexes that control local blood vessels, GI movements, or urinary excretion) 2. The lower brain\Subcortical level (Most subconscious activities: respiratory, vasomotor, equilibrium, feeding reflexes, emotional patterns: anger, excitement, sexual response, reaction to pain and pleasure) (Medulla, pons, mesencephalon, hypothalamus, thalamus, cerebellum, basal ganglia) 3. The higher brain or cortical level (Extremely large memory storehouse, newer functions alone, without the cerebral cortex, the functions of the lower brain centers are often imprecise, thought processes) (Guyton) |
|
|
Presynaptic terminal - synonym (5)
|
1. Terminal knobs
2. Terminal boutons 3. Axon terminals 4. Synaptic knobs 5. End-feet (Guyton, Stedman) |
|
|
General components of receptor proteins on the postsynaptic neurons
|
1. A binding component
2. An ion channel or a second messenger activator (Guyton) |
|
|
Why does not cations pass through the anion channels?
|
Sodium, potassium, and calcium are blocked, mainly because their hydrated ions are too large to pass.
(Cation channels block anions due to their negative charge) (Guyton) |
|
|
Excitatory receptors can cause excitation by which mechanisms (3)
|
1. Increased sodium ion conduction.
2. Decreased chloride and potassium ion conduction. 3. Various changes in the internal metabolism of the postsynaptic neuron to a. Excite cell activity b. Increase the number of excitatory membrane receptors c. Decrease the number of inhibitory membrane receptors (Guyton) |
|
|
Small-molecule rapid acting synaptic transmitters
a. Class I (1) b. Class II - The amines (5) c. Class III - Amino acids (4) d. Class IV (1) |
a. Acetylcholine
b. 1. Norepinephrine 2. Epinephrine 3. Dopamine 4. Serotonin 5. Histamine c. 1. Gamma-aminobutyric acid (GABA) 2. Glycine 3. Glutamate 4. Aspartate d. Nitric oxide (They cause most of the acute responses of the nervous system - sensory, motor..) (Guyton) |
|
|
Neuropeptide, slowly acting transmitters or growth factors
a. 3 groups as examples b. Type of effect (3) |
a. Groups of neuropeptides, slowly acting transmitters, or growth factors
1. Hypothalamic-releasing hormones (TRH, LHRH, GHIH) 2. Pituitary peptides (ACTH, alpha-MSH, beta-endorphin, PRL, LH, thyrotropin, GH, ADH) 3. Peptides that act on gut and brain (Leucine-enkephalin, Methionine-enkephalin, substance P, gastrin, cholecystokinin, vasoactive intestinal peptide, nerve growth factor, brain-derived growth factor, neurotensin) b. More prolonged actions 1. Long-term changes in numbers of neuronal receptors 2. Long-term opening or closure of certain ion channels, and 3. Possibly long-term changes in number and size of synapses (Guyton) |
|
|
Small-molecule, rapidly acting synaptic transmitters
a. Typically synthesized in b. Characteristics of effect |
a. Cytosol
(And actively reabsorbed into vesicles) b. Usually increase or decrease conductance through ion channels, effect only lasts a millisecond or less. (Guyton) |
|
|
Acetylcholine
a. Produced by which enzyme where b. Degraded by which enzyme where c. Generally excitatory or inhibitory? d. Found where? (6) |
a. Choline acetyltransferase in cytosol.
b. Cholinesterase in proteoglycan reticulum of the synaptic cleft. (Choline is reabsorbed and recycled) c. Excitatory (Inhibitory on some of the parasympathetic nerve endings, ie. the heart) d. 1. Terminals of the large pyramidal cells from the motor cortex 2. Several different types of neurons in the basal ganglia 3. The motor neurons that innervate skeletal muscle 4. The preganglionic neurons of the autonomic nervous system 5. Cholinergic postsynaptic sympathetic neurons (ie sweat glands) 6. The postganglionic neurons of the parasympathetic nervous system (Guyton) |
|
|
Norepinephrine
a. Generally excitatory or inhibitory? b. Found where? (2) |
a. Excitatory with exceptions
b. 1. Terminals of many neurons whose cell bodies are located in the brain stem and hypothalamus - specifically the norepinephrine-secreting neurons in the locus ceruleus (blue) in the pons (send nerve fibers to widespread areas of the brain to help control overall activity and mood - ie level of wakefulness 2. Most postganglionic neurons of the sympathetic nervous system (Guyton) |
|
|
Characteristics of various small-molecule transmitters
a. Dopamine - location (1), effect b. Glycine - location (1), effect c. GABA, location (4), effect |
a. Neurons that originate in the substantia nigra
(-> striatal region of the basal ganglia) Mostly inhibition b. Synapses in the spinal cord, always inhibitory c. Always inhibitory Nerve terminals in 1. Spinal cord 2. Cerebellum 3. Basal ganglia 4. Many areas of the cortex (Guyton) |
|
|
Characteristics of various small-molecule transmitters
a. Glutamate - location (2), effect b. Serotonin - location (1), effect c. Nitric oxide - location (1) |
a. Always excitatory
1. Terminals of many of the sensory pathways entering the central nervous system 2. Many areas of the cerebral cortex b. Inhibitory 1. Neurons of nuclei of median raphe of the brain stem (-> many brain and spinal cord areas - dorsal horns of the spinal cord, hypothalamus. Inhibitory of pain pathways in the cord, inhibitory effect in higher regions is linked to control mood and perhaps sleep) c. 1. Nerve terminals in areas of the brain responsible for long-term behavior and memory (Unique in its mechanism of formation (not stored, synthesized rapidly as needed) and in its actions on the postsynaptic neuron (diffuse into postsynaptic neurons nearby, diffuse through the presynaptic membrane in a matter of seconds)(don't greatly change membrane potential, instead changes intracellular metabolic functions that modify neuronal excitability for seconds, minutes, or maybe even longer) (Guyton) |
|
|
Neuropeptides
a. Mechanism of synthesis b. Actions (4) |
a. Synthesis of neuroeptides
1. Synthesized as integral parts of larger protein molecules on RER 2. Transported to the Golgi apparatus, where a. Split into smaller fragments: the neuropeptide itself or a precursor b. Packaged into vesicles 3. Transported through the axon by axonal streaming (few cm\day) (Release neurotransmitter in the same manner as small molecule rapid-acting synaptic transmitters, however, vesicle is autolyzed and not reused) (Less is released, but the potency is higher and the duration of action is longer) b. Often more prolonged actions 1. Prolonged closure of calcium channels 2. Prolonged changes in the metabolic machinery of the cell 3. Prolonged changes in activation or deactivation of specific genes 4. Prolonged alterations in numbers of excitatory or inhibitory receptors (Can last for months or years) (Guyton) |
|
|
Concentration differnces of ions across the neuronal somal membrane
a. Resting membrane potential b. Nernst potential - what? equation? c. Sodium - concentration outside, inside, Nernst potential, diffuse which way when conductivity is increased d. Potassium - concentration outside, inside, Nernst potential, diffuse which way when conductivity is increased e. Chloride ions - concentration inside, outside, Nernst potential, diffuse which way when conductivity is increased |
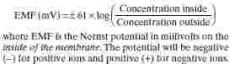
a. -65 mV
b. Nernst potential for a ion: a potential that exactly opposes movement of an ion c. 135-145 mM, 14 mM, +61 mV, in (to become closer to Nernst potential) d. 4.5 mM, 120 mM, -86 mV, out (to become closer to its Nernst potential) e. 107 mM, 8 mM, -70 mM, In (to become closer to its Nernst potential) (Guyton) |
|
|
Excitatory postsynaptic potential (EPSP)
a. What b. Transmitter substances released by a single terminal cause an EPSP of? c. Duration of opening of channels, time neded for them to be pumped back again |
a. The change in potential that is produced in the membrane of the next neuron when an impulse that has an excitatory influence arrives at the synapse.
It is a local change in the direction of depolarization. (A summation of these can lead to an action potential) b. 0.5-1 mV (Need 20 mV to reach threshold for firing) c. 1-2 ms, 15 ms (Explains why temporal summation is possible) (Guyton) |
|
|
Generation of action potential from excitatory postsynaptic potential
a. Where is it usually generated? b. Why? c. How large must the EPSP usually be? |
a. Initial segment of axon
(From electrotonic current (direct spread of electrical current by ion conduction in the fluids of the dendrites but without generation of action potentials) mainly from the dendrites (80-95% of synapses) b. 7x the density of voltage-gated sodium channels (Also explains the forward direction of the action potential) c. +20 mV (+30-40 mV on soma) (Guyton) |
|
|
Presynaptic inhibition
a. Mechanism b. Especially prevalent where, why |
a. Caused by release of an inhibitory substance (mostly GABA which open anion channels) onto the outsides of the presynaptic nerve fibrils proximal to the nerve terminals -> Inhibit synaptic transmission by canceling out much of the excitatory effect of the inward flow of sodium ions that enter the terminal fibrils when an action potential arrives.
b. Many of the sensory pathways. Inhibiting nearby nerve fibers minimize sideways spread and mixing of signals. (Guyton) |
|
|
Neural characteristics
a. Facilitation of neurons b. Decremental conduction |
a. The phenomenon when the summated postsynaptic potential is excitatory but has not risen high enough to reach the threshold for firing by the postsynaptic neuron.
(Diffuse signals in the nervous system often facilitate large groups of neurons so they can respond quickly and easy to signals arriving from other sources) b. Refers to the decrement of electrotonic conduction in the dendrites - the farther the excitatory synapse is from the soma, the greater will the decrement be. Due to ionic leakage through the membrane. (Guyton) |
|
|
Fatigue of synaptic transmission
a. What b. Cause\Mechanism (3) c. Importance |
a. The decrease in firing of a postsynaptic neuron in response to repetitive stimuli at a rapid rate.
b. 1. Depletion of neurotransmitters (Many neurons only contain 10 000 vesicles, these can be depleted in seconds to minutes) 2. Progressive inactivation of many of the postsynaptic membrane receptors 3. Slow development of abnormal concentrations of ions inside the postsynatpic neuronal cell c. Probably the most important means by which the excess excitability of the brain during an epileptic seizure is finally subdued. (Guyton) |
|
|
Synaptic transmission
a. Effect of pH on synaptic transmission b. Effect of hypoxia on synaptic transmission c. Drugs which increase excitability d. Drugs which decrease synaptic transmission |
a. Normally, alkalosis greatly increases neuronal excitability while acidosis greatly depress neuronal activity.
(Alkalosis and cerebral epileptic seizure generation) b. A few seconds of hypoxia can cause complete inexcitability of some neurons. (Ie temporarily disruption of cerebral blood flow for 3-7 seconds cause LOC) c. Drugs which increase excitability I. Increase excitability by reducing threshold for firing: caffeine, theophylline, theobromine II. By inhibiting glycine (inhibitory): strychnine (Cause severe tonic muscle spasms) d. Most anesthetics increase the neuronal membrane threshold for excitation (Since many of them are very lipid-soluble, it has been reasoned that some of them might change the physical characteristics of the neuronal membranes, making them less responsive to excitatory agents) (Guyton) |
|
|
Synaptic delay
a. What b. Minimal period of synaptic delay |
a. The time from transmission of a neuronal signal from a presynaptic neuron to a postsynaptic neuron
b. 0.5 ms (-> Neurophysiologists can use this to estimate number of neurons in series in a circuit) (Guyton) |
|
|
Classification of sensory receptors - there are five basic types of sensory receptors. List the subgroups of these
I. Mechanoreceptors (5) II. Thermoreceptors (2) III. Nocireceptors (1) IV. Electromagnetic receptors (1) V. Chemoreceptors (6) (Guyton) |
I. Mechanoreceptors
1. Skin tactile sensibilities (In epidermis and dermis) (Free nerve endings, expanded tip endings, spray endigns, Ruffini's endings, ecapsulated endings, hair end-organs) 2. Deep tissue sensibilities (Free nerve endings, expanded tip endings, spray endings, encapsulated endings, muscle spindles) 3. Hearing - sound receptors of cochlea 4. Equilibrium - vestibular receptors 5. Arterial pressure - baroreceptors of carotid sinuses and aorta II. Thermoreceptors 1. Cold - cold receptors 2. Warmth - warmth receptors III. Nocireceptors 1. Pain - free nerve endings IV. Electromagnetic receptors 1. Vision - rods and cones V. Chemoreceptors 1. Taste - receptors of taste buds 2. Smell - receptors of olfactory epithelium 3. Arterial oxygen - receptors of aortic and carotid bodies 4. Osmolality - neurons in or near supraoptic nuclei 5. Blood CO2 - receptors in or on surface of medulla and in aortic and carotid bodies 6. Blood glucose, amino acids, fatty acids - receptors in hypothalamus (Guyton) |
|
|
Classification of sensory receptors - there are five basic types of sensory receptors. List the subgroups of these
I. Mechanoreceptors (5) II. Thermoreceptors (2) III. Nocireceptors (1) IV. Electromagnetic receptors (1) V. Chemoreceptors (6) (Guyton) |

I. Mechanoreceptors
1. Skin tactile sensibilities (In epidermis and dermis) (Free nerve endings, expanded tip endings, spray endigns, Ruffini's endings, ecapsulated endings, hair end-organs) 2. Deep tissue sensibilities (Free nerve endings, expanded tip endings, spray endings, encapsulated endings, muscle spindles) 3. Hearing - sound receptors of cochlea 4. Equilibrium - vestibular receptors 5. Arterial pressure - baroreceptors of carotid sinuses and aorta II. Thermoreceptors 1. Cold - cold receptors 2. Warmth - warmth receptors III. Nocireceptors 1. Pain - free nerve endings IV. Electromagnetic receptors 1. Vision - rods and cones V. Chemoreceptors 1. Taste - receptors of taste buds 2. Smell - receptors of olfactory epithelium 3. Arterial oxygen - receptors of aortic and carotid bodies 4. Osmolality - neurons in or near supraoptic nuclei 5. Blood CO2 - receptors in or on surface of medulla and in aortic and carotid bodies 6. Blood glucose, amino acids, fatty acids - receptors in hypothalamus (Guyton) |
|
|
Nocireceptors detect
|
Damage occurring in the tissues - whether physical or chemical damage.
(Guyton) |
|
|
Mechanoreceptors - subgroups
a. Skin tactile sensibilities (epidermis and dermis) (6) b. Deep tissue sensibilities (5) c. The three remaining groups |

a.
1. Free nerve endings 2. Expanded tip endings (Merkel's discs, several others) 3. Spray endings 4. Ruffini's endings 5. Encapsulated endings (Meissner's corpuscles, Krause's corpuscles) 6. Hair end-organs b. 1. Free nerve endings 2. Expanded tip endings 3. Spray endings (Ruffini's corpuscles) 4. Encapsulated endings (Pacinian corpuscles, a few other variants) 5. Muscle endings (Muscle spindles, Golgi tendon receptors) c. 1. Hearing (sound receptors of cochlea) 2. Equilibrium (vestibular receptors) 3. Arterial pressure (baroreceptors of carotid sinuses and aorta) (Guyton) |
|
|
Receptor potential
a. What b. Elicited by what, how (4)? |
a. The change in electrical potential of a sensory receptor elicited by its stimulus.
(Stimulate a action potential if it rise above threshold for firing, increased receptor potential over this point increase frequency of action potentials) b. 1. Mechanical deformation of the receptor - stretch the receptor membrane and open ion channels 2. Application of a chemical to the membrane - opens ion channels 3. By change of temperature of the membrane - alters the permeability of the membrane 4. By the effect of electromagnetic radiation - directly or indirectly changes the receptor membrane characteristics (Guyton) |
|
|
Adaptation of receptors
a. What b. Which group of receptors adapt completely? c. Which groups of receptors adapt partially? d. What is the mechanism for adaptation for mechanoreceptors (2) |
a. A characteristic of all sensory receptors. All adapt either partially or completely to any constant stimulus after a period of time.
(That is, when a continuous sensory stimulus is applied, the receptor responds at a high impulse rate at first and then at a progressively slower rate until finally the rate of action potentials decreases to very few or often to none at all) b. Mechanoreceptors (Pacinian corpuscle after ms, 2 days for many carotid and aortic baroreceptors) c. Chemo- and nocireceptors d. Twofold 1. Readjustments in the structure of the receptor itself 2. Electrical accommodation in the terminal nerve fibril by closure of sodium channels induced by continuous flow through them (Guyton) |
|
|
Slowly and rapidly adapting receptors
a. Slow adapting receptors - synonym, examples (4) b. Rapid adapting receptors - synonym, example |
a. Tonic receptors (detect continuous stimulus)
1. Receptors of the macula in the vestibular apparatus 2. Pain receptors 3. Baroreceptors of the arterial tree 4. Chemoreceptors of the carotid and and aortic bodies b. Rate\Movement\Phasic receptors (respond to changes in stimuli) 1. Pacinian corpuscles 2. Receptors of the semicircular canals in the vestibular apparatus 3. Joint receptors (Allows one to predict the state of the body ahead of time. Ie joint receptors allow the nervous system to predict where the feet will be during any precise fraction of the next second) (Guyton) |
|
|
Nerve fibers
a. Range of diameter b. Range of conducting velocity c. General classification of nerve fibers - groups and subgroups |
a. 0.5-20 um
b. 0.5-120m\s c. Type A (2-20 um, 2-120 m\s) alpha, beta, gamma, delta Type C (0.5-2 um, 05.2m\s) |
|
|
Classify the following sensory and motor functions into the general and alternative classification of nerve fibers
a. Muscle spindle (primary ending\annulospiral endings) b. Muscle tendon (Golgi tendon organ) c. Skeletal muscle d. Hair receptors e. Vibration (pacinain corpuscle) f. High discrimination touch (Meissner's corpuscle) |

a. Aalpha, IA
b. Aalpha, IB c. Aalpha\Abeta, I\II d. Aalpha\Abeta, I\II e. Aalpha\Abeta, I\II f. Aalpha\Abeta, I\II (Guyton) |
|
|
Group II (Sensory nerve classification)\Abeta and gamma nerve (General classification) fibers - members (2)
|

1. Most discrete cutaneous tactile receptors
2. Flower-spray endings of the muscle spindles (Guyton) |
|
|
Group III (Alternative sensory classification) and group Adelta (General classification) of nerve fibers. Members (3)
|

Fibers carrying
1. Temperature 2. Crude touch 3. Pricking pain sensations (Myelinated, 2-5 um, 6-30m\s) (Guyton) |
|
|
Group IV\Type C nerve fibers - members (4)
|

Fibers carrying
1. Pain 2. Itch 3. Temperature 4. Crude touch sensations (Unymelinated, 0.5-2 um, 0.5-2 m\s) (Guyton) |
|
|
Neuronal pool
a. What b. Examples (3) b. What is a stimulatory field |
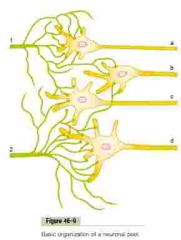
a. A group of interconnected neurons with specific functions.
(Have input and output part) b. 1. The cerebral cortex 2. The gray matter of the spinal cord 3. The specific nuclei in the thalamus, cerebellum, pons, medulla c. The neuronal area stimulated by each incoming nerve fiber (Most on the nearest neurons. Progressively fever nerve terminals lie on the neurons farther away) (Guyton) |
|
|
Facilitated and discharge zone
a. Discharge zone b. Facilitated zone |
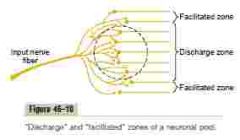
a. Discharge\Excited\Liminal (limin: threshold)\Suprathreshold zone
The area which an input neuron project to where it can elicit an action potential on its own b. Facilitated\Subthreshold\Subliminal zone The area to which an input neuron projects to, in which it does not have enough nerve terminals to elicit an action potential, only facilitate the next neuron. (Also inhibitory zone in the case of inhibitory neuronal branches) (Guyton) |
|
|
Relaying of signals through neuronal pools
a. Amplifying divergence - what, example b. Divergence into multiple tracts - what, example c. Convergence from a single source d. Convergence from multiple sources e. Reciprocal inhibition - what, example (Guyton) |

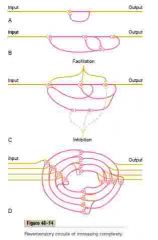
a. Amplifying divergence
I. An input signals spreads to an increasing number of neurons as it passes through successive orders of neurons in its path. II. Ie. corticospinal pathway where a large pyramidal cell of the motor cortex can excite up to 10 000 muscle fibers. b. Divergence into multiple tracts I. The signal is transmitted in two directions. II. Ie. Sensory information to thalamus -> 1. Discrete regions of cerebral cortex 2. Deeper structures of the thalamus c. Convergence from a single source I. Multiple terminals from a single incoming fiber tract terminate on the same neuron. (Spatial summation -> action potential generation from single incoming fiber) d. Convergence from multiple soruces I. Signals from multiple terminals of different neurons unite to excite a single neuron. (Motor neurons <- converging of interneurons <- Interneurons of spinal cord receive 1. Peripheral nerve fibers 2. Propriospinal fibers passing from one segment of the cord to another 3. Corticospinal fibers 4. Several other long pathways descending from the brain) e. Reciprocal inhibition I.Incoming signal both excite and inhibit. II. Characteristic for innervation of antagonistic pairs of muscles. (Achieved by stimulating an inhibitory interneuron which furher inhibits the antagonist alpha motor fibers) (Guyton) |
|
|
How is prolongation of a signal by a neuronal pool achieved?
|
1. Synaptic afterdischarge
I. Due to the duration of the postsynaptic electrical potential. The longer it is, the more action potentials it can generate. (Longer with some of the long-acting synaptic transmitters) 2. Reverberatory (gjenklang)\Oscillatory circuit I. Caused by positive feedback within the neuronal circuit that feeds back by collateral branches to re-excite the input of the same circuit (The intensity of the output signal usually increases to a high value early in reverberation and then decreases to a critical point, at which it suddenly ceases entirely. Due to synaptic fatigue.) (Guyton) |
|
|
Mechanism for continuous signal output from some neuronal circuits (2)
|
1. Intrinsic neuronal excitability
(<- Membrane above to threshold for firing, frequency of action potentials generated is also an variable intrinsic value) 2. Reverebrating circuits (If it is not active enough to fatigue) (Ie. vascular tone, gut tone, degree of constriction of the iris in the eye, controlled by inhibitory and excitatory autonomic nervous system stimuli) (Both are regulated by inhibitory and excitatory stimuli) (Guyton) |
|
|
Rhythmical signal output
a. Cause b. Example |
a. Most are caused by reverberating circuits
b. Rhythmical respiratory signal from respiratory centers of the medulla and pons (Regulated by inhibitory and excitatory influences) (Guyton) |
|
|
How does the central nervous system prevent mass reverberatory cycles of re-excitation as happens during an epileptic seizure (2)?
|
1. Inhibitory circuits
(a. Inhibitory feedback circuits that return from the termini of pathways back to the initial excitatory neurons of the same pathways b. Some neuronal pools that exert gross inhibitory control over widespread areas of the brain - many of the basal ganglia over muscle control) 2. Fatigue of synapses (Automatic short-term adjustment of pathway sensitivity by the fatigue mechanism of transmitter substance, long-term changes in synaptic sensitivity caused by automatic downregulation or upregulation of synaptic receptors) (Guyton) |
|
|
Propriocetive sensations
a. What b. Components (4) |
a. Those sensations having to do with the physical state of the body
b. 1. Joint position sensations 2. Tendon and muscle sensations 3. Pressure sensations from the bottom of the feet 4. Sense of equilibrium (Guyton) |
|
|
Tactile sensation
a. Subcategories (4) b. Tactile receptors (6) |

a. Tactile sensations
1. Touch (<- stimulation of tactile receptors in the skin or in tissues immediately beneath the skin) 2. Pressure (<- Deformation of deeper tissues) 3. Vibration (<- Rapidly repetitive sensory signals, some of the same types of receptors as those for touch and pressure are used) 4. Tickle senses b. Tactile receptors 1. Free nerve endings (Skin and many other tissues, <- touch and pressure) 2. Meissner's corpuscle (<- Touch, encapsulated, Abeta sensory fiber, non-hairy parts of skin, very fast adapting) 3. Expanded tip tactile receptors - ie Merkel's discs (<- touch, skin, slower to adapt -> steady-state signals, Abeta nerve fiber, part of Iggo dome receptor, localize touch and determine texture) 4. Hair end-organ (<- Movement of hair (<- movement of objects on the surface, initial contact), adapts fast) 5. Ruffini's end-organs (Deeper layer of skin and deeper internal tissue, multibranched and encapsulated, adapt very slow, <- continuous state of deformation - heavy prolonged touch and pressure) 6. Pacinian corpuscles (beneath skin and in fascial tissue, <- rapid local compression (tissue vibration), adapt fast) (Guyton) |
|
|
Free nerve endings
a. Location b. Stimuli c. Nerve fiber type |

a. Everywhere in the skin and in many other tissues
b. Touch and pressure c. Adelta\III (5-30m\s) and C\IV (0.5-2m\s)(-> spinal cord\lower brain stem, tickle sensation) (Only receptor on cornea, but can trigger touch and pressure sensation) (Guyton) |
|
|
Meissner's corpuscle
a. Location b. Stimuli c. Structure d. Characteristics e. Nerve fiber type |

a. Nonhairy parts of the skin - especially fingertips, lips
(Where one's ability to discern spatial locations of touch sensation is highly developed) b. Touch c. Encapsulated nerve ending (Many terminal nerve filaments inside the capsule) d. Rapidly adapting (Fraction of a second -> sensitive to movement of objects over the surface of the skin as well as to low frequency vibration) e. Type Abeta (Most specialized sensory receptors: Meissner's corpuscles, Iggo dome receptors, hair receptors, pacinian corpuscles, Ruffini's endings) (30-70m\s) (Guyton) |
|
|
Expanded tip tactile receptors
a. Example b. Location c. Characteristic d. Nerve fiber type |

a. Merkel's discs (Iggo dome receptor is groups of Merkel's disc domed superficially in the skin)
b. Skin - hair and nonhairy, in receptor organ called the Iggo dome receptor. (This projects upward against the underside of the epithelium -> dome -> extremely sensitive receptor) c. Slow partially adapting signal (-> Steady-state signals that allow one to determine continuous touch of objects) d. Type Abeta (Most specialized sensory receptors: Meissner's corpuscles, Iggo dome receptors, hair receptors, pacinian corpuscles, Ruffini's endings) (30-70m\s) (Guyton) |
|
|
Ruffini's end-organs
a. Stimuli b. Location (3) c. Structure d. Characteristics e. Nerve fiber type |
Ruffini's end-organs
a. Prolonged touch and pressure signals b. Location 1. Deeper layers of skin 2. Deeper internal tissues 3. Joint capsule (signal degree of joint rotation) c. Multibranched, encapsulated endings d. Adapt very slow e. Type Abeta (Most specialized sensory receptors: Meissner's corpuscles, Iggo dome receptors, hair receptors, pacinian corpuscles, Ruffini's endings) (30-70m\s) (Guyton) |
|
|
Vibration
a. Detection by which group of receptors b. Which are most sensitive at 30-800 Hz c. Which are most sensitive at 2-80 Hz |
a. Tactile
b. Pacinian corpuscles (Encapsulated ending in deeper organs) c. Meissner's corpuscles (Encapsulated ending in skin) (Guyton) |
|
|
Type C\IV nerve fibers
a. Size & conduction velocity b. Include (6) |
a. 0.5-2 um, 0.5-2 m\s
b. Sensory 1. Crude touch and pressure 2. Tickle (distinct free nerve endings) 3. Aching pain 4. Cold 5. Warmth Motor 6. Sympathetic (Guyton) |
|
|
Dorsal column-Medial lemniscal system
a. Pathway b. Characteristics - speed, myelination, other c. Components (3) d. Spatial orientation of the nerve fibers - dorsal column, ventrobasal complex |
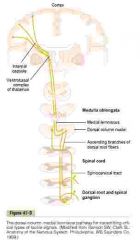
a. Dorsal column-medial lemniscal system - Pathway
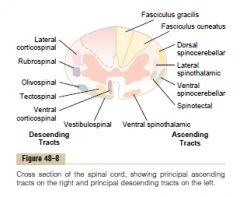
1. Sensory information -> dorsal sensory root -> 2. Dorsal horn of spinal cord -> 3. Dorsal columns -> (Lower extremity in fasciculus gracilis, upper extremities in fasciculus cuneatus) 4. Synapse in dorsal medulla in the dorsal column nuclei (cuneate and gracile nuclei)(2nd order neurons)-> 5. Decussate -> 6. Medial lemniscus -> 7. VPL of thalamus -> third order nerve fibers -> 8. Postcentral gyrus of the cerebral cortex (Somatic sensory area I)(also smaller area in the lateral parietal cortex called somatic sensory area II) (Lemniscus: a bundle of nerve fibers ascending from sensory relay nuclei to the thalamus) b. Characteristics 1. Large, myelinated 2. 70-110m\s 3. High degree of spatial orientation c. Components 1. Fine touch sensation and pressure (Requiring a high degree of localization of the stimulus and touch sensations requiring transmission of fine gradations) 2. Phasic (fast-adapting) sensations - vibratory sensations 3. Position sensations from the joints d. Spatial orientation of nerve fibers I. Dorsal column: fibers from the lower parts of the body lie more centrally, while those that enter at progressively higher levels lie more peripherally. II. Ventrobasal complex: opposite -> lateral: caudal portions, central: cranial portions (Guyton) |
|
|
Sensory pathways for transmitting somatic signals into the central nervous system
a. From the entry point into the spinal cord and then to the brain, the sensory signals are carried through one of two alternative sensory pathways b. Where do these partially unite? |
a.
1. The dorsal column-medial lemniscal system 2. The anterolateral system b. Thalamus (Guyton) |
|
|
Anterolateral system - sensory pathway
a. Pathway b. Characteristics - myelination, speed, others (6) c. Components (4) |
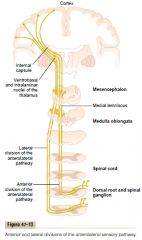
a. Anterolateral system - Pathway
1. Sensory information -> dorsal root -> synapse in dorsal horns of the spinal gray matter (at dorsal horn laminae I, IV, V, VI) -> 2.Decussate immediately in the anterior commissure of the cord to the opposite anterior and lateral white columns -> 3. Ascend through anterior spinothalamic and lateral spinothalamic tracts -> 4. Lower brain stem (reticular nuclei) and thalamus (ventrobasal complex, intralaminar nuclei. Converge with dorsal column-medial lemniscal system) (most pain signals go to reticular nuclei -> intralaminar nuclei) b. Characteristics 1. Myelinated (but smaller than dorsal column-medial lemniscal system) 2. 8-40 m\s (One half-One third of dorsal columns) 3. Low degree of spatial orientation (Thus tend to transmit information that does not need to be transmitted rapidly or with great spatial fidelity) 4. Can transmit a broad spectrum of sensory modalities (pain, warmth, cold, crude tactile) 5. Gradations of intensities are far less accurate than in the dorsal columns-medial lemniscal system (Most have 10-20 gradiations of strength as opposed to as many as 100 gradiations in the dorsal column system) 6. The ability to transmit rapidly changing or rapidly repetitive signals is poor c. 1. Pain 2. Thermal sensations - both warmth and cold sensations 3. Crude touch and pressure sensations (Capable only of crude localizing ability on the surface of the body) 4. Sexual sensations (Guyton) |
|
|
Somatosensory areas
a. Primary somatosensory area I - include which of Brodmanns areas? b. Somatosesensory association area - include which of Brodmanns areas? |
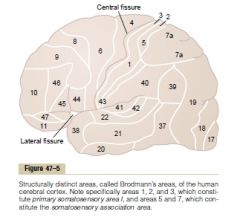
a. 1,2,3
b. 5,7 (Guyton) |
|

(I is closest to the surface)
Layers of the somatosensory cortex and their function a. Layer I and II b. Layer II and III c. Layer IV d. layer V and VI |

a. Layer I and II
I. <- Diffuse, non-specific input signals from lower brain centers II. Mainly controls the overall level of excitability of the respective regions stimulated b. Layer II, III I. The neurons send axons to related portions of the cerebral cortex on the opposite side of the brain through corpus callosum c. Layer IV I. The incoming sensory signals excites neuronal layer IV first -> spread d. Layer V and VI 1. Send axons to the deeper parts of the nervous system I. V is larger and project to more distant areas: basal ganglia, brain stem, spinal cord. Control signal transmission II. VI: -> thalamus. Help to control the sensory signals entering the thalamus) (Guyton) |
|
|
Functional units of the sensory cortex
a. What? b. Which are most anterior? c. Which are more posterior? d. Which are most posterior? |
a. Functionally, the neurons of the somatosensory cortex are arranged in vertical columns extending all the way through the six layers, each of these columns serves a single specific sensory modality.
b. Those involved with proprioception (muscle, tendon, and joint stretch receptors) (Brodmann 3a, close association with motor cortex, help control efferent motor signals) c. More posterior respond to slowly adapting cutaneous receptors c. Deep pressure (Guyton) |
|
|
Functions of somatosensory area I - as demonstrated by bilateral excision
|
1. Discrete localization of the different sensations (including pain)
(Can still localize crudely - thus this is a property of the brain stem, thalamus, or other parts of the cerebral cortex) 2. Judge critical degrees of pressure against the body and weight 3. Astereognosis\tactile agnosia - unable to judge shapes or forms of objects if this area is damaged (a-: stereos: solid, gnosis: knowledge) 4. Judge texture (Pain is still preserved in quality and intensity, but it is poorly localized) (Guyton) |
|
|
Two-point discrimination
a. What b. Strongly dependent on which phenomenon |
a. A method to test tactile discrimination, two needles are pressed lightly against the skin simultaneously, and the person determines if one or two stimulus are felt.
b. Lateral inhibition (With the dorsal column lateral inhibition occurs at the dorsal column nuclei of the medulla, the ventrobasal nuclei of the thalamus and the cortex itself.) (1-2 mm in finger, up to 70 mm on the back) (Guyton) |
|
|
Weber-Fechner principle
a. What b. Limited to |
a. The gradations of stimulus strength are perceived approximately in proportion to the logarithm of stimulus strength.
(ie increase 10x to double, the perceivable difference will be a constant ratio. Ie 1 g when holding 30 g, 10 g when holding 300 g) b. Higher intensities of visual, auditory, and cutaneous sensory experiences. (Basically, it emphasize that the greater the background sensory intensity, the greater the additional change must be for the psyche to detect the change.) (Guyton) |
|
|
Proprioceptive senses - static and dynamic
a. Depend on b. Position sensory receptors |
a. Depend on knowing the degree of angulation of all joints in all planes and their rates of change.
b. 1. Skin tactile receptors near the joints (Important in finger joints where these are abundant) 2. Deep receptors near the joints (Important virtually everywhere else) a. Muscle spindles - especially mid-range b. Pacinian corpuscles, Rufffini's endings, Muscle tendon receptors - extreme end of joint angulation (Due to stretching of these tissues) (The pacinian corpuscles and muscle spindles are especially adapt for detecting rapid rates of change.) (Guyton) |
|
|
Corticofugal signals
a. What b. Inhibitory, excitatory, or mixed c. Function (2) |
a. Signals transmitted from the cerebral cortex to the lower sensory relay stations (thalamus, medulla, spinal cord)
b. Almost completely inhibitory. c. Function 1. Decrease lateral spread of the sensory signals -> increase the degree of contrast in the signal pattern 2. Keeps the sensory system operating in an optimal range of sensitivity - not so low that the signals are ineffectual, nor so high that the system is swamped beyond its capacity to differentiate sensory patterns. (Used by all sensory systems) (Guyton) |
|
|
Fast and slow pain
Fast pain a. Felt within ...s b. Synonyms (4) c. Examples d. Deep, skin, or both parts of the body e. Transmitted by which type of nerve fiber Slow pain f. Begins after ..s, other temporal characteristic g. Synonym (5) h. Associated with i. Skin, deeper, or both j. Travel in which nerve fiber |
a. 0.1s
b. Fast\sharp\pricking\acute\electric pain c. Skin is cut with a knife, skin is acutely burned, skin is subjected to electric shock d. Only skin e. Type Adelta\III (6-30m\s) f. Begins after 1 second or more (Increase slowly over seconds to minutes) g. Slow\Slow burning\Aching\Throbbing\Nauseous\Chronic pain h. Tissue destruction i. Both j. Type C\IV (0.5-2m\s) (Transmitted by different conduction pathways) (Guyton) |
|
|
Pain receptors - free nerve endings
a. Widespread in superficial layers of the skin as well as in certain internal tissues ...(4)? b. Which three types of stimuli can excite pain receptors? c. Which of these is fast pain associated with? d. Slow pain? |
a. Periosteum, Peritoneum, Arterial wall, Falx and tentorium in the cranial vault.
b. 1. Mechanical 2. Thermal (>45 C) 3. Chemical c. Mechanical and thermal d. All three (The fact that the rate of tissue damage and not the total damage that has already occurred is the stimuli for pain is an important principle. <- Make a person counteract the cause before damage occurs) (Guyton) |
|
|
Pain receptors and their stimulation
a. Eliciting chemicals (7) b. Which substances enhance the sensitivity of pain endings but do not directly excite them? (2) c. Adaptive property of pain receptors |
a.
Mast cell secretions 1. Bradykinin (Many consider this to be the primary agent responsible for causing pain following tissue damage) 2. Serotonin 3. Histamine Intracellular 4. Potassium ions (Excitatory influence on nerve ending membrane) 5. Proteolytic enzymes (Proteolytic effect increase permeability of ions to nerve ending membrane) Others 6. Acetylcholine 7. Lactic acid (ischemia) b. 1. Prostaglandins 2. Substance P c. Adapt very little, not at all, or increase in sensitivity (hyperalgesia) (Evolutionary purpose) (Guyton) |
|
|
Fast pain
a. Pathway b. Capabiliy of localization, how (2) c. Probable neurotransmitter |

a. Pathway
1. Adelta neuron -> 2. Lamina I (lamina marginalis of the dorsal horns) -> 3. Neospinothalamic tract which decussate immediately through the anterior commissure -> 4. Anterolateral columns -> 5a. VPL of thalamus (with DCML system) - Spinothalamic 5b. The reticular nuclei of the brain stem - Spinoreticular 5c. The posterior nuclear group of the thalamus (->other basal areas of the brain, somatosensory cortex) b. High. I. Adelta\III nerve fibers (C\IV in slow pain) II. Helped by accompanying tactile receptors. c. Glutamate (Duration of only a few milliseconds) (Guyton) |
|
|
Slow pain
a. Name of pathway - route b. Probably neurotransmitter c. Capability of localization, why |

a. Paleospinothalamic pathway (paleo: old\primitive)
1. Type C\IV fibers (some Adelta as well) -> 2. Substantia gelatinosa (laminae II, III of dorsal horn) -> 3. Interneurons -> 4. Lamina V -> decussate through anterior commissure -> 5. Anterolateral pathway -> 6a. Thalamus (10-40%) Brain stem areas 6b. Reticular nuclei of the brain stem 6c. The tectal area of the mesencephalon (Deep to the inferior and superior colliculi) 6d. The periaqueductal gray region (Brain stem areas -> intralaminar and ventrolateral nuclei of thalamus -> hypothalamus, basal regions of the brain) (Brain stem areas seem to be responsible for perception of this type of pain) b. Substance P (Substance P is released slowly, building up in concentration over a period of seconds to minutes) (Type C\IV secrete both glutamate and substance P - double pain sensation) c. Poor (Usually only to major part of the body - arm, stomach) I. Multisynaptic II. Diffuse connectivity III. Low myelin content (Guyton) |
|
|
Appreciation of pain
a. Role of reticular formation, thalamus and other lower brain centers b. Role of cerebral cortex |
a. Cause conscious perception of pain
(Complete removal of sensory cortex of an animal don't remove its ability to perceive pain) (Electrical stimulation in the reticular areas of the brain stem and in the intralaminar nuclei of the thalamus (the areas where the slow-suffering type of pain terminates, has a strong arousal effect on nervous activity throughout the entire brain. <- Part of arousal system. -> Virtually impossible to sleep when in severe pain) b. Believed to interpret pain quality (Guyton) |
|
|
Why is a anterolateral cordotomy to relieve pain not always successful? (2)
|
1. Many pain fibers from the upper part of the body do not decussate until they have reached the brain, so that the cordotomy don't transect these fibers.
2. Pain frequently returns several months later, partly as a result of sensitization of other pathways that normally are too weak to be effectual (ie sparse pathways in dorsolateral cord). (Guyton) |
|
|
Analgesia system in the brain and spinal cord
a. The three major components b. Involved neurotransmitters c. Which areas can stimulate the first part of the analgesic pathway? |
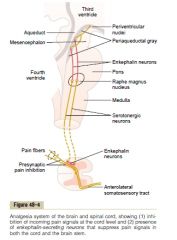
a. The three major components
1. Periaqueductal gray and periventricular areas of the mesencephalon and upper pons. Neurons project to -> 2. Neurons of raphe magnus nucleus (thin midline nucleus in the lower pons and upper medulla) and nucleus reticularis paragigantocellularis (laterally in medulla) -2nd order signal--> 3. Pain inhibitory complex in dorsal horns of spinal cord b. Involved neurotransmitters 1. Enkephalin: I. Nuclei of periventricular nuclei and periaqueductal gray area II. Interneurons of inhibitory complex in the dorsal horns of the spinal cord (Enkephalin have both pre- and postsynaptic inhibition of incoming type Adelta and C) 2. Serotonin - Raphe magnus fibers c. Which areas can stimulate the first part of the analgesic pathway 1. Periventricular nuclei in the hypothalamus 2. MFB from hypothalamus (Electrical stimulation in periaqeductal gray area or in the raphe magnus nucleus is analgesic) (Guyton) |
|
|
Brain's opiate system
a. Which (4) b. Derived from what (3) c. Act where (2) |
a. Endogenous opioids
1. Beta-endorphin (Hypothalamus, pituitary gland) 2. Met-enkephalin 3. Leu-enkephalin (Both enkephalins found in brain stem and spinal cord) 4. Dynorphin (Same areas as enkephalins but in lower quantities, 17 AAs, contain leukenkephalin) b. Breakdown of 1. Proopiomelanocortin (POMC) (-> Beta-endorphin, met-enkephalin) 2. Proenkephalin 3. Prodynorphin c. Act where 1. Periventricular nucleus and periaqueductal grey area 2. Dorsal horns of the spinal cord (Enkephalins: pentapeptide endorphins, found in many parts of the brain, Metenkephalin: Tyr-Gly-Gly-Phe-Met, Leu-enkephalin: Tyr-Gly-Gly-Phe-Leu, Proenkephalin: Tyr-Gly-Gly-Phe-Pro) (Guyton) |
|
|
Mechanism of referred pain
|
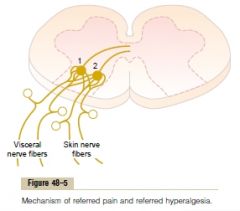
Branches of visceral pain fibers synapse in the spinal cord on the same second-order neurons (1 and 2) that receive pain signals from the skin.
When the visceral pain fibers are stimulated, pain signals from the viscera are conducted through at least some of the same neurons that conduct pain signals from the skin, and the person has the feeling that the sensation originates in the skin itself. (Guyton) |
|
|
Viscera insensitive to pain - which, compensated by
|
1. Liver.
Capsule and bile ducts are sensitive to pain. 2. Lung alveoli Parietal pleura and bronchi are sensitive to pain. (Guyton) |
|
|
Cramps
a. What b. Causes (7) |
a. Spasmic pain of a hollow viscus which occurs each time a peristaltic wave travels along an overly excitable part of a tube.
b. Overly excitable from 1. Appendicitis 2. Gatroenteritis 3. Constipation 4. Menstruation 5. Parturition 6. Gallbladder disease 7. Urethral obstruction (Guyton) |
|
|
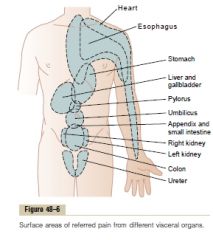
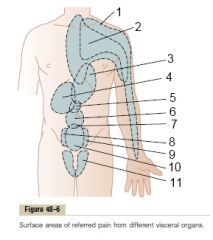
(Heart: dermatome C3-T5 since the heart originated in the neck.Side of the neck, over the shoulder, over the pectoral muscles, down the arm, and into the substernal area of the upper chest. Most frequently on the left because the left side of the heart is much more frequently involved in coronary artery disease than the right.)
(Stomach originated from T7-T9. -> Pain is referred to anterior epigastrium above the umbilicus) (Guyton) |
|
|
Mechanism of dual transmission of pain with visceral organs
|
By
1. Visceral pathways (low pain receptor density) -> sensory fibers within the autonomic nerve bundles -> referred 2. Parietal pathways -> local spinal nerves -> localized (Parietal part of peritoneum, pleura, and pericarrdium is extensively supplied by pain receptors) (Ie inflamed appendix. Referred umbilical pain by visceral pathway, lower right quadrant pain by parietal pathway by ie. adhesion of peritoneum) (Guyton) |
|
|
Hyperalgesia
a. What, primary vs. secondary b. Causes of primary and secondary hyperalgesia (one of each) |
a. Hypersensitivity to pain caused by a nervous pathway becoming excessively excitable.
Primary <- Receptor-level Secondary <- Facilitation of sensory transmission b. Causes of primary and secondary hyperalgesia Primary <- Sunburn (Sensitization of nerve endings from chemicals, histamine? prostaglandins?) Secondary <- Lesion in spinal cord or thalamus (Guyton) |
|
|
Herpes zoster\Shingles
a. Mechanism and location of pain b. Association with vesiculating rash |
a. Herpesvirus infects a dorsal root ganglion and cause pain by infectious changes of the neuronal cell in the dorsal root ganglion. Halfway dermatomal distribution
b. The virus is carried by cytoplasmic flow to the peripheral cutaneous origin. (Guyton) |
|
|
Tic Douloureux
a. What b. Characteristic of pain c. Triggered by |
a. Excruciating pain usually over one side of the face in the sensory distribution area (or part of it) of the fifth (trigeminal neuralgia) or ninth (glossopharyngeal neuralgia)
b. Like a electric shock (Can last for a few seconds at a time or be almost continuous) c. Sensitive trigger areas, mostly by mechanoreceptive stimulus (Ie in face, mouth, throat) (Can usually be blocked by cutting the perihperal nerve. Not always successful -> lesion that cause the pain might be in the sensory nucleus in the brain stem and not in the peripheral nerves) (Guyton) |
|
|
Brown-Sequard syndrome
a. What b. Effect |
a. Syndrome caused by hemitransection of the spinal cord.
b. 1. All motor functions are lost on the side of the transection in all segments below the level of the transection 2. Sensations served by spinothalamic pathway (pain, heat, cold) are lost on the opposite site of the body 3. Sensations transmitted in the dorsal and dorsolateral columns (kinesthetic and position sensation, vibration senastion, discrete localization, two-point discrimination) are lost on the same side of the transection in all dermatomes below the level of the transection 4. Light touch on the same site is lost because it cross in the medulla 5. Crude touch (poorly localized) persists because of partial transmission in the opposite spinothalamic tract (Guyton) |
|
|
Pain-sensitive areas in the cranial vault
a. Brain tissue itself? b. Pain-sensitive areas |
a. Almost totally insensitive to pain
(Electrical stimuli cause pricking type paresthesia) b. Pain-sensitive areas of the brain 1. Tugging (rykke) on the venous sinuses 2. Damaging the tentorium (dura mater fold) 3. Stretching the dura at the base of the brain 4. Blood vessels of the meninges - especially the middle meningeal artery (Guyton) |
|
|
Areas of the head to which intracranial headaches is referred
a. Stimulation of pain receptors in the cerebral vault above the tentorium, including the upper surface of the tentorium itself -> b. Pain impulses from beneath the tentorium -> |
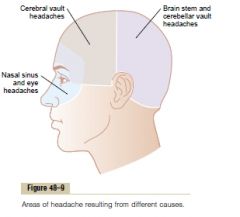
a. Initiates pain impulses in part of the cerebral portion of the fifth cranial nerve, in the ophthalmic distribution mainly.
b. Pain impulses enter the CNS through CN IX, X and second cervical nerves. -> Pain can be referred to scalp above, behind, and slightly below the ear ("Occipital headache") (Guyton) |
|
|
Types of intracranial haedaches (5)
|
1. Headache of meningitis
(Inflammation of all the meninges, including the sensitive areas of the dura and the sensitive area around the venous sinuses. -> Intense headache pain referred over the entire head) 2. Headache caused by low CSF (Removal of CSF -> removal of base of flotation of the brain -> the weight of the brain stretches and distorts the various dural surfaces -> pain) 3. Migraine headache (Theory: prolonged emotion\tension -> cerebral vasoconstriction (-> prodromal symptoms: nausea, visual disturbances, aura) -> compensatory vasodilation -> stretching of vessels -> pain) or excess local potassium in the CSF?) 4. Alcoholic headache (Alcohol probably directly irritates the meninges due to its toxicity) 5. Headache caused by constipation (Not direct link, experienced in patients with spinal cord transection, absorbed toxic products? circulatory changes?) (Guyton) |
|
|
Thermal sensations
a. Discriminated by which receptors (3) b. Location c. Mechanism of stimulation of thermal receptors |
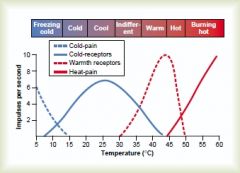
a.
1. Cold receptors (small Adelta myelinated nerve ending that branches with its tips protruding into the bottom of basal epidermal cells)(Some in type C as well) 2. Warmth receptors (Distinct receptors not confirmed histologically, free nerve endings? transmitted over type C nerve fibers) 3. Pain receptors b. The cold and warmth receptors are located immediately under the skin at discrete separated "spots" (3-10 times as many cold as warmth in most areas of the body) (The thermal receptors have partial adaptation -> changes in temperature elicit stronger sensation than steady state) c. Thermal receptors are believed to be stimulated by chemical changes in the cell during different temperatures. (Temperature alters the rate of intracellular chemical reactions more than twofold for each 10 C change.) (Guyton) |
|
|
Transmission of thermal signals in the nervous system
|
Pathway
1. Dorsal root of spinal nerve -> 2. Travel for a few segments up or down the spinal tract in the tract of Lissauer -> 3. Synapse in laminae I-III of the dorsal horn (same as for pain) -> 4. Processed by one or more interneurons -> 5. Decussate in anterior white commissure -> 6. Anterolateral tracts (anterior and lateral spinothalamic tracts) -> 7a. Reticular areas of the brain stem 7b. The ventrobasal complex of the thalamus (-> a few to somatic sensory cortex) (Somatic sensory cortex is not essential, destruction does not abolish the ability to distinguish gradations of temperature, only reduce it). (Guyton) |
|
|
Refractive index of a transparent substance
a. Velocity of light rays traveling through air b. The refractive index of a transparent substance c. Refraction |
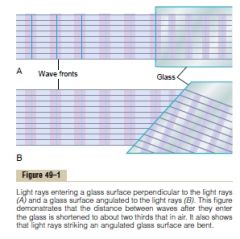
a. 300 000 km\s
b. The ratio of the velocity of light in air to the velocity in the substsance. c. Refraction I. The bending of light rays at an angulated interface. (Increase when the refractive index increase and when the degree of angulation between the two interfaces decrease.) (A perpendicular interface don't deviate it, it only cause it to change speed) (Bend because the lower portion hit the wave front before the upper portion -> The lower portion gets slowed down before the upper -> angulation of the wave) (Guyton) |
|
|
Application of refractive principles to lenses
a. Convex lens does what to light rays? b. Concave lens does what to light rays? |
a. Convex lens focuses light rays
(Progressively more toward the periphery of the lens) (Half the bending occurs when the rays enter the lens,and half as they exit from the opposite side) b. Diverge (The rays at the edge of the lens enter the lens ahead of the rays in the center. This is opposite to the effect in convex lens, and it causes the peripheral light rays to diverge from the light rays that pass through the center of the lens.) (Guyton) |
|
|
Focal length of a lens
a. What b. Change in response to divergence of the rays, as occurs when the point source is closer c. Change in response to increased curvature of the lens? |

a. The distance beyond a convex lens at which parallel rays converge to a common focal point.
b. Increased focal length. c. Decreased focal length. (Guyton) |
|
|
Measurement of the refractive power of a lens
a. Unit b. Definition of unit - applied to convex, concave, and spherical convex lenses |
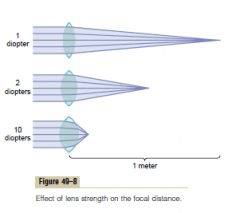
a. Diopter
b. The refractive power in diopters of a convex lens is equal to 1 meter divided by its focal length. +1: convex lens that converge parallel light rays to a focal point 1 meter beyond the lens. Concave: if a concave lens diverges light rays at the same rate that a 1-diopter convex lens converge them, it is said to have a dioptric strength of -1. (Measured by its "neutralizing" capability when set in front of a convex lens with known refractory power) Spherical convex: refractory power with angle of focus line. Horizontal is zero, vertical is 90 degrees. (Guyton) |
|
|
Refractory power of the eye
a. Total refractive power b. Its four refractive interfaces |
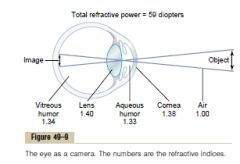
a. 59 diopters
(2\3 by the anterior surface of the cornea) (20 diopters by lens) b. 1. The interface between air and the anterior surface of the cornea 2. The interface between the posterior surface of the cornea and the aqueous humor 3. The interface between the aqueous humor and the anterior surface of the lens 4. The interface between the posterior surface of the lens and the vitreous humor (Guyton) |
|
|
Presbyopia
a. What b. Cause (2) |
a. The physiological loss of accommodation in the eyes in advancing age. (presby-: old age)
(The power of accommodation decrease from about 14 diopters in a child (can increase the refractive power from 20 to 34) to less than 2 diopters by the time the person reaches 45-50, essentially 0 at 70 years of age) b. 1. Lens grows larger and thicker 2. Becomes less elastic due to denaturation of the lens proteins (To see clearly both in the distance and nearby, an older person must wear bifocal glasses with the upper segment focused for far-seeing and the lower segment focused for near-seeing (ie. reading)) (Guyton) |
|
|
Pupillary diameter
a. Size b. Relationship of the amount of light that enters the eye and the area of the pupil c. Why does depth of focus of the lens system increase with decreasing pupillary diameter |
a. 1.5-8 mm
b. Proportional to the square of the diameter of the pupil. c. The smaller the pupillary aperture, the more centrally through the lens are the light rays that enter the lens (Guyton) |
|
|
Errors of refraction
a. Emmetropia - synonym, what b. Hyperopia - synonym, what, cause c. Myopia - synonym, what, cause d. How is the two pathologic conditions fixed with lenses |

a. Emmetropia - Normal vision
I. Emmetropic if parallel light rays from distant objects are in sharp focus on the retina when the ciliary muscles is completely relaxed. b. Hyperopia - Farsightedness I. Caused by failure of the lens system to converge or too short eyeballs II. Compensated by increased contraction of the ciliary muscle. (Lower threshold to become presbyopic, fixed by a convex lens) c. Myopia - Nearsightedness I. When the ciliary muscle is completely relaxed, the light rays coming from distant objects are focused in front of the retina. II. <- Too long eyeball or too much refractive power. (Fixed by concave (divergent) lens, no mechanism for the myopic person to compensate) (Guyton) |
|
|
Astigmatism
a. What b. Cause c. Can the body compensate? d. Treatment |
a. Astigmatism (stigma -point)
I. A refractive error of 'part' of the eye that causes the visual image in one plane to have a different focal length from that of the plane at right angles. b. Too great a curvature of the cornea in one plane of the eye. (Ie egg-shaped instead of spherical) c. No. d. Combine a spherical (to fix one plane) and cylindrical lens (to fix the other). (Guyton) |
|
|
Why is contact lenses so effective against keratoconus\conical cornea - the condition with an odd-shaped, bulging cornea?
|
The refraction of the surface of the contact lens substitutes the cornea's usual anterior refraction almost completely.
(The contact lens almost entirely nullifies the refraction that normally occurs at the anterior surface of the cornea. The tears between the contact lens and the cornea have a refractive index almost equal to that of the cornea, so that the anterior surface of the cornea no longer plays a significant role in the eye's optical system.) (Guyton) |
|
|
Visual acuity
a. Normal visual acuity for discriminating between point source b. Clinical method for stating visual acuity |
a. 25 seconds of arch (1 = 1\360 of 1 degree).
(When light rays from two separate points strike the eye with an angle of at least 25 seconds between them, they can usually be recognized as two points instead of one.) (Average diameter of a cone is about 1.5 um, two light sources can be discriminated in the fovea if they are more than 2 um apart on the retina - slightly more than the width of a foveal cone.) b. A visual acuity of 20/20 is frequently described as meaning that a person can see detail from 20 feet away the same as a person with normal eyesight would see from 20 feet. If a person has a visual acuity of 20/40, he is said to see detail from 20 feet away the same as a person with normal eyesight would see it from 40 feet away. (Guyton) |
|
|
Determination of distance of an object from the eye - depth perception. The three mechanisms
|
1. The sizes of the images of known objects on the retina.
(Comparing..) 2. The phenomenon of moving parallax (When moving the head, closer objects move more rapidly than more distant objects.) (Parallax: the apparent displacement of an object that follows a change in the position from which it is viewed) 3. The phenomenon of stereopsis - Binocular vision (The single perception of a slightly different image from each eye.) (Virtually useless for depth perception above 15-60 meters) (Stereo: spatially\three-dimensionally, opsis: vision) (Guyton) |
|
|
Ophthalmoscope
a. Principle b. Turret of lenses c. Normal corrective lens used for young adults |
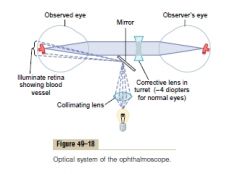
a. Bright spot on the retina (produced by light angled toward the eye by a mirror or prism) of an emmetropic eye -> return by diverging out again from the eye toward the lens system -> After passing through the lens system the light rays are parallel with one another because the retina is located one focal length distance behind the lens system -> pass into an emmetropic eye of another person -> focus again to a point focus on the retina of the second person, because his or her retina is also one focal length distance behind the lens.
b. Correct with turret of lenses if the observed or observer's eyes are not emmetropic. c. -4 diopter (In the eye of normal young adults, accommodative reflexes occur that cause an approximate +2-diopter increase in strength of the lens of each eye.) (Guyton) |
|
|
Vitreous humor
a. What b. Structure |
a. The fluid in the posterior chamber - behind the lens of the eye.
b. Gelatinous mass held together by a fine fibrillar network composed primarily of proteoglycan molecules. (Allow diffusion but little flow of fluid) (Guyton) |
|
|
Aqueous humor
a. Produced by, where, empty into b. Structure of the producing structure c. Mechanism of secretion d. Pathway of outflow |
a. Ciliary processes - folds projecting from the ciliary body. Empty into the space behind the iris where the suspensory ligaments and ciliary muscle attach to the eyeball.
(2-3 mL\min) (Their folding give them a total surface area of 6 cm2) b. Highly secretory epithelial cells. c. Active Na export -> Cl and HCO3 follow -> water follow d. Ciliary processes -> posterior chamber -> pupil -> anterior chamber -> spaces of iridocorneal angle (angle between the cornea and iris)\Spaces of Fontana (endothelium-lined spaces) -> meshwork of trabeculae -> Canal of Schlemm -> aqueous veins (filled with aqueous humor) -> extraocular veins e. Spaces of Fontana Thin-walled vein that extends circumferentially all the way around the eye. Porous endothelial membrane allowing particulate matter up to the size of red blood cells to pass from the anterior chamber into the canal of Schlemm. (Normally filled with aqueous humor, not blood) (Guyton) |
|
|
Intraocular pressure
a. Normal value b. Principle for measuring c. Mechanism for cleansing the trabecular spaces and aqueous humor - ie. after infection or hemorrhage (3) |
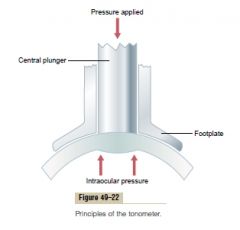
a. 15-20 mmHg
b. Measure pressure by measuring the amount of displacement of the cornea by applying pressure to it. (Locally anesthetize the cornea prior to it.) c. Mechanism for cleansing the trabecular spaces and aqueous humor 1. Large number of phagocytic cells on the surfaces of the trabecular plates of the trabecular meshwork 2. Immediately outside the canal of Schlemm is a layer of interstitial gel that contains large numbers of very active reticuloendothelial cells (High capacity for engulfing debris and digesting it into small molecular substance that can be absorbed) 3. The surface of the iris and other surfaces of the eye behind the iris are covered with an epithelium that is capable of phagocytosing proteins and small particles from the aqueous humor (Guyton) |
|
|
Glaucoma
a. What b. Pressure above ... can cause loss of vision when maintained for long periods c. Pathophysiologic mechanism of loss of vision d. Cause of acute glaucoma e. Cause of chronic glaucoma |
a. Disease of the eye in which the intraocular pressure becomes pathologically high
(Can rise to 60-70 mmHg, normal value is 15-20 mmHg) b. > 25-30 mmHg (Higher can cause blindness within days or hours) c. Increased pressure -> 1. optic nerve are compressed -> axonal cytoplasm is blocked -> loss of anterograde nutrition from the cell body to the peripheral axons -> necrosis 2. Compression of retinal artery d. White blood cells and tissue debris block trabcular spaces (normally only 2-3 um) -> acute increase e. Fibrous occlusion of the trabecular spaces (In older people) (Guyton) |
|
|
Photoreceptors
a. Name of the receptors responsible for color vision, amount b. Name of the receptors responsible for black and white vision and vision in the dark, amount |
a. Cones, 3 million
b. Rods, 100 million (Only 1.6 million ganglion cells: on average one ganglion cells receive input from 60 rods and 2 cones) |
|
|
Layers of the retina from the outside (choroid) to the inside (vitreous humor) (10)
|

Layers of the retina from the outside (choroid) to the inside (vitreous humor)
1. Pigmented layer (= Closest from choroid, light from vitreous humor must penetrate all the other layers first) 2. Outer limiting membrane 3. layer of processes of rods and cones projecting to the pigmented layer 4. Outer nuclear layer containing the cell bodies of the rods and cones 5. Outer plexiform layer - Interneuron layer - Horizontal cells 6. Inner nuclear layer - Bipolar cells 7. Inner plexiform layer - Interneuron layer - Amacrine cells 8. Ganglionic layer 9. Layer of optic nerve fibers\Stratum opticum 10. Inner limiting membrane (Guyton) |
|
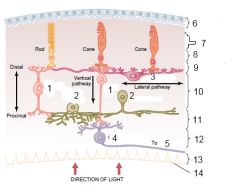
Layers and structure of the retina.
|
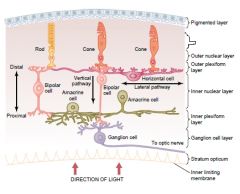
7. Layer of rods and cones projecting to the pigment
(Guyton) |
|
|
Foveal region of the retina
a. Fovea, part of which region b. Central fovea c. Properties that make the central fovea important in acute vision (2) |
a. Minute area in the center of the retina especially capable of acute and detailed vision, part of macula lutea\of retina (posterior pole of eye, 3x5 mm)
(1 mm2) b. Small area in the fovea composed almost entirely of cones (0.3 mm2) c. Properties that make the central fovea important in acute vision 1. Different shape of the cones - long and slender (1.5 um in diameter) compared to fatter cones (5-8 um) located more peripherally (Rods have a diameter of 2-5 um) 2. The structures internally covering the cones are displaced laterally (The rods and cones are external\closer to choroid than their covering structures which are internal\closer to vitreous humor) (blood vessels, ganglion cells, inner nuclear layer of cells, plexiform layers) (Guyton) |
|
|
Rods and cones
a. Major functional segments (4) b. Where is the light-sensitive chemical found? c. What is the name of the light-sensitive chemical in rods, and in cones d. Discs |
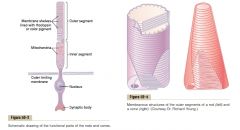
a. Major functional segments of rods and cones
1. The outer segment (Discs with photochemicals) 2. The inner segment (Usual cytoplasm, important role of mitochondria) 3. The nucleus 4. The synaptic body (Connect with horizontal and bipolar cells) b. The outer segment c. Light-sensitive chemicals I. Rods - rhodopsin II. Cones - color pigments (differences in spectral sensitivity) (Conjugated transmembrane protein, 40% of membrane of discs) d. Discs I. Infolded shelfs of cell membrane in the outer segment of rods and cones (Up to 1000\cell) (Guyton) |
|
|
Pigment layer of the retina
a. Important components (2) b. Albinos lack? ->? |
a. Pigment layer of the retina - Important components
1. Melanin (black pigment) (Prevent light reflection throughout the globe of the eyeball. Without it, light rays would be reflected in all directions within the eyeball and would cause diffuse lighting of the retina rather than the normal contrast between dark and light spots required for formation of precise images) 2. Vitamin A (Storage function - exchanged back and forth with the cell membranes of the outer segments of the rods and cones where it serves as a precursor for the photo-sensitive chemicals) b. Melanin, loss of visual acuity (20\100-20\200) (Guyton) |
|
|
Retinal detachment
a. What b. Causes (2) c. Why can the neural retina survive for some days before it is destroyed? (2) d. Symptoms (3) |
a. Detachment of the neural retina from the pigment epithelium.
b. Causes 1. Injury to the eyeball (Allow fluid or blood to collect between the neural retina and the pigment epithelium) 2. Contracture of collagenous fibrils in the vitreous humors which drags the neural retina with it c. How can the neural retina survive for some days before it necrotizes 1. Independent blood supply via the retinal artery (Normally the outer layer is mostly supplied by the choroid, especially by oxygen) 2. Diffusion across the detachment gap d. S&S 1. The sudden appearance of many floaters (small bits of debris in your field of vision that look like spots, hairs or strings and seem to float before your eyes) 2. Sudden flashes of light 3. A shadow or curtain over a portion of your visual field (Can be surgically attached) (Guyton) |
|
|
Rhodopsin-retinal visual cycle
a. Rhodopsin - components (2) b. Cycle after light energy is absorbed by rhodopsin c. What is the activated rhodopsin that excites electrical changes in the rods? d. Importance of vitamin A |

a. Rhodopsin (40% of outer segment of rods)
1. Scotopsin (The protein moiety) 2. 11-cis retinal b. Cycle after light energy is absorbed by rhodopsin 1. Rhodopsin --(light energy)--> bathordopsin 2. Bathordopsin --> lumirhodopsin (Decay reaction, bathordopsin is very unstable, ns) 3. Lumirhodopsin -> metarhodopsin I (decay) 4. Metarhodopsin I -> Metarhodopsin II (decay) 5. All-trans retinal and all-trans retinol (vitamin A) --(retinal isomerase)--> 11-cis retinal and retinol 6. 11-cis retinal automatically combines with scotopsin -> back to #1 c. Metarhodopsin II excite electrical changes in the rods d. Importance of Vitamin D I. Can replenish 11-cis retinal when it is needed or remove it when it is in excess. (Present in large amounts in the rods\cones and in the pigment layer) (Vitamin A deficiency -> night blindness, can sometimes be reversed in less than one hour by administration of vitamin A intravenously) (Guyton) |
|
|
Excitation of the rod when Rhodopsin (visual purple) is activated by light
a. How is the reduced electronegativity inside the membrane of the rod generated and maintained? b. Mechanism for action potential triggering |

a.
1. Inward leakage current of sodium into the outer segment 2. Continuous outward pumping of sodium through the inner segment (-> -40 mV resting potential) b. 1. Decomposition of rhodopsin -> decrease rod membrane conductance for sodium ions in the outer segment of the rod -> 2. Hyperpolarization (-70 to -80 mV) (Guyton) |
|
|
The eye
a. Duration of the receptor potential b. Relation of the receptor potential to light intensity |
a. Last for more than a second
(Peaks in 0.3 seconds, the change occurs four times as fast in cones) (Light ray stimulate retina for one millionth of a second -> sensation of seeing remains for longer than a second) b. Logarithmic (Guyton) |
|
|
Mechanism by which Rhodopsin decomposition decreases membrane sodium conductance - The excitation cascade
|
1. The photon activates an electron in the 11-cis retinal portion of the Rhodopsin ->-> metarhodopsin II
2. Metarhodopsin II enzymatically activate transducin (Transducin is a protein present in an inactive form in the membranes of the discs and cell membranes of rods) 3. Activates transducin activates phosphodiesterase 4. Activated phosphodiesterase remove cGMP by hydrolyzation. cGMP is bound to the sodium channel protein of the rod in a way that keeps it open. -> Allow sodium channel to close 5. Within one second, rhodopsin kinase inactivates metarhodopsin II -> reversal (30 photons can half saturate a rod due to a extremely sensitive cascade that amplifies the stimulatory effects about a millionfold)) (The cones are about 30-300 times less sensitive than the rods) (Guyton) |
|
|
Rods and cones
a. Difference of photochemicals of the cones in comparison to the rods b. Name of photochemicals of the cones (3) |
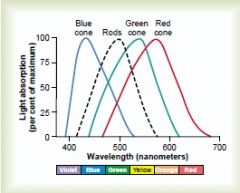
a. The protein portions - the opsins, is called photopsins in the cones and are slightly different from the scotopsin in the rods
b. Photochemicals of the cones 1. Blue-sensitive pigment (Peak absorption at light wave length of 445 nm) 2. Green-sensitive pigment (Peak absorption at light wave length of 535 nm) 3. Red-sensitive pigment (Peak absorption at light wave length of 570 nm) (Rhodopsin have a peak absorption of wave lengths of 505 nm) (Guyton) |
|
|
Mechanism of light and dark adapation (4)
|
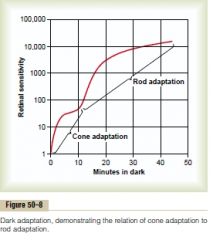
Mechanism of light and dark adaptation
1. Association\Disassociation of retinal and opsins 2. Conversion of retinal into vitamin A 3. Change in pupillary diameter 4. Neural adaptation involving the neurons in the successive stages of the visual chain (bipolar, horizontal, amacrine, ganglion cells) (Dark adaptation - sensitivity increase 10-fold the first minute, 6000-fold after 20 minutes and 25 000-fold after 40 minutes. All the chemical events, including adaptation, occur about four times as rapidly in the cones.) (Guyton) |
|
|
Red-green color blindness
a. Which colors can the person not distinguish? b. Why c. Cause |
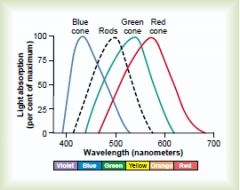
a.. Green, yellow, orange, and red (525-675)
b. These colors are normally distinguished from one another by the red and green cones. If either of these are missing, the person cannot use this mechanism for distinguishing these four colors. (The person is especially unable to distinguish red from green -> red-green color blindness) c. Lack of red cones (protanope) or green cones (deuteranope) (Lack of red cones has loss of the visual spectrum as well). (Very rare to miss blue cones, but can have genetically inherited state where they are underrepresented) (Guyton) |
|
|
Neuronal cell types of the retina (6) - which, location, transmit signal to
|

1. The photoreceptors - cones and rods
-> outer plexiform layer. Synapse with bipolar and horizontal cells. (Glutamate as neurotransmitter) 2. The horizontal cells -> horizontally in the outer plexiform layer. From the rods and cones to the bipolar cells. 3. The bipolar cells -> vertically from the rods, cones, and horizontal cells to the inner plexiform layer, where they synapse with ganglion cells and amacrine cells (Have two processes) 4. The amacrine (makros: long, -in; fiber, a cell lacking a long, fibrous process) cell Transmit signals in two directions a. Vertically: <- Bipolar cells -> ganglion cells b. Horizontally in the inner plexiform layer: bipolar cells -> ganglion cells or amacrine cells (Many subtypes of cells (> 30) secreting different inhibitory neurotransmitters: GABA, Glycine, doapmine, Ach, Indolamine) (Numerous functions as analyzing interneurons before the visual signals leave the retina. Some react to onset, offset of visual stimuli, some to movement of a spot - direction sensitive, some as part of the direct pathway of the rods..) 5. The ganglion cells <- amacrine\bipolar cell -> optic nerve 6. Interplexiform cell Transmit inhibitory signals retrograde from the inner plexiform layer to the outer plexiform layer. Believed to control lateral spread of visual signals by the horizontal cells in the outer plexiform layer (improve contrast) (Inner plexiform (weblike) layer: the layer of the retina composed of the processes of the bipolar cells, ganglion cells, and amacrine cells. Contain synaptic contacts.) (Inner nuclear layer: the layer of the retina composed of the cell bodies of bipolar cells, horizontal cells, and some of the cell bodies of the amacrine cells) (Outer plexiform layer: The layer of the retina composed of the processes of the rods and cones, horizontal cells, and bipolar cells. Contain synaptic contacts.) (Outer nuclear layer: The layer of the retina containing the cell bodies of the rods and cones) (Guyton) |
|
|
The visual pathway from the cones to the ganglion cells and from the rods to the ganglion cells
a. Direct pathway from the cones (foveal portion of retina) b. Direct pathway from the rods c. Difference between rods and cones and their central pathway (2) |

a. Cones -> bipolar cells -> ganglion cells
(Horizontal and amacrine have lateral connectivity in the outer and inner plexiform layer, respectively) b. Rods -> bipolar cells -> amacrine cells -> ganglion cells c. Cones 1. Large nerve fibers that conduct its visual signals (-> Signals are conducted to the brain 2-5 times as fast) (Guyton) |
|
|
Transmission of most signals in the retinal neurons except the ganglionic cells and partly the amacrine cells is by which mechanism? advantage?
|
Electrotonic conduction. Allows graded conduction of signal strength, not all or none as with action-potential.
(Guyton) |
|
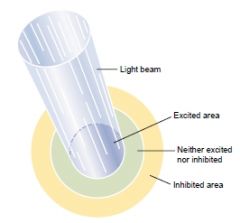
Which of the retinal neurons is responsible for this principle of excitation?
|
1. Horizontal cells in the outer plexiform layer and partly amacrine cells in the inner plexiform layer. By lateral inhibition.
2. Hyperpolarzing bipolar cells also by lateral inhibition. (Exist two cell populations of bipolar cells: hyperpolarizing and depolarizing) (Guyton) |
|
|
Differences between central retina\fovea and peripheral retina
a. Cell type and characteristics b. Ratio of photoreceptor\ganglion cells c. Sensitivity |
a. More slender rods and cones in the central retina\fovea. Only cones in the central fovea (about 35 000)
b. Almost 1\1 of photoreceptors to ganglionic cells in the central fovea (Atleast 60\1 in the peripheral retina) c. Much greater in the peripheral retina. 1. High density of rods - rods are 30-300 times as sensitive to light as cones are 2. High number of convergence of rods on ganglionic cells (up to 200) -> spatial summation (Guyton) |
|
|
Retinal ganglion cells - types and function
|
1. Type W
I. <- peripheral rods II. For directional movement and crude rod vision under dark conditions (40%, < 10 um diameter, 8 m\s, dendrites branch out extensively -> crude) 2. Type X <- rods and cones, input from at least one cone. Color vision and fine details (55%, limited branching of dendrites -> respond to discrete visual field, 10-15 um diameter of nerve fiber, 8 m\s) 3. Type Y <- broad dendritic field. Sensitive to rapid changes in visual image - movement or light intensity (< 35 um, >50m\s) (Guyton) |
|
|
Why is the contrast type of ganglionic cell not stimulated or inhibited when flat light is applied to the entire retina - that is, when all the photoreceptors are stimulated equally by the incident light.
|
Signals transmitted directly from the photoreceptors through depolarizing bipolar cells are excitatory, while the signals transmitted laterally through hyperpolarizing bipolar cells as well as through horizontal cells are mainly inhibitory.
(Need contrast - ie. differential stimulation of the photoreceptors) (Guyton) |
|
|
How does color analysis begin in the retina?
|
Some of the ganglion cells are excited by only one type of cone, but inhibited by a second type (ie excited by red, inhibited by green, or vice versa).
(Mechanism: excitatory cones goes through depolarizing bipolar cell, inhibitory cones goes through hyperpolarizing bipolar cell) (Thus, each color-contrast type of ganglion cell is excited by one color but inhibited by the "opponent" color.) (Guyton) |
|
|
Visual pathway from optic nerve
|
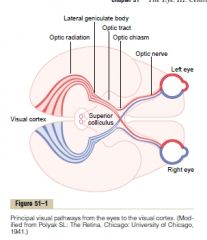
Visual pathway
1. Optic nerve -> optic chiasm: nasal halves cross and join the fibers from the opposite temporal retinas to form the optic tracts -> 2. Synapse in the lateral geniculate nucleus of the thalamus -> 3. Geniculocalcarine fibers pass by way of the optic radiation\geniculocalcarine tract -> (Lower\temporal\Meyer's loop from inferior retina, superior\parietal\Baum's loop) 4. Primary visual cortex in the calcarine fissure area of the medial occipital lobe (Brodmann area 17\Striate cortex) (Signals from macular area terminate near the occipital pole, more peripheral retina terminate in concentric half circles anterior to the occipital pole) (Based on retinal area, the fovea has several hundred times as much representation in the primary visual cortex as do the most peripheral portions) (Guyton) |
|
|
Visual pathway - alternative pathways of the optic tracts (4) and their presumed function
|
Optic tract ->
1. The suprachiasmatic nucleus of the hypothalamus I. Control circadian rhythms that synchronize various physiological changes of the body with night and day. (Functions as visual cortex in primitive animals) 2. The pretectal nuclei in the midbrain I. Reflex movements of the eyes to focus on objects of importance II. Activate the pupillary light reflex. 3. The superior colliculus I. To control rapid directional movement of the two eyes 4. The ventral lateral geniculate nucleus of the thalamus and surrounding basal regions I. Control some of the body's behavioral functions (Guyton) |
|
|
The (dorsal) lateral geniculate nucleus of the thalamus
a. <-, -> b. Nuclear layers - function c. Gating - what, controlled by d. Special about layers I, II e. Special about layers III-VI |
a. Optic tract, optic radiation\geniculocalcarine tract to primary visual cortex
b. I-VI. 1. II, III, V: receive signals from lateral half of ipsilateral retina 2. I, IV, VI: receive signals from medial half of contralateral retina c. Gating - control how much of the signals will be transmitted. Increased gating by stimuli from 1. Corticofugal fibers from the primary visual cortex 2. Reticular areas of the mesencephalon d. Magnocellular layer: receive mainly type Y retinal ganglion cells by the rapidly conducting pathway (40 m\s). (Black-and-white, poor point-to-point transmission due to few Y fibers and large dendritic branches) e. Parvocellular layers <- type W and X retinal ganglion cells. (Color, accurate point-to-point spatial information, moderate velocity: 4-8 m\s) (Guyton) |
|
|
Primary visual cortex
a. In which cortical layer does the geniculocalcarine fibers terminate? b. Functional units of the visual cortex |

a. Mainly in layer IV
(Then spread both outward toward the cortical (I-III -> signals for short distance laterally in the cortex) surface and inward toward deeper levels (V-VI -> transmit signals greater distances) b. Vertical neural columns (Several millions, 30-50 um in diameter, about 1000 cells) (Ganong) |
|
|
Visual cortex
a. Which areas are though to be the primary areas for deciphering color? b. How is the separate visual signals from the dorsal lateral geniculate nucleus processed in the primary visual cortex |

a. Color blobs
Column-like areas. Receive lateral signals (layer I-III) from adjacent visual columns (In primary and some in secondary) (Activated specifically by color signals) b. Layer IV is interlaced with stripes of neuronal columns (0.5 mm wide) where right and left eye alternatively projects into it. (This cortical area deciphers whether the respective areas of the two visual images from the two separate eyes are in register with each other. This information is used to adjust the directional gaze of the separate eyes so that their focus will fuse with each other ("brought into register") by causing interference excitation in specific neurons when their images are not "in register". Degree of nonregister provides the neural mechanism for stereopsis) (Guyton) |
|
|
Two major pathways for analysis of visual information
a. The fast position and motion pathway - recognize, which retinal ganglionic cell, pathway b. The accurate color pathway - recognize, which retinal ganglionic cell, pathway |
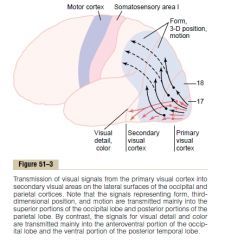
a. The fast position and motion pathway
<- 3D position, gross form, motion. By Y retinal ganglionic cell (large and fast) -> 1. posterior midtemporal area -> 2. occipitoparietal cortex (Overlap with signals from the posterior somatic association areas that analyze 3D aspects of somatosensory signals) b. The accurate color pathway <- visual detail (texture, letters, identification and meaning of object), color. By X retinal ganglionic cell -> 1. Inferior, ventral, and medial regions of the occipital and temporal cortex |
|
|
Visual cortex
a. Simple cells b. Complex cells |
a. First-order analysis, layer IV, detect lines and borders and their direction, initial details of color
b. Second-order analysis, in I-III, detect lines and their angles even though their displaced in the visual field, secondary analysis of color.. (Guyton) |
|
|
Perimetry
a. What b. Where is the blind spot? cause? c. Scotoma d. How can retinitis pigmentosa be diagnosed by perimetry? |
a. The determination of the limits (perimeters) of the visual field.
(The subject close one of the eyes, and then a small dot of light is moved back and forth in all areas of the field of vision, and the subject indicates when the spot of light can be seen and when it cannot) b. 15 degrees laterally to the central point of vision. Correspond to the optic disc on the retina where the optic nerve exits the eye and there therefore is no photoreceptors. c. Blind spots in portions of the visual field other than the optic disc area. (skotos: darkness) (<- damage to the optic nerve <- glaucoma, or from allergic reactions in the retina, or from toxic conditions such as lead poisoning or excessive smoking) d. This condition usually cause blindness in the peripheral field of vision first (Portions of the retina degenerate, and excessive melanin pigment deposits in the degenerated areas) (Retinitis pigmentosa is a progressive retinal degenerative condition, hereditary and sporadic forms) (Guyton) |
|
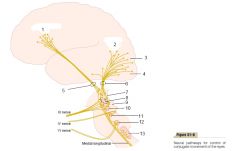
|

(Guyton)
|
|
|
Neural pathways for control of eye movements
a. Which pathway connect the brain stem nuclei of the cranial nerves responsible for extraocular movement b. Out of register left and right eyes -> ?? -> oculomotor apparatus c. Pathway for equilibrium control center's effect on the oculomotor apparatus |

a. Medial longitudinal fasciculus
b. Primary and secondary visual cortex -> occipitotectal and occipitocollicular tracts -> pretectal and superior colliculus of the brain stem -> oculomotor control to brain stem nuclei of the oculomotor nerves c. Equilibrium control center in vestibular nucleus in brain stem -> medial longitudinal fasciculus -> oculomotor system (Guyton) |
|
|
Fixation movements of the eyes - the two types and the location of responsible cortical region
|

1. The voluntary fixation mechanism.
Cortical field located bilaterally in the premotor cortical regions of the frontal lobes. 2. Involuntary fixation mechanism Secondary visual areas in the occipital cortex, mainly anterior to the primary visual cortex. (Voluntary signals must be given to unlock this visual fixation) (Guyton) |
|
|
Stereopsis
a. Functional up to b. Mechanism |
a. 60 meters
b. Some of the fiber pathways from the retinas are exactly in register (see the "same") for objects 2 meters away, some for 25, etc. Thus, the distance is determined by which set(s) of pathways are excited by nonregister or register. (Guyton) |
|
|
Strabismus\Squint (mysing)\Cross-eye
a. What |
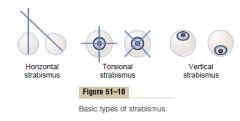
a. Lack of fusion of the eyes in one or more of the visual coordinates: horizontal, vertical, or rotational.
(Often caused by abnormal set during development in childhood of the fusion mechanism. Non-synchronized fixation, one fails to fixate) |
|
|
Control of accommodation
a. Pathway b. Mechanisms or clues that help the lens to change the strength in proper direction when finding a new focus point (4) |
a. Pathway of accommodation
1. Visual signals in Brodmann's cortical areas 18 and 19 -> 2. Pretectal area in the brain stem -> 3. Edinger-Westphal nucleus (visceral nucleus of CN III) -> 4. Parasympathetic nerves b. 1. Chromatic aberration (Red light rays focus slightly posteriorly to blue light rays because the lens bends blue rays more than red rays. The lens seems to be able to detect which of these is more in focus) 2. Convergence cause a simultaneous signal to accommodate 3. Fovea lies in a depression, maybe the lens is capable of using the differential focal length of the fovea and the rest of the retina 4. Continuous oscillation of the accommodation of the lens -> fine tune it into which part gives a higher focus (Guyton) |
|
|
Pupillary light reflex
a. Pathway b. Blocked by which pathologies (3) c. Pretectal area lesion cause which other phenomenon, how is the only way the pupil then can be stimulated to contract? d. What is an Argyll Robertson pupil? indicative of? |
a. CN II -> pretectal nuclei -> edinger-Westphal nucleus (visceromotor nucleus of CN III) -> parasympathetic nerves -> constrict sphincter of the iris
(1.5-8 mm, 30:1 change in incoming light) b. 1. CNS syphyilis 2. Alcoholism 3. Encephalitis (Usually occur at pretectal region) c. The nerves from the pretectal area to the Edinger-Westphal nucleus are mostly inhibitory. Loss of this inhibition cause the pupils to remain mostly constricted. (In addition to their failure to respond to light.) Fixation of a near object cause some degree of pupillary constriction - called the pupillary reaction to accommodation (In addition the pupils converge and accommodate) d. A pupil that 1. Fail to respond to light 2. Is in a miotic state 3. Respond to accommodation Often CNS syphilis (Guyton) |
|
|
How much higher force is exerted on the fluid of the cochlea than is exerted by the sound waves against the tympanic membrane? Which two factors are responsible for this?
|
22 times.
The lever system of the ossicles (increase the force by 1.3) and the size difference of tympanic membrane and surface of the stapes (55 mm2 vs 3.2 mm2, 17-fold difference) (Guyton) |
|
|
Impedance
a. What b. Example of use of impedance |
a. Resistance of an acoustic system to being set in motion.
b. The tympanic membrane and ossicular system provide impedance matching between the sound waves in air and the sound vibrations in the fluid of the cochlea. (Need to be higher in the cochlea due to the higher inertia of fluid) (Guyton) |
|
|
Attenuation reflex of the ossicular muscles
a. What b. Function (2) |
a. Transmission of loud sounds through the ossicular system -> CNS -(40-80 ms)-> contraction of stapedius and tensor tympani muscles to increase rigidity of the system and thus reduce ossicular conduction of low frequency sound.
(Tensor tympani muscle pulls the handle of the malleus inward while the stapedius muscle pulls the stapes outward. These two forces cause rigidity in the system by opposing each other) b. 1. Protect the cochlea from damaging vibration caused by excessively loud sound. 2. To mask low-frequency sounds in loud environments (Usually removes a major share of the background noise and allow the person to concentrate on sounds > 1000 Hz where the most pertinent information in voice communication is transmitted) (3. Also decrease a person's hearing sensitivity to his or her own speech by reflexively contracting while the person is speeking.) (Guyton) |
|
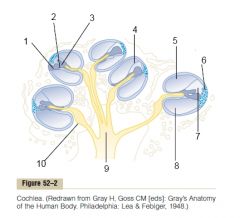
The cochlea
|
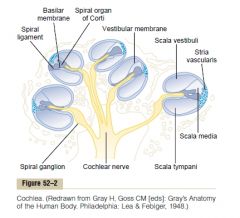
(Guyton)
|
|

The cochlea
|
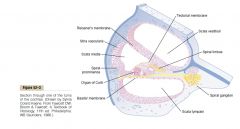
(Reissner's membrane\Vestibular membrane: separate the scala vestibuli and scala media. So thin and so easily dispalced that it does not obstruct the passage of sound vibrations from the scala vestibuli into the scala media. Therefore, as far as fluid conduction of sound is concerned, the scala vestibuli and media are considered a single chamber.)
(Basilar membrane: separates the scala media and scala tympani. On its surface lies the organ of Corti.) (Guyton) |
|
|
Basilar fibers of the basilar membrane of the cochlea
a. What is the basilar membrane b. What is the basilar fibers c. How are the basilar fibers related to sound perception |
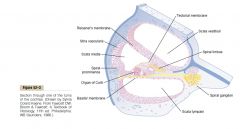
a. Fibrous membrane that separates the scala media from the scala tympani.
b. Fibers that project from the bony center of the cochlea - the modiolus, toward the outer wall. (20 000-30 000) c. They can vibrate in response to vibration of the fluid. They vary in length - progressively longer from the oval window to the tip of the cochlea (the helicotrema) (0.04 mm to 0.5 mm -> 12-fold increase), and progressively thinner. -> Differential vibration in response to different frequencies of fluid vibration. Higher frequencies vibrate the thicker and shorter fibers while lower frequencies vibrate the thicker and shorter basilar fibers. (Guyton) |
|
|
Pattern of vibration of the basilar membrane for different sound frequencies
a. Mechanism b. Location on basilar membrane of high, medium and low frequency sound |
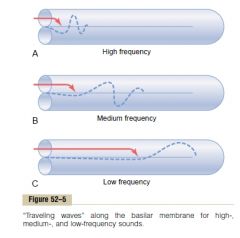
a. Each portion of the basilar membrane has a natural resonant frequency equal to the respective sound frequency. At this point, the basilar membrane can vibrate back and forth with such ease that it dissipates most of the energy of the wave so it dies out.
a. A high-frequency sound resonates the proximal part and dies out. A medium frequency travels longer before it meets its respective resonant frequency of the basilar membrane, low frequency sound travel all the way to the tip. (Also the structure of the basilar membrane allows the traveling wave to travel fast along the initial portion of the basilar membrane but become progressively slower as it goes farther into the cochlea. Due to progressively less elasticity of the basilar fibers. Allows the high-frequency sounds to not stack up on the most proximal part of the basilar membrane but spread out to allow differentiation of high frequencies.) (Guyton) |
|
|
The organ of Corti
a. Cells, location of receptor cell b. Receptor cell -> pathway |
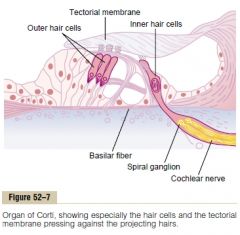
a.
1. External\Outer hair cells (12 000, 8 um in diameter) 2. Internal\Inner hair cells - receptor cells, located on the basilar fibers and membrane (3 500, 12 um in diameter, 90-95% of the nerve endings of the cochlear nerve terminate on these) b. Internal hair cell -> cochlea nerve endings -> Spiral ganglion of Corti (in modiolus of cochlea) -> cochlear nerves (30 000) -> Upper medulla (Guyton) |
|
|
Mechanism of excitation of the hair cells
|
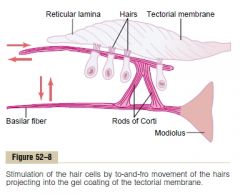
The outer portion of the hair cells is fixed to the reticular lamina, which is connected by triangular rods of Corti to the basilar fibers.
Vibration of basilar fibers spreads via triangular rods of Corti and reticular lamina to hair cells. The hair cells have stereocilia that are embedded into the tectorial membrane (a gel coating that lies above the stereocilia in the scala media). Movement of cells relative to the stereocilia in the tectorial membrane results in depolarization when bent one way and hyperpolarization when bent the other way. (The stereocilia become progressively longer on the apical side of the hair cell away from the modiolus. The shorter steroecilia are connected to the longer stereocilia by thin filaments. -> Bending of the longer stereocilia away from the smaller cause the smaller stereocilia to be tugged outward from the surface of the cell -> mechanical transduction that opens cation channels, allowing K influx (high K outside due to pumping of stria vascularis). Opposite bending of the long stereocilia cause the opposite effect. When the basilar fibers bend toward the scala vestibuli, the hair cells depolarize, and in the opposite way they hyperpolarize.) (The endolymph has intracellular ion profile (high K, low Na), +80 in comparison to perilymph - this difference is called the endocochlear potential. The endolymph is secreted by stria (stripe) vascularis. The hair cell are exposed to endolymph above the reticular fibers and perilymph below. The hair cells have a negative intracellular potential of -70 mV with respect to perilymph, but -150 mV with respect to the endolymph. It is believed that this high electrical potential at the tips of the stereocilia sensitizes the cell an extra amount - thus increasing its ability to respond to the slightest sound.) (Guyton) |
|
|
Function of outer hair cells - considering they are more than three times as numerous as the inner hair cells, yet only receive 5-10% of the nerve endings of the cochlea
|
Proposed to control the sensitivity of the inner hair cells at different sound pitches - a phenomenon called tuning of the receptor system.
(A large number of retrograde nerve fibers pass from the brain stem to the vicinity of the outer hair cells. Stimulating these can cause shortening and possibly changing of the degree of stiffness of the outer hair cells.) (Guyton) |
|
|
Place principle
a. What b. Explanation of detection of frequencies below 200 Hz |
a. Refer to the central nervous system's ability to detect different sound frequencies from the positions along the basilar membrane that are most stimulated.
b. Volley\Frequency principle: the theory that the rate of nerve impulses traveling up the auditory nerve matches the frequency of a tone. (Limited by the maximum Hz of the neuron < 500 Hz) (Volley principle is also proposed to explain identification of frequencies over the entire range by alternating firing of neurons.) (Guyton) |
|
|
Determination of loudness (3)
|
Determination of loudness
1. Louder sound -> increased amplitude of vibration of the basilr membrane and hair cells -> hair cells excite the nerve endings faster 2. Spatial summation - transmission through many nerve fibers due to activation of nearby hair cells by increased amplitude 3. The outer hair cells don't become significantly stimulated until vibration at the basilar membrane reach a high intensity. Stimulation of these cells presumably apprises the nervous system that the sound is loud (Guyton) |
|
|
Loudness
a. The power law b. decibel c. Frequency range of hearing for a young person |
a. The interpreted sensation changes approximately in proportion to the cube root of the actual sound intensity.
b. One decibel reprsent an increase in sound energy of 1.26 times (deci: 1\10, bel: a 10-fold or 1-logarithmic increase in sound energy) (The ears can barely distinguish an approximately 1 decibel change in sound intensity) c. 20-20 000 Hz (Depend on loudness though, only with intense sounds can the complete frequency range be heard.) (Usually shortened to 50-8 000 Hz in old age) (Guyton) |
|
|
Auditory nervous pathways
a. Pathway from the spiral ganglion of Corti b. In which three places does decussation occur between the ipsi- and contralateral pathway c. Collateral pathways of the auditory tract (2) |

a.
1. Spiral ganglion of Corti -> 2. Dorsal and ventral cochlear nuclei in the upper part of the medulla and synapse, 2nd order neurons -> 3. Decussate in brain stem -> superior olivary nucleus (Some don't cross) 4. Lateral lemniscus -> a. Nucleus of the lateral meniscus b. Inferior colliculus (most) -> medial geniculate nucleus of thalamus -> auditory radiation -> auditory cortex in the superior gyrus of the temporal lobe. b. 1. In the trapezoid body of the medulla 2. In the commissure between the two nuclei of the lateral lemnisci (Commissure: a bundle of nerve fibers passing from one side to the other in the brain or in the spinal cord.) 3. In the commissure connecting the two inferior colliculi c. 1. Into reticular activating system of the brain stem (-> project down to the spinal cord and upward in the brain stem to activate the entire nervous system in response to loud sound) 2. Vermis of the cerebellum (Also activated instantaneously in response to loud noise) (Guyton) |
|
|
Primary auditory cortex
a. What is the name of the organization where different frequencies in the ear correspond to different spatial points in the primary auditory cortex? b. Function of the auditory cortex |
a. Tonotopic map
(Tono: tone) (Denoting a spatial structure that subserve various frequencies, as in the auditory pathwway.) (6 different tonotopic maps in the primary auditory cortex - uncertain what the function of all is. Pitch, direction of sound, onset\offset..) b. Especially important in the discrimination of tonal and sequential patterns. (Animals with bilateral lesions can still respond to crude sounds, but cant distinguish frequencies or patterns.) (Guyton) |
|
|
Determination of the direction from which sound comes from
a. Mechanisms for determining where horizontal sound comes from (2) b. Mechanism for determining where vertical and anterior\posterior sound is coming from |
a. Mechanisms for determining where horizontal sound comes from
1. The time lag between the entry of sound into one ear and its entry into the opposite ear. (Best < 3 000 Hz, most precise) 2. The difference between the intensities of the sounds in the two ears. (Best above > 3 000 Hz) b. Accomplished mainly by the pinnae of the ear. The shape of the pinna changes the quality of the sound entering the ear, depending on the direction from which the sound comes. (Emphasize specific sound frequencies from the different directions.) (Guyton) |
|
|
Neural mechanisms for detecting sound direction
|
1. Begin in the superior olivary nuclei in the brain stem.
a. Lateral superior olivary nuclei is concerned with detecting the direction from which the sound is coming by comparing the difference in intensities of the sound reaching the two ears b. The medial superior olivary nucleus has a specific mechanism for detecting the time lag between acoustic signals entering the two ears. (This nucleus have a large number of neurons with two major projections - one to each side. The intensity of excitation of each neuron is highly sensitive to a specific time lag between the two acoustic signals from the two ears. There is a spatial pattern for detecting of different lengths of time lags. The spatial orientation of signals is the transmitted to the auditory cortex, where sound direction is determined by the locus of the maximally stimulated neurons.) 2. Auditory cortex - integrate input from the two parts of the nuclei (Guyton) |
|
|
Sense of taste - caused by (4)
|
1. Taste buds
2. Smell - interconnected 3. Texture of the food - as detected by tactual senses of the mouth 4. Presence of substances in the food that stimulate pain endings - ie. pepper (Guyton) |
|
|
Primary sensation of taste
a. Probable chemical receptors b. The five general categories - the primary sensations of taste |
a. Probable chemical receptors
1. Ionic receptors - Na, K, Cl 2. Adenosine, glutamate and inosine receptor 3. H receptor 4. Bitter, and sweet receptors (Several of some) b. The five general categories - The primary sensations of taste 1. Sour (<- acids, logarithmic relationship between sensation and concentration of H) (HCl is chosen to have 1 on the taste index for sour substances.) (Open ion channels to cause the receptor potential) 2. Salty (Ionized salts - mainly cations and thereunder mainly Na) (NaCl is chosen to have 1 on the taste index for salty taste.) (Open ion channels to cause the receptor potential) 3. Sweet (<- Many types of chemicals: sugars, glycols, alcohols, aldehydes, ketones, amides, esters, some amino acids, some small proteins, sulfonic acid, inorganic salts of lead. Most are organic chemicals.) (Sucrose is chosen to have 1 on the taste index for sweet taste) (Activate second messenger system when the taste substance binds to the receptor, to cause the receptor potential) 4. Bitter (Not caused by a single agent, most eliciting agents are organic chemicals, especially long-chain organic substances that contain nitrogen and alkaloids (quinine, caffeine, strychnine, nicotine)) (High intensity is repulsive. Protective since many toxins in the nature are alkaloids. For this purpose probably, this sense is many times more sensitive than the others.) (Quinine is chosen to have 1 on the taste index for bitter taste) (Activate second messenger system when the taste substance binds to the receptor, to cause the receptor potential) 5. Umami (Japanese for delicious) (Dominant taste of food containing L-glutamate - meat extracts, aging cheese) (Activate second messenger system when the taste substance binds to the receptor, to cause the receptor potential) (Guyton) |
|
|
Taste buds
a. Cell populations, which are the actual receptive cells b. Structure of the receptor part of the taste receptor cell c. Location of taste buds (4) d. Specificity of taste buds |
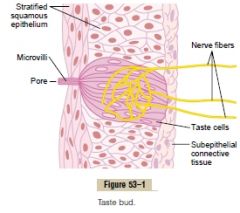
a. (50 cells\taste bud)
1. Sustentacular (supporting) cell 2. Taste cells (Continually renewed by mitosis of surrounding epithelial cells) b. Each taste cell have microvilli called taste hair that protrude through a taste pore, and it is here the actual receptor surface is. (Believed that the taste cells release a neurotransmitter to the surrounding nerve fibers) c. In 1. Walls of the troughs that surround the circumvallate papillae, which form a V line on the surface of the posterior tongue (Abundant) 2. On the fungiform papillae over the flat anterior surface of the tongue (Moderate) 3. On the foliate papillae located in the folds along the lateral surfaces of the tongue 4. On the palate, tonsillar pillars, epiglottis, and esophagus (Limited) (3 000-10 000, decrease with age) d. Usually responds mostly to one of the five taste sensation at low concentrations of the taste substance, and two or more in high conentrations. (Guyton) |
|
|
Transmission of taste signals into the central nervous system
a. Pathway from taste cells to tractus solitarius (3) b. Path further c. Path of taste reflex from the tractus solitarius |

a. Pathway from taste cells to tractus solitarius
1. Taste cells in anterior 2\3 of tongue -> lingual nerve -> chorda tympani -> facial nerve -> tractus solitarius in the brain stem 2. Taste buds on circumvallate papillae (back of tongue), other posterior regions of the mouth and throat -> glossopharyngeal nerve -> tractus solitarius (slightly more posterior) 3. Base of the tongue, other pharyngeal regions -> vagus nerve -> tractus solitarius b. Path further 1. Tractus solitarius of the brain stem --(2nd order neurons)--> 2. Ventral posterior medial nucleus of the thalamus --3rd order neurons)--> 3. Lower tip of the postcentral gyrus in the parietal cerebral cortex (where it curls deep into the sylvian fissure) and into the adjacent opercular insular area (This last area lies slightly ventral, lateral, and rostral to the area for tongue tactile signals, thus they closely parallel the somatosensory pathways of the tongue. Link between taste and texture?) c. Path of taste reflex from the tractus solitarius 1. Tractus solitarius -> superior and inferior salivatory nuclei -> submandibular, sublingual, and parotid salivary glands (Guyton) |
|
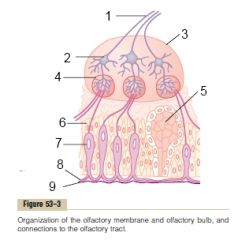
The olfactory membrane and olfactory bulb
|
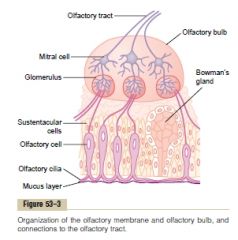
(Bowman's\Olfactory glands: branched tubuloalveolar secreting glands in the mucuous membrane of the olfactory region of the nasal cavity.)
(Olfactory glomerulus: small globular masses of dense neuropil in the olfactory bulb, containing the first synapse in the olfactory pathway.) (Neuropil: the complex, feltlike net of axonal, dendritic, and glial arborizations that form the bulk of the CNS gray matter, and in which the nerve cell bodies are located.) (Mitral cells: large nerve cells in the olfactory lobe of the brain whose dendrites synapse in glomeruli with axons of the olfactory receptor cells, and whose axons pass centrally in the olfactory tract to the olfactory cortex.) (Olfactory bulb: the grayish, expanded rostral extremity of the olfactory tract, lying on the cribriform plate of the ethmoid, and receiving the olfactory filaments.) (Olfactory nerves\CN I\fila olfactoria\Olfactory filaments: collective term for the numerous olfactory filaments: slender fascicles, each composed of the thin, unmyelinated axons of 8-12 bipolar olfactory receptor cells. They pass through the cribriform plate of the ethmoid bone and enter the olfactory bulb where they synapse with mitral, tufted, and granule cells.) (Guyton) |
|
|
The olfactory membrane
a. Cell types, which are the receptor b. Which part of the receptor reacts to odors c. Mechanism of excitation of the receptor cells |
a.
1. Sustentacular cells 2. Olfactory bipolar cells - receptors (100 million) (Olfactory membrane has a surface area of 2.4 cm2 over the superior nasal septum, roof, superior turbinate and some spreading to part of the middle turbinate) b. The olfactory hairs\cilia which project into or trough the mucosa (4-25\cell, 0.3 um in diameter, < 200 um in length) c. G-protein coupled receptors - Gs -> adenylate cyclase -> cAMP -> sodium channels (Amplifying mechanism allowing response to low concentrations) (The receptors themselves can only account for about 50% of the adaptation.) (Guyton) |
|
|
Stimulation of olfactory cells
a. Physical factors increasing substances odorigenic capability (3) |
a.
1. Volatile (So it can be sniffed into the nose) 2. Slightly water-soluble (To penetrate mucus to reach the olfactory cilia) 3. Slightly lipid-soluble (Presumably because the lipid constituents of the cilia itself are a weak barrier to non-lipid soluble odorants) (Guyton) |
|
|
Adaptation of the olfactory sense
a. Response of the olfactory receptors b. Mechanism for neural adaptation |
a. The olfactory receptors adapt 50% during the first second or so, then adapt very little.
b. Centrifugal (efferent) fibers pass from the olfactory regions of the brain to terminate on special inhibitoryr cells in the olfactory bulbs, the granule cells. These provide a means of feedback inhibition. (Guyton) |
|
|
Smell
a. Primary sensations b. Threshold c. Gradations of smell intensities - compare to auditory and visual |
a. Thought to exist over 100 primary sensations
(Evidenced by > 50 specific odor blindnesses which are thought to arise from single receptor mutations of the olfactory cells) b. Can detect 25 trillionth of a gram of methylmercaptan. c. Only 10-50 times higher than the threshold evoke maximum intensity of smell. In contrast to 500 000 times the threshold value in the case of the eyes and 1 trillion to the threshold value in the case of the ears. (Smell is more a qualitative nature of detecting the presence or absence of different gases?) (Guyton) |
|
|
Olfactory glomeruli
a. What b. Which cells synapse here c. Possible function |
a. Globular structures containing dense neuropil of the olfactory bulb and the first synapse of the olfactory pathway.
b. Olfactory bipolar cells -> mitral and tufted cells -> CNS c. Some research has indicated that different glomeruli respond to different odors - part of the analytic system? (Several thousand, 25 000 axons from olfactory bipolar cells terminate here, and 25 large mitral cells and 60 small tufted cells (the cell bodies of which lie in the glomeruli) have dendritic connections here.) |
|
|
The olfactory pathways into the central nervous system - pathway and function
a. The very old olfactory system b. The less old olfactory system c. The newer pathway |
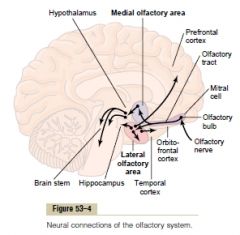
a. Olfactory tract -> the medial olfactory area (anterior to the hypothalamus)
The septal nuclei (midline) -> hypothalamus and other primitive portions of the brain's limbic system -> basic behavior (Behavior of licking the lips, salivation, and other feeding responses caused by the smell of food or by primitive emotional drives associated with smell.) b. Olfactory tract -> the lateral olfactory area: the prepyriform cortex, the pyriform (pear-shaped) cortex, and the cortical portion of the amygdala nuclei 1. -> limbic system (newer parts) (-> hippocampus: important for learning to like or dislike (aversion) certain foods) 2. -> paleocortex (older part): anteromedial portion of the temporal lobe (Only area of the entire cortex where sensory signals bypass the thalamus) c. Olfactory tract -> dorsomedial thalamic nucleus -> lateroposterior quadrant of the orbitofrontal complex Conscious perception and analysis of odor. (Guyton) |
|
|
Spinal cord
a. Types of neurons of the spinal cord (3) b. The two destinations of sensory signals into the spinal cord |
a. Types of neurons of the spinal cord
1. Sensory-relay neurons 2. Interneurons 3. Anterior motor neurons b. The two destinations of sensory signals into the spinal cord 1. Terminate immediately in the gray matter of the cord and elicit local segmental cord reflexes and other local effects. 2. Transmit signals to higher levels - spinal cord, brain stem, and cerebral cortex. (Guyton) |
|
|
Anterior motor neurons
a. Location b. Characteristics c. Types (2) |
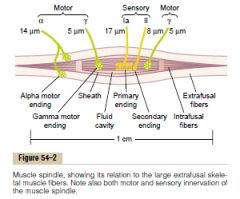
a. Anterior horns of the cord gray matter
b. 50-100% larger than most of the other neurons c. 1. Alpha motor neurons (14 um diameter nerve fiber, motor units of extrafusal skeletal muscle fibers) 2. Gamma motor neurons (Agamma nerev fibers, intrafusal muscle fibers of the muscle spindle) (Guyton) |
|
|
Interneurons of the spinal cord
a. Location b. Amount relative to anterior motor neurons c. Characteristics d. Types of neural circuits (3) |
a. In the entire gray matter of the cord.
b. 30 times as numerous as anterior motor neurons c. Small and highly excitable. Most sensory sensory signals terminate on the interneurons which feed forward to the anterior motor neurons (The corticospinal tract terminates almost entirely on spinal interneurons.) d. Diverging, converging, repetitive-discharge circuits.. (Guyton) |
|
|
Spinal cord
a. What are the mechanism responsible for lateral inhibition of skeletal muscle output b. What are the name of the fibers of the spinal cord that allow multisegmental connections from one spinal cord level to other levels |
a. Renshaw cells in the anterior horn is inhibitory and innervated by collaterals from anterior motor neurons.
b. Propriospinal fibers (Guyton) |
|
|
Muscle sensory receptors
a. Members (2) b. Which respond to what |
a. b.
1. Muscle spindles - muscle length, rate of change of length 2. Golgi tendon organ - tendon tension or rate of change of tension (Guyton) |
|
Muscle spindle
|
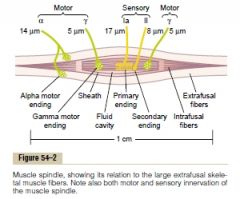
(Guyton)
|
|
|
Muscle spindle
a. Structure and location b. Motor innervation c. Sensory - in which two ways can the muscle spindle receptor be excited d. Sensory innervation |

a. Structure and location
I. In the belly of skeletal muscle II. 3-10 mm long, 3-12 intrafusal fibers. III. The intrafusal fibers have a central portion almost without contractile proteins which functions as a sensory receptor. b. Gamma motor nerve (Agamma fiber) c. In which two ways can the muscle spindle receptor be excited 1. By lengthening the whole muscle 2. By contraction of the end portions of the spindle's intrafusal fibers d. Sensory innervation 1. Primary\Annulospiral ending - Ia nerve fiber, encircles the central portion of each intrafusal fiber (17 um, 70-120 m\s) 2. Secondary ending - II nerve fiber, innervate the receptor region on one or on both sides of the primary ending (one or two, 8 um) (Guyton) |
|
|
Muscle spindle
a. Types of intrafusal muscle fibers and their characteristics (2) b. Relationship of types of intrafusal fibers and sensory innervation c. Static response - what, mediated by d. Dynamic response - what, mediated by e. Types of gamma motor nerves (2) |

a. Types of intrafusal muscle fibers and their characteristics
1. Nuclear bag fibers - several nuclei are congregated in "bags" in the central portion of the receptor area (1-3\spindle) 2. Nuclear chain fibers - nuclei aligned in a chain throughout the receptor area (3-9\spindle, 50% smaller diameter and length b. Relationship of types of intrafusal fibers and sensory innervation I. The primary sensory nerve ending (Ia, 17 um) is excited by both II. The secondary nerve ending (II, 8 um) is excited only by nuclear chain fibers. c. Static response I. The excitation of both the primary and secondary nerve endings when the receptor portion of the spindle is stretched slowly. (Almost in proportion to degree of stretch, last for minutes) d. Dynamic response I. The excitation of only the primary ending in response to rapid change of the length of the spindle receptor. (Under normal conditions there is a continuous discharge of the nerve endings. By up-regulating or down-regulating this, they can transmit increased and decreased stretch.) e. Types of gamma motor nerves 1. Gamma-dynamic I. Mainly nuclear bag intrafusal fibers II. Cause dynamic response without altering the static response 2. Gamma-static I. Mainly nuclear chain intrafusal fibers II. Enhance the static response while having little influence on the dynamic response. (Guyton) |
|
|
Muscle stretch reflex
a. What b. Pathway c. Dynamic and static stretch reflex - mediated by, function d. Combined function of both the dynamic and static stretch reflexes |
a. Sudden stretch of a muscle cause excitation of the muscle spindles which cause reflex contraction of the large skeletal muscle fibers of the stretched muscle and also of closely allied synergistic muscles.
b. 1. Ia proprioceptive nerve (primary ending) -> 2. Dorsal root of spinal cord -> 3. One branch synapse with anterior motor neurons -> 4. Contract extrafusal muscle fibers (Monosynaptic pathway) (Secondary nerve endings\Type II fibers mostly transmit via interneurons (= not monosynaptic pathway) and cause delayed signals or server other functions.) c. Dynamic is only by primary nerve endings that go via Ia nerve fibers and serve to oppose sudden changes in muscle length. (Last a fraction of a second) Static stretch reflex is mediated by both primary and secondary nerve endings (via Ia and II nerve fibers). It cause the degree of muscle contraction to remain reasonably constant. d. Provide a damping mechanism in smoothing muscle contraction. The signals from the spinal cord are often transmitted to the muscle in a jerky, low frequency form. (Synonym: signal averaging function of the muscle spindle reflex) (Guyton) |
|
|
Muscle spindle
a. Brain areas for control of the gamma motor system b. Functions (2) |
a. Bulboreticular facilitatory region of the brain stem <-
1. The cerebellum 2. The basal ganglia 3. The cerebral cortex (Also involved in control of antigravity muscles which have a high density of muscle spindles) b. 1. Dampening\Stimulus-averaging function of the muscle spindle reflex (Smooth jerky muscle contraction) 2. Stabilize body position during tense action (-> contract gamma motor neurons in antagonistic muscles over a joint -> reflex contraction on extrafusal fibers of muscles on both sides) (Guyton) |
|
|
Clonus
a. What b. Mechanism c. Cause |
a. Oscillating muscle jerks.
b. Alternation between stretching the muscle -> activating dynamic stretch reflex -> contracting -> relaxing after a fraction of a second -> stretching... c. Caused by increased facilitation of the spinal cord by decreased inhibition of the upper nervous system. (Test by suddenly stretching a muscle and applying a steady stretching force to it. If clonus occurs, the degree of facilitation is certain to be high.) (Guyton) |
|
|
Golgi tendon organ
a. Structure b. Stimulated by c. The two types of responses d. Pathways e. Function |
a. Encapsulated sensory receptor through which muscle tendon fibers pass (10-15)
b. Tension of the tendon's muscle fibers (Not muscle length and the changes of it.) c. Static and dynamic (change). d. Pathways Type Ib nerve fibers (16 um) -> 1. Local: -> inhibitory interneuron -> inhibits anterior motor neuron 2. Long: -> synapse in the dorsal horn of the cord -> several pathways, ie spinocerebellar tracts and tracts to the cerebral cortex d. Function 1. Negative feedback mechanism that prevent excessive tension on the muscle (The sudden relaxation of the muscle in response to extreme tension is called the lengthening reaction) (Protective mechanism to prevent tearing or avulsion of the muscle or the tendon) 2. Equalize contractile force among the individual muscle fibers of a muscle (Inhibit those fibers that exert excessive tension, those that exert too little tension become more excited because of absence of reflex inhibition) (Guyton) |
|
|
Flexor reflex
a. Pathway b. Involved types of circuits (3) c. Pattern of withdrawal - depend on d. Crossed extensor reflex - what, function |
a. Painful stimuli -> spinal cord interneuron pool -> motor neurons
(At least three-neuron pathway) b. 1. Diverging circuits to spread the reflex to the necessary agonistic muscles 2. Reciprocal inhibitory circuits to inhibit antagonistic muscles 3. Repetitive circuits to cause after-discharge (Lasting < 3 seconds after the stimulus is over) (After-discharge intensity depend on strength of stimulus) c. Depend on which sensory nerve is stimulated. Ie. inside of arm stimulate abductor muscles as well. (The integrative centers of the cord cause those muscles to contract that can most effectively remove the pained part of the body away from the object causing pain.) d. < 0.5 seconds after a stimulus elicits a flexor reflex in one limb, the opposite limb begins to extend. Help remove the body from a noxious stimulus by extending the other foot, thus pushing the body away. (Has a longer after-discharge period than the flexor reflex) (Flexor reflex is also caused nociceptive reflex since it is most strongly stimulated by nociceptive stimuli.) (Guyton) |
|
|
Spinal cord reflexes that cause muscle spasms
|
1. Muscle spasm resulting from a broken bone
(Results from pain impulses initiated from the broken edges of the bone, which cause the muscles that surround the area to contract tonically. Administration of a local or general anesthetic relieve the spasm.) 2. Abdominal muscle spasm in peritonitis (Also here, relief of the pain caused by the peritonitis cause the spastic muscle to relax.) 3. Some forms of muscle cramps (Local irritating factor -> reflex feedback muscle contraction -> stimulate the same sensory receptors even more -> positive feedback -> fullblown muscle cramp) (Local irritating factor can be cold, heat, hypoperfusion, overexercise) (Thus, in most instances, localized pain is the cause of the local spasm.) (Guyton) |
|
|
Autonomic reflexes in the spinal cord (5)
|
1. Changes in vascular tone resulting from changes in local skin heat.
2. Sweating, which results from localized heat on the surface of the body. 3. Intestinointestinal reflexes that control some motor functions of the gut. 4. Peritoneointestinal reflexes that inhibit gastrointestinal motility in response to peritoneal irritation. 5. Evacuation reflexes for emptying the full bladder or the colon. (Guyton) |
|
|
Mass reflex of the spinal cord
a. What b. Cause c. Effects (4) d. Analogous to what phenomenon in the brain |
a. Sudden massive discharge in large portions of the cord in a person with a transected spinal cord.
b. The usual stimulus is a strong pain sensation or excessive filling of a viscus (bladder, colon). c. 1. A large portion of the body's skeletal muscles goes into a strong flexor spasm 2. The colon and bladder are likely to evacuate 3. The arterial pressure rise to maximal pressure (>200 mmHg) 4. Large areas of the body break out into profuse sweating d. Epileptic seizures (Both are thought to be caused by activation of a great number of reverberating circuits) (The mass reflex can last for minutes) (Guyton) |
|
|
Spinal cord transection
a. Spinal shock b. Consequences c. Duration |
a. Transient depression or abolition of reflex activity below the level of an acute spinal cord injury.
(Normal activity of the cord neurons depends to a great extent on continual tonic excitation by the discharge of nerve fibers entering the cord from higher centers, particularly discharge transmitted through the reticulospinal, vestibulospinal, and corticospinal tracts.) b. 1. Severe hypotension (as low as 40 mmHg) 2. Loss of skeletal muscle reflexes integrated in the spinal cord (some reflexes may eventually become hyperexcitable, especially if some facilitatory pathways remains intact while the remainder of the spinal cord is transected. The first reflex to return are the stretch reflexes, followed by the more complex flexor reflexes, postural antigravity reflexes, and remnants of stepping reflexes.) 3. The sacral reflexes for control of bladder and colon evacuation are suppressed c. Depend on the components - from hours (vasomotor) to several months (some skeletal muscle reflexes). Some may not be regained. (The neurons regain their excitability gradually. This seems to be a general principle - after neurons lose their source of facilitatory impulses, they increase their own natural degree of excitability to make up at least partially for the loss.) (Guyton) |
|
|
How are most "voluntary" mechanisms initiated by the cebrebral cortex achieved?
|
Most are achieved by the cerebral cortex activating patterns of function stored in lower brain areas, these include the cord, the brain stem, basal ganglia, and cerebellum.
(Guyton) |
|
|
The three subareas of the motor cortex
|
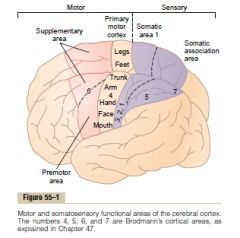
1. The primary motor cortex
2. The premotor area 3. the supplementary motor area (Guyton) |
|
|
A single motor cortex neuron usually excites ..?
|
A specific movement by exciting a "pattern" of separate muscles.
(Rather than exciting a specific muscle.) (Guyton) |
|
|
Premotor area
a. What does nerve signals generated in the premotor area cause |
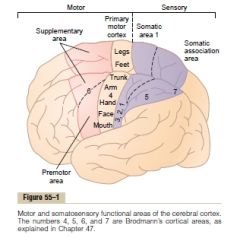
a. Patterns of movement of separate muscles, but more complex than in the primary motor cortex.
(The most anterior part of the premotor area first develops a "motor image" of the total muscle movement that is to be performed. Then the posterior premotor cortex use this image to excite each successive pattern of muscle activity required to achieve this motor image. It sends its signals either directly to the primary motor cortex or via the basal ganglia and thalamus to the primary motor cortex.) (Guyton) |
|
|
Specialized areas of motor control found in the human motor cortex - location and function
a. Broca's area b. Voluntary eye movement field c. Head rotation area d. Area for hand skills |
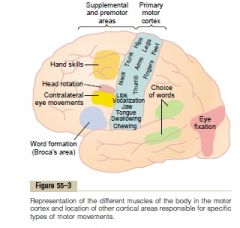
a. Broca's area
Immediately anterior to the primary motor cortex and immediately above the sylvian fissure. Needed for a person to speak whole words - the coordinated muscular part of speaking. (Lesion leaves the patient only able to utter simple words as no, yes. Lie in close proximity to a cortical area that synchronize respiration with speech.) b. Voluntary eye movement field Immediately above Broca's area. Also control blinking. (Lesion -> the eyes tend to lock involuntarily onto specific objects) c. Head rotation area Above the voluntary eye movement field. Direct the head toward different objects, and is closely related to the eye movement field. d. Area for hand skills\Exner's area In the premotor area immediately anterior to the primary motor cortex. (Lesion -> uncoordinated and nonpurposeful hand movements - motor apraxia) (Apraxia (pratto: to do): loss or impairment in performing complex coordinated movements without sensory or muscular impairment.) (Guyton) |
|
|
Corticospinal\Pyramidal tract
a. Origin (3) b. Pathway c. What happens to the fibers that don't cross over in the medulla? |

a.
1. The primary motor cortex (30%) 2. the premotor and supplementary motor cortex (30%) 3. The somatosensory areas (3) b. 1. Cortex -> 2. Posterior limb of internal capsule -> (Between the caudate nucleus and the putamen of the basal ganglia) 3. Downward through the brainstem as the pyramids of the medulla -> 4. (Most) decussate in the lower medulla -> 5. Descend into the lateral corticospinal tracts of the cord -> 6. -> interneurons in the intermediate regions of the cord gray matter (A few terminate on sensory relay neurons and a few directly on anterior motor neurons) c. Pass ipsilaterally down the cord in the ventral corticospinal tracts Most cross in the neck or upper thoracic region. (May be concerned with the control of bilateral postural movements by the supplemental motor cortex) (Guyton) |
|
|
Other pathways beside the corticospinal tract from the motor cortex (6)
|
1. Collaterals from Betz cells back to the cortex itself - lateral inhibition.
2. -> Caudate nucleus and putamen (-> brain stem and spinal cord. Mainly to control body postural muscle contractions.) 3. -> Red nuclei of the midbrain -> rubrospinal tract 4. -> Reticular substance and vestibular nuclei of the brain stem -> a. Reticulospinal and vestibulospinal tracts b. Reticulocerebellar and vestibulocerebellar tracts 5. -> Pontile nuclei -> pontocerebellar fibers 6. -(collaterals)-> Inferior olivary nuclei -> olivocerebellar fibers (Guyton) |
|
|
Incoming fiber pathways to the motor cortex (5)
|
1. Subcortical fibers from adjacent regions of the cerebral cortex
a. Somatosensory areas of the parietal cortex b. The adjacent areas of the frontal cortex anterior to the motor cortex c. The visual and auditory cortices 2. Subcortical fibers that arrive through the corpus callosum from the corresponding opposite cerebral hemisphere 3. Somatosensory fibers that arrive directly from the ventrobasal complex of the thalamus (Mainly cutaneous tactile signals and joint and muscle signals) 4. Cerebellum and basal ganglia -> ventrolateral and ventroanterior nuclei of the thalamus -> motor cortex (Coordination among the motor control functions of the motor cortex, basal ganglia, and cerebellum.) 5. From the intralaminar nuclei of the thalamus (Control the general level of excitability of the motor cortex, in the same what they control it in the rest of the cerebral cortex.) (Guyton) |
|
|
Red nucleus in the mesencephalon
a. Function b. Pathway c. Collective name with the corticospinal tract |
a. Alternative crude pathway for transmitting cortical signals to the spinal cord.
(Can not perform delicate movements - such as finger movements.) b. <- direct fibers from the motor cortex as the corticorubral tract and collaterals from the corticospinal tract -> magnocellular lower portion of red nucleus -> rubrospinal tract -> decussate in the lower brain stem -> follow the corticospinal tract and lie anterior to it (The magnocellular portion contains neurons related to Betz cells which is large and have a crude somatographic map) (Also have close connections to the cerebellum) c. Lateral motor system (Lie in the lateral columns along with the corticospinal tract) (Medial motor system: vestibuloreticulospinal system) (Guyton) |
|
|
Red nucleus in the mesencephalon
a. Function b. Pathway c. Collective name with the corticospinal tract |
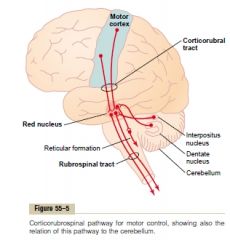
a. Alternative crude pathway for transmitting cortical signals to the spinal cord.
(Can not perform delicate movements - such as finger movements.) c. Lateral motor system (Lie in the lateral columns along with the corticospinal tract) (Medial motor system: vestibuloreticulospinal system) (Guyton) b. <- direct fibers from the motor cortex as the corticorubral tract and collaterals from the corticospinal tract -> magnocellular lower portion of red nucleus -> rubrospinal tract -> decussate in the lower brain stem -> follow the corticospinal tract and lie anterior to it (The magnocellular portion contains neurons related to Betz cells which is large and have a crude somatographic map) (Also have close connections to the cerebellum) |
|
|
Motor cortex
a. Functional units b. Which layer is the pyramidal cells in c. Which layers does the input signal enter into d. What does the sixth layer give rise to? e. Functions of individual columns |
a. Vertical six-layer columns
(Usually stimulate a group of synergistic muscles.) b. Fifth layer c. Second-fourth d. Give rise to fibers that communicate with other regions of the cerebral cortex itself. e. Functions of individual columns 1. Integrate input and cause an output response 2. Can function as an amplifying system to stimulate large numbers of pyramidal fibers for the same synergistic muscle group (This is important because 50-100 pyramidal cells need to be excited simultaneously or in rapid succession to achieve muscle contraction) (Guyton) |
|
|
Motor cortex - static and dynamic signals
a. Difference b. Location of generation of the two signals |
a. A much weaker continuing signal can maintain a contraction than that needed to initiate it. The dynamic neurons initiate movement by being excessively excited for a short period at the beginning of a contraction (Causing the initial rapid development of a force). The static neurons fire at a slower rate to maintain the force of contraction.
b. Both the parvocellular nuclei of the red nucleus and the Betz cells of the motor cortex have both static and dynamic neurons. However, there is a greater percentage of dynamic neurons in the red nucleus and a greater percentage of static neurons in the motor cortex. (The red nucleus is closely related with the cerebellum, and the cerebellum is important in rapid initiation of muscle contraction.) (Guyton) |
|
|
Spinal cord motor reflexes (8)
|
1. Stretch reflex
2. Withdrawal reflex 3. Crossed extensor reflex (stimuli -> flexor of same limb -(delay)-> extension of contralateral limb) 4. Stepping 5. Walking (Reciprocal inhibition by extensors and flexors of the foot) 6. Scratching (itch\tickle -> position sense -> to-and-fro scratching (reciprocal inhibition)) 7. Postural mechanisms (positive support reaction: pressure on foot -> limb extension, stronger where the pressure is stronger -> magnet reaction (prevent collapse\falling)) 8. Stumble reflex (Obstruction during walking -> stop -> lift foot -> continue) |
|
|
Area pyramidalis of the primary motor cortex
a. Function b. Which movements are lost when the area pyramidalis is lesioned? |
a. Essential for voluntary initiation of finely controlled movements, especially of the hands and fingers.
b. All except gross postural and limb fixation movements (Guyton) |
|
|
Lesions that damage large areas adjacent to the motor cortex
a. What is the effect of damaging the small neurons of the primary motor cortex b. What is the mechanism for development of muscle spasms after lesions of the motor cortex |
a. These normally maintain a continual tonic stimulatory effect on the motor neurons. Loss of this results in hypotonia.
b. A stroke usually affect adjacent parts of the brain such as the basal ganglia. The spasm results mainly from damage to accessory pathways from the nonpyramidal portions of the motor cortex. these pathways normally inhibit the vestibuloreticulosystem. Loss of this inhibition cause this system to become spontaneously active and cause excessive spastic tone in the involved muscles. (Guyton) |
|
|
Brain stem
a. Components b. Why can it functionally be considered an extended spinal cord c. Special control functions (6) |
a. Mesencephalon, pons, medulla.
b. It contains motor and sensory nuclei that perform motor and sensory functions for the face and head region in the same manner that the spinal cord performs these functions from the neck down. b. 1. Control of respiration 2. Control of the cardiovascular system 3. Partial control of the gastrointestinal system 4. Control of many stereotyped movements of the body 5. Control of equilibrium 6. Control of eye movements (Guyton) |
|
|
Cerebral cortex
a. Thickness b. Number of neurons c. Surface area |
a. 2-5 mm
b. 100 billion neurons c. 1\4 m2 (Guyton) |
|
|
Cerebral cortex
a. Granular\Stellate neurons - structural characteristics, functional characteristics, where is the highest concentration of them b. Pyramidal and fusiform cells - structural and functional characteristics, location |
a. Granular\Stellate neurons
Short axons -> short distance transmission. Functions mainly as interneurons. Both the sensory, association, and motor areas have large concentrations of them. (Inhibitory release mainly GABA, excitatory release mainyl glutamate) b. Pyramidal and fusiform cells Give rise to most of the output of the cerebral cortex. The pyramidal cells are larger and more numerous, and are the neurons that give rise to the long nerve fibers that go all the way to the spinal cord. (Guyton) |
|
|
Cerebral cortex
a. Function of layers I-III b. Function of layer IV c. Function of layer V and VI |
a. Perform most of the intracortical association functions.
b. Receive most of the incoming specific sensory signals. c. Most of the output signals leave the cortex through neurons located in these layers. (V: the large fibers to the brain stem and spinal cord arise from here) (VI: to thalamus) (Guyton) |
|
|
Thalamocortical system - what? why?
|
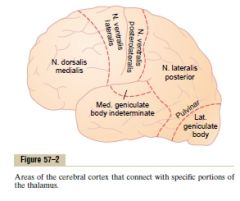
The thalamus and cortex. Can be considered a structural and functional unit. Structural because there is extensive afferent and efferent interconnections. Functional because when the connection to the thalamus is lost, the functions of the corresponding cortical area become almost entirely lost.
(Except some olfactory pathways, all sensory pathways goes first through the thalamus.) (Guyton) |
|
|
What are the name of the neurosurgeons who did the most famous cortical function mapping?
|
Penfield and Rasmussen.
(By electrical stimuli during neurosurgery and by examining patients with specific structural lesions.) (Guyton) |
|
|
Association areas
a. The three most important b. Function |
a.
1. Prefrontal association area 2. The parietoccipitotemporal association area 3. The limbic association area b. They receive and analyze signals simultaneously from multiple regions of both the motor and sensory cortices as well as from subcortical structures. (Guyton) |
|
|
Parieto-occipitotemporal association area
a. Location b. The functional subareas (4) |

a. Between the somatosensory cortex anteriorly, the visual cortex posteriorly, and the auditory cortex laterally.
b. 1. Analysis of the spatial coordinates of the body (Computes the coordinates of the visual, auditory, and body surroundings) (posterior parietal cortex->superior occipital cortex) 2. Area for language comprehension\Wernicke's area (behind the primary auditory cortex in the posterior part of the superior gyrus of the temporal lobe.) (The most important region of the brain for higher intellectual functioning, because almost all such intellectual functions are language based) 3. Area for initial processing of visual language (reading) (Angular gyrus area) (Posterior to the language comprehension area, in the anterolateral region of the occipital lobe.) (Feed to Wernicke's area) 4. Area for naming objects (Most lateral portions of the anterior occipital lobe and posterior temporal lobe) (Guyton) |
|
|
Prefrontal association cortex
a. Input b. Function c. Special functional area |

a. Much from subcortical bundles of fibers connecting the parieto-occipitotemporal association area with the prefrontal area.
(<- preanalyzed informaton, important information on the spatial coordinates of the body that is necessary for planning effective movements.) b. Plan motor movements and carry out thought processes. (Much of the motor output passes through the caudate portion of the basal ganglia-thalamic feedback circuit for motor planning.) c. Broca's area (Provide the neural circuitry for word formation, located partly in the prefrontal association cortex and partly in the premotor area. Plans and motor patterns for expressing words and phrases are initiated and executed here) (Guyton) |
|
|
Limbic association area
a. Location b. Functions\Associated with |

a. Found in the
1. Anterior pole of the temporal lobe 2. In the ventral portion of the frontal lobe 3. In the cingulate gyrus (Deep in the longitudinal fissure on the midsurface of each cerebral hemisphere) b. 1. Behavior 2. Emotion 3. Motivation (Part of a larger limbic system which include a complex set of neuronal structures in the midbasal regions of the brain.) (Guyton) |
|
|
Prosophenosia
a. What b. Cause |

a. Inability to recognize faces. (Prosopo: face)
(Prosopagnosia - Difficulty in recognizing familiar faces) b. Bilateral damage to the underside of the occipital lobes and medioventral surface of the temporal lobes (Occiptal part is concerned with visual input, the temporal part is closely associated with the limbic system and therefore emotion, behavior and motivation.) (Guyton) |
|
|
Wernicke's area
a. Location b. Synonyms c. Function d. Lesion -> in association with language e. Electrical stimulation of this area in a conscious person often cause |
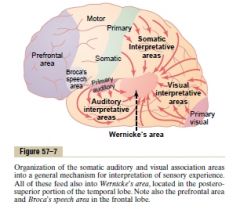
a. Posterior part of the temporal lobe, confluence of the different sensory interpretative areas (somatic, auditory, visual)
(Usually best developed on the left side) b. The general interpretative area\the gnostic (knowledge)\The tertiary association area c. The most important single structure for the higher comprehension levels of brain function (intelligence) d. Unable to arrange words - spoken or written, into a coherent thought e. A highly complex thought (Visual scene, specific musical piece..) (Therefore it is believed that activation of Wernicke's area can call forth complicated memory patterns that involve more than one sensory modality even thought most of the individual memories may be stored elsewhere.) (Guyton) |
|
|
Concept of the dominant hemisphere
a. In how many percent of people is it on the left side b. Involved areas or functions c. Proposed theory |
a. 95%
b. 1. Interpretative functions of the Wernicke's area and angular gyrus 2. Functions of the speech and motor control areas (90% are right-handed - controlled by left hemisphere). c. The attention of the mind seems to be limited to one principal thought at the time. In >50% of neonates the left Wernicke's area is 50% larger than the right. Because of the tendency to direct one's attention to the better developed region, the rate of learning in the cerebral hemisphere that gains the first start increases rapidly, whereas in the opposite, less-used side, learning remains slight. (Guyton) |
|
|
Functions of the parieto-occipitotemporal cortex in the nondominant hemisphere (4)
|
1. Understanding and interpreting music
2. Nonverbal visual experiences 3. spatial relations 4. Capability to comprehend and interpret body language and intonation (Guyton) |
|
|
Neural pathway for communication from written word to speech
|
1. Primary visual area ->
2. Angular gyrus - early interpretation -> 3. Wernicke's area - interpretation of the words -> 4. Wernicke's area - determination of thoughts and the words to be spoken -> 5. Arcuate fasciculus - Transmission of signals from Wernicke's area to Broca's area 6. Broca's area - activation of the skilled motor programs for control of word formation -> 7. -> motor cortex -> control speech muscles (Guyton) |
|
|
The corpus callosum provide abundant bidirectional neural connections between most of the respective cortical areas of the two cerebral hemispheres except for ..., which are connected by ...
|
The anterior portions of the temporal lobes, especially the amygdala
Anterior commissure (Guyton) |
|
|
The holistic theory of thoughts
|
A thought results from a "pattern" of stimulation of many parts of the nervous system at the same time, probably involving most importantly the cerebral cortex, thalamus, limbic system, and upper reticular formation of the brain stem.
(The stimulated areas of the limbic system, thalamus, and reticular formation are believed to determine the general nature of the thought, giving it such qualities as pleasure, displeasure, pain, comfort, localization to gross areas of the body..) (Specific stimulated areas of the cerebral cortex determine discrete characteristics of the thought: localization on the body, texture, visual recognition) (Guyton) |
|
|
Consciousness
|
Our continuing stream of awareness of either our surroundings or our sequential thoughts.
(Guyton) |
|
|
Memory
a. Physiologically, memories are stored in the brain by changing ..., as a result of ... b. The new or facilitated pathways are called ... |
a. the sensitivity of synaptic transmission between neurons as a result of previous neural activity
b. Memory traces (Guyton) |
|
|
Memory
a. Negative memory - what, mechanism, name of phenomenon b. Positive memory, what, mechanism, name of phenomenon |
a. The capability of the brain to ignore information that is of no consequence. Achieved by inhibition of the synaptic pathways. This effect or phenomenon is called habituation.
b. Incoming information that are judged by specific areas in the basal limbic regions as being important are stored by facilitation. The phenomenon is called memory sensitization. (Guyton) |
|
|
Classification of memories, duration and characteristics of
a. Short-term memory b. Intermediate-term memory c. Long-term memory |
a. Short-term memory
I. Memories that last for seconds or at most minutes (Working memory: short-term memory that is used during the course of intellectual reasoning.) II. Capable of handling 7-10 entities (Continual neural activity? aspects of reverberating circuit? presynaptic facilitation\inhibition?) b. Intermediate-term memories Memories that last for days to weeks, but then fades away Structural or chemical transient changes c. Long-term memories Structural changes (Guyton) |
|
|
Theory of memory based on Kandel's research on the Aplysia snail
a. Mechanism for habituation b. Mechanism for facilitation |
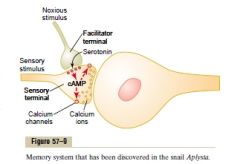
a. Mechanism for habituation
I. Decreased conductance of Ca channels in the sensory terminal, caused by sensory terminal activity without simultaneous activity of the facilitator terminal. (Type of negative memory that causes the neuronal circuit to lose its response to repeated events that are insignificant) b. Mechanism for facilitation 1. Stimulation of the facilitatory terminal by noxious (important) stimuli at the same time that the sensory terminal is stimulated causes serotonin release at the facilitator synapse 2. Serotonin -> Serotonin receptors in the sensory terminal membrane -> activate adenyl cyclase -> cAMP -> 3. cAMP -> protein kinase -> phosphorylate part of a K channel -> block K channel (can last for weeks) -> 4. Prolonged action potential -> prolonged activation of Ca channels -> more Ca enter sensory synaptic terminal -> more neurotransmitter is released -> facilitate synaptic transmission (Guyton) |
|
|
Long-term memory - proposed mechanism
|
Physical restructuring of the synapses themselves in a way that changes their sensitivity for transmitting nervous signals.
The changes include 1. Increase in vesicle release sites for secretion of transmitter substances 2. Increase in number of transmitter vesicles released 3. Increase in number of presynaptic terminals 4. Chagnes in structures of the dendritic spines that permit transmission of stronger signals (The structural changes will not occur if a drug is given that blocks DNA stimulation of protein replication in the presynaptic neuron, nor will the permanent memory trace develop. (Guyton) |
|
|
Consolidation
a. What b. Mechanism |
a. The process of turning a short-term memory into a intermediate- or long-term memory.
b. Mechanism I. The short-term memory, if activated repeatedly, will initiate chemical, physical and anatomical processes in the synapses that are responsible for the long-term type of memory. (Require 5-10 minutes for minimal consolidation, 1 hour for strong consolidation. Proved by inducing convulsion or anesthesia after exposure to event.) (Guyton) |
|
|
Anterograde amnesia
a. What b. Caused by lesion of which structure of the nervous system c. Why |
a. Inability to store declarative memory from short-term to more lasting forms.
b. Hippocampus (Part of limbic system, the most medial portion of the temporal lobe cortex) c. The hippocampi are among the most important output pathways from the reward and punishment areas of the limbic system that is critically involved in making the decision about which of our thoughts are important enough on a basis of reward (what can they gain us) or punishment (avoid aversion) to be worthy of memory. (Guyton) |
|
|
Activating-driving systems of the brain - how does the brain stem activate the cerebral part of the brain (2)
|
1. By directly stimulating a background level of neuronal activity in wide areas of the brain.
2. By activating neurohormonal systems that release specific facilitory or inhibitory hormone-like neurotransmitter substances into selected areas of the brain. (Guyton) |
|
|
The bulboreticular facilitatory region\The reticular substance of the pons and mesencephalon
a. Function b. Stimulated by c. Location |
1. Transmit facilitory signals downward to the spinal cord to maintain tone in the antigravity muscles and to control levels of activity of the spinal cord reflexes.
2. Sends excitatory signals in the upward direction -> thalamus, excite a different set of neurons that transmit nerve signals to all regions of the cerebral cortex as well as some subcortical areas b. Stimulated by 1. Peripheral sensory signals I. Depends on number and type II. Pain is especially excitatory (Demonstrated by cutting the brain stem above the point where CN enter the brain stem, this is the most superior somatosensory input. This results in coma. Transecting below CN V entrance don't.) 2. Feedback signals returning from the cerebral cortex (Brain thought processes, motor processes. Positive feedback mechanism that allows any beginning activity in the cerebral cortex to support still more activity, thus leading to an "awake" mind) c. Posterior and laterally in the pons and mesencephalon of the brain stem. (Guyton) |
|
|
Bulboreticular facilitory area\The reticular substance of the pons and mesencephalon
a. Stimulated by (2) b. Location |
a.
1. Peripheral sensory signals Number and type, pain is especially excitatory (demonstrated by cutting the brain stem above the point where CN enter the brain stem, this is the most superior somatosensory input. This results in coma. Transecting below CN V entrance don't.) 2. Feedback signals returning from the cerebral cortex (Brain thought processes, motor processes, positive feedback mechanism that allows any beginning activity in the cerebral cortex to support still more activity, thus leading to an "awake" mind) b. Posterior and laterally in the pons and mesencephalon of the brain stem. (Guyton) |
|
|
The reticular inhibitory area
a. Location b. Function |
a. Location
I. Medial and ventral in the medulla. b. Function I. Can inhibit the reticular facilitatory area and thereby decrease activity in the superior portions of the brain. (By serotonergic fibers, serotonin is inhibitory) (Guyton) |
|
|
Neurohormonal control of brain activity, <-, ->, characteristics
a. The norepinephrine system b. The dopamine system c. The Serotonin system d. The acetylcholine system |

a. The norepinephrine system
<- The locus ceruleus (blue), small area located bilaterally and posteriorly at the juncture between the pons and the mesencephalon. -> spread throughout the brain NE has mostly excitatory effec (probably involved in causing dreaming by leading to REM sleep) b. The dopamine system <- The substantia nigra, lies anteriorly in the superior mesencephalon -> caudate nucleus and putamen of the cerebrum (basal ganglia nuclei) Inhibitory at basal nuclei ganglia, possibly excitatory in other areas (Some areas next to substantia nigra are dopaminergic and project to more ventral areas of the brain) c. The serotonin system <- the raphe nuclei, several nuclei in the midline of the pons and medulla -> diencephalon, cerebral cortex, spinal cord (can suppress pain) Inhibitory (Help cause normal sleep by stimulating diencephalon and the cerebrum.) d. The acetylcholine system <- The gigantocellular neurons of the reticular excitatory area, in the pons and mesencephalon -> 2 branches 1. Reticulospinal 2. Upward Excitatory in most places (The following is a list of other neurohormonal substances that functon either at specific synapses or by release into the fluids of the brain: 1. Enkephalins 2. GABA 3. Glutamate 4. Vasopressin 5. ACTH 6. Epinephrine 7. Histamine 8. Endorphins 9. ATII 10. Neurotensin) (Guyton) |
|
|
Support of the body against gravity
a. Role of the pontine reticular system b. Role of the Medullary reticular system c. The pontine reticular system function in close association with ... to excite the antigravity muscles |
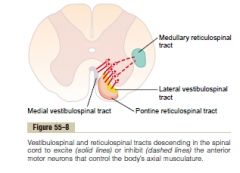
a. Excite the antigravity muscles (the muscles of the vertebral column, trunk, and the extensor muscles of the limbs)
(Pontine reticular nuclei -> the pontine reticulospinal tract (anterior column) -> medial anterior motor neurons -> axial muscles (antigravity muscles) (<- excitatory signals from the vestibular nuclei and from deep nuclei of the cerebellum) b. Transmit inhibitory signals to the same antigravity anterior motor neurons (medullary reticular nuclei -> medullary reticulospinal tract (lateral column) -> medial anterior motor neurons -> antigravity muscles) (Receive inhibitory input from collaterals from the corticospinal tract, the rubrospinal tract, and other motor pathawys.) (Prevent excessive tension in the antigravity muscles and can relax certain portions of the body to allow them to perform specific motor activities.) c. All the vestibule nuclei. (Transmit strong excitatory signals to the antigravity muscles by way of the lateral and medial vestibulospinal tracts in the anterior columns) (Specifically, this system is involved in activating specific portions in accordance with signals from the equilibrium organ of the vestibule) (Guyton) |
|
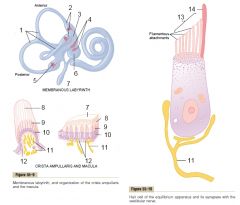
The vestibular apparatus
|
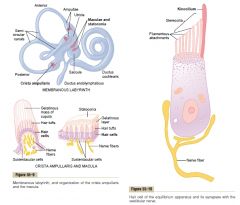
(Macula (spot): the neuroepithelial sensory receptors of the utricle and saccule)
(Statoconia (statos: standing, konis: dust)\Otoliths (ear, stone): crystalline particles of calcium carbonate and protein adhering to the gelatinous membrane of the maculae of the utricle and saccule.) (Ampullary crest: an elevation on the inner surface of the ampulla of each semicircular duct, filaments of the vestibular nerve pass through the crista to reach hair cells on its surface) (Ductus endolymphaticus: connect the utricle and saccule, -> aqueduct of vestibule -> endolymphatic sac (cul de sac)) (Cupula ampullaris: a gelatinous mass that overlies the hair cells of the ampullary crest of the semicircular ducts, movements of the endolympathic fluid cause the cupula to move across the hair cells of the ampullary crest) (Hair cells: sensory epithelial cells present in the organ of Corti, in the maculae and cristae of the membranous labyrinth of the ear, and in taste buds, characterized by having long stereocilia, kinocilia, or both) (Stereocilia: a nonmotile long microvillus) (Kinocilia: a cilium, usually motile, having nine peripheral double microtubules and two single central ones, only found on hair cells in the cochlea and maculae of the saccule and utricle and cristae of the semicircular canals) (Cilium: a motile extension of a cell surface, ie. epithelial cell, contain nine peripheral doubles of microtubules and a central pair) (Guyton) |
|
|
Hair cells
a. What b. Found where (3) c. Characterized by d. Kinocilia, Stereocilia e. Where is the only three places where kinocilia is found |
a. Sensory epithelial cells
b. Location 1. The organ of Corti 2. In the maculae and cristae of the membranous labyrinth of the ear, 3. In taste buds c. characterized by having long stereocilia, kinocilia, or both d. Stereocilia: a nonmotile long microvillus Kinocilia: a cilium, usually motile, having nine peripheral double microtubules and two single central ones e. The kinocilia are only found on hair cells in the cochlea and maculae of the saccule and utricle and cristae of the semicircular canals. (Cilium: a motile extension of a cell surface, ie. epithelial cell, contain nine peripheral doubles of microtubules and a central pair) (Guyton) |
|
|
Vestibular apparatus
a. What is the name of the sensory organ of the utricle and saccule? b. What do they detect - important when |
a. Maculae
(2 mm2) b. 1. Static role The macula of the utricle lies mainly in a horizontal plane and plays an important role in determining orientation of the head when the head is upright. The macula of the saccule is located mainly in a vertical plane and signals head orientation when the person is lying down. 2. Dynamic role - linear acceleration (Guyton) |
|
|
Vestibular apparatus
a. Components of the maculae b. Mechanism of excitation of the hair cells |
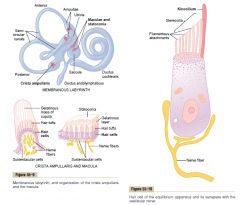
a.
1. Covered by gelatinous layer with calcium carbonate crystals called statoconia embedded into it 2. Hair cells a. Cilia project into the gelatinous layer b. Basolateral part synapse with sensory endings of vestibular nerves b. 1. The statoconia has a specific gravity 2-3 times that of the surrounding fluid and tissue. Gravitational forces act through the statoconiae to bend the cilia on the hair cells 2. The hair cells have several stereocilia (50-70, progressively lower away from the kinocilium) and one kinocilium located on one side of the cell. The apices are connected by filamentous attachments. 3. When the stereocilia bend against the direction of the kinocilium, the kinocilium via the filamentous attachments tug the stereocilia partly out of the cell membrane -> open cation channels (The reverse movement cause hyperpolarization by blocking the channels again) (Under normal resting conditions, the hair cells transmit nerve impulses at a rate of 100 Hz, increase to several hundred when they are further depolarized, while hyperpolarization can almost stop them from firing) (In each macula, some of the hair cells are oriented in a different direction so that there is always someone reacting to bending in a specific direction -> a different pattern of excitation occurs in the macular nerve fibers for each orientation of the head in the gravitational field) (Guyton) |
|
|
The crista ampullaris of the semicircular ducts
a. Mechanism of excitation of the hair cells b. What do they detect c. Lesion of which structure of the brain prevents normal detection of semicircular duct signals but has less effect on detecting macular signals |
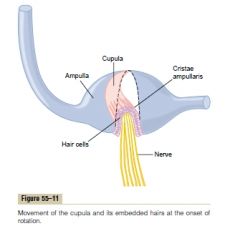
a. Mechanism of excitation of the hair cells
1. On top of the crista ampullaris is a gelatinous tissue mass called the cupula 2. When a person's head begins to rotate in any direction, the inertia in the fluid in one or more of the semicircular ducts cause the fluid to remain stationary while the semicircular duct rotates with the head -> fluid flow from the duct trough the ampulla -> bend the cupula to one side 3. Into the cupula are projected hundreds of cilia from hair cells The kinocilia of all these are located in the same direction, and bending in this direction cause depolarization and bending in the opposite way cause hyperpolarization. b. Detect angular acceleration (acceleration of rotation) (They predicts that dysequilibrium is going to occur and thereby causes the equilibrium centers to make appropriate anticipatory adjustments, before the macuale of the utricle and saccule are stimulated due to dysequilibrium.) c. The flocculonodular lobes of the cerebellum. (It is interesting to note that the cerebellum serves as a predictive organ for most rapid movements of the body, as well as for those having to do with the equilibrium.) (Reflexes transmitted from the semicircular ducts through the vestibular nuclei and medial longitudinal fasciculus to the oculomotor nuclei cause the eyes to rotate in a direction equal and opposite to the rotation of the head.) (Guyton) |
|
|
The vestibular apparatus
a. Other factors concerned with equilibrium b. Neural connections of the vestibular apparatus with the central nervous system |
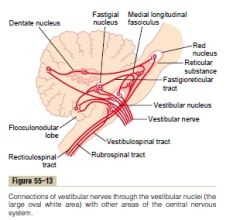
a. Other factors concerned with equilibrium
1. Neck proprioceptors (Bending of neck -> neck proprioceptors oppose equilibrium signals, bending of entire body does not give this effect) 2. Proprioceptive and exteroceptive information from other parts of the body - ie. differential weights placed on footpads 3. Visual information (some people with bilateral destruction of the vestibular apparatus have almost normal equilibrium as long as their eyes are open and all motions are performed slowly.) b. Neural connections of the vestibular apparatus with the CNS 1. Vestibular nerve fibers -> 2. Mostly vestibular nuclei (near pontomedullary junction). -> some directly without synapsing to the brain stem reticular nuclei, the cerebellar fastigial, uvular (essential for static equilibrium), and flocculonodular (essential for dynamic equilibrium signals from the semicircular ducts) lobe nuclei.) 3. --(2nd order neurons)--> 4a. Cerebellum 4b. Vestibulospinal tracts (Vestibulospinal and reticulospinal - these signals to the cord control the interplay between facilitation and inhibition of the antigravity muscles -> controlling equilibrium) 5c. MLF -> oculomotor nuclei -> corrective eye movements 5d. Other areas of the brain stem (Also pass up to a primary cortical center for equilibrium located in the parietal lobe deep in the sylvian fissure) (Guyton) |
|
|
The cerebellum
a. Contributions to overall motor control - functions (6) |
a. Important in
1. Timing of motor activities 2. Rapid, smooth, progression from one muscle movement to the next (By helping the cerebral cortex in planning the next sequential movement a fraction of a second in advance) 3. Help control intensity of muscle contraction when the muscle load changes 4. Control necessary instantaneous interplay between agonist and antagonist muscle groups. 5. Helps to sequence the motor activities 6. Makes corrective adjustments in the body's motor activities while they are being executed so that they will conform to the motor signals directed by the cerebral motor cortex (and other parts of the brain) (Compares the actual movements as depicted by the peripheral sensory feedback information with the movements intended by the motor system) (= Active during rapid muscular activities: running, typing, playing the piano) (Has the capability of learning by its mistakes - if a movement does not occur exactly as intended, the cerebellar circuits learns to make a stronger or weaker movement the next time) (Guyton) |
|
|
The basal ganglia
a. Contributions to overall motor control - functions |
a.
1. Help to plan and control complex patterns of muscle movement a. Control relative intensities of the separate movements b. Directions of movements c. Sequencing of multiple successive and parallel movements for achieving specific complicated motor goals |
|
|
Anatomical functional areas of the cerebellum - motor function, sensory functon, <-, ->
a. Vermis b. The intermediate zone of the hemispheres c. The lateral zone of the hemispheres |
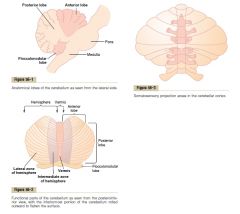
a. Vermis
Motor: Control functions for muscle movements of the axial body, neck, shoulders, and hips. sensory: Somatosensory for all the body except face and distal limbs <- represented parts of the body, corresponding topographical motor areas in the cerebral cortex and brain stem -> respective topographical areas of the cerebral motor cortex and topographical areas of the red nucleus and reticular formation b. Intermediate zone of the hemispheres Motor: Control muscle contractions in the distal portions of the limbs Sensory: somatosensory for the distal limbs and face <- represented parts of the body, corresponding topographical motor areas in the cerebral cortex and brain stem -> respective topographical areas of the cerebral motor cortex and topographical areas of the red nucleus and reticular formation c. Joins the cerebral cortex in the overall planning of sequential motor movements. <- cerebral cortex, especially premotor areas of the frontal cortex, somatosensory, and other sensory association areas of the parietal cortex -> same areas (Dysfunction of this structure -> most discrete motor activities of the body lose their appropriate timing and sequencing) (Guyton) |
|
|
Cerebellum - input pathways
a. Afferent pathways from other parts of the brain (4) b. Afferent pathways from the periphery (5) |
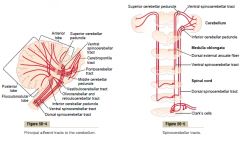
a.
1. Corticopontocerebellar pathway Cerebral motor cortex, cerebral premotor cortex, cerebral somatosensory cortex -> cerebropontile tracts -> pontile nuclei -> pontocerebellar tracts -> lateral divisions of the cerebellar hemispheres (contralateral to cerebral areas) 2. Olivocerebellar tract Cerebral motor cortex, basal ganglia, areas of reticular formation, spinal cord -> inferior olive -> cerebellum 3. Vestibulocerebellar fibers Vestibular apparatus, vestibular nuclei -> flocculonodular lobe, fastigial nucleus of cerebellum 4. Reticulocerebellar fibers -> Vermis mainly b. Afferent pathways from the periphery 1. Dorsal spinocerebellar tracts -> Inferior cerebellar peduncles -> ipsilateral vermis and intermediate zone of the hemishperes 2. Ventral spinocerebellar tracts -> superior cerebellar peduncles -> bilateral cerebellar projections 3. Spinal dorsal columns -> dorsal column nuclei of the medulla -> cerebellum 4. The spinoreticular pathway -> Reticular formation -> reticulocerebellar fibers 5. The spino-olivary pathway -> Inferior olivary nucleus -> olivocerebellar fibers (Guyton) |
|
|
The cerebellum
a. Signals transmitted in the dorsal spinocerebellar tracts b. Signals from the dorsal spinocerebellar tract apprise the cerebellum of the momentary status of (4) c. the neurons of the ventral spinocerebellar tracts are excited by |
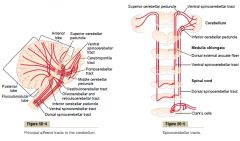
a.
1. Muscle spindles 2. Less from other somatic receptors such as Golgi tendon organs, tactile organs of the skin, and joint receptors b. 1. Muscle contraction 2. Degree of tension over muscle tendons 3. Position and rates of movement of the parts of the body 4. Forces acting on the surfaces of the body c. Motor signals arriving in the anterior horns of the spinal cord from the brain (corticospinal and rubrospinal tracts) and the internal motor pattern generators in the cord itself (tells the cerebellum which motor signals have arrived at the anterior horns - called the efference copy of the anterior horn motor drive)(fastest pathway in the brain - 120m\s) (Guyton) |
|
|
The cerebellum
a. Deep nuclei (3) b. Sources of input to the deep nuclei (2) c. efferent pathways |
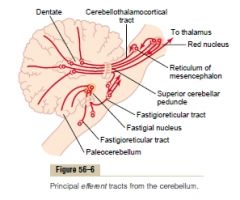
a.
1. The dentate nuclei 2. The interposed nuclei 3. The fastigial nuclei (The vestibular nuclei in the medulla also function in some respects as if they were deep cerebellar nuclei because of their direct connections with the cortex of the flocculonodular lobe) b. 1. From the cerebellar cortex 2. From the deep sensory afferent tracts to the cerebellum (Input -> deep nuclei, cerebellar cortex. Cerebellar cortex inhibit the deep nucleus. The output signals leave from the deep nuclei.) c. 1. Vermis -> fastigial nuclei -> medullary and pontine regions (Associated with the equilibrium apparatus and brain stem vestibular apparatus to control equilibrium) (Associated with the reticular formation to control postural attitudes) 2. Intermediate zone of the cerebellar hemisphere -> the interposed nucleus -> ventrolateral and ventroanterior nuclei of the thalamus -> cerebral cortex -> several midline structures of the thalamus -> the basal ganglia -> the red nucleus and reticular formation (Help to coordinate mainly the reciprocal contractions of agonists and antagonist muscles, especially distal to forearm) 4. The lateral zone of the cerebellar hemispheres -> dentate nucleus -> ventrolateral and ventroanterior nuclei of the thalamus -> cerebral cortex (Help coordinate sequential motor activities initiated by the cerebral cortex) (Guyton) |
|
|
The cerebellum
a. What is the functional unit of the cerebellar cortex? b. Layers of the cerebellar cortex c. What is the output part of the functional unit? d. What is the two different afferent inputs - where do they come from |
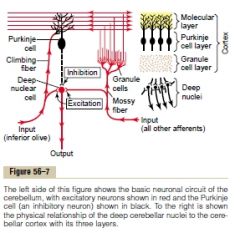
a. The Purkinje cell and the deep nuclear cell
(30 million) b. Superficial->Deep 1. Molecular layer 2. Purkinje cell layer 3. Granular layer (Beneath are the deep cerebellar nuclei) c. The deep nuclear cell. (Continually under both excitatory influence from afferent fibers from the brain or periphery and inhibitory influence from the Purkinje cell) d. Afferent inputs 1. The climbing fiber type <- the inferior olives of the medulla (Connect with both deep nuclear cell and purkinje cells) 2. The mossy fiber type <- All sources except the inferior olive nucleus (higher brain, brain stem, spinal cord) (Synapse with hundreds-thousands of granule cells in the granule cell layer -> axons to molecular layer (< 1 um, some of the thinnest (and therefore slowest)) -> branch in two in each horizontal direction -> (Stellate and Basket cells --(inhibitory)-> (Intermediate pathway for lateral inhibition)) dendrites of the purkinje cells (500-1000\Purkinje cell, 80 000-200 000 parallel fibers synapse with each Purkinje cell) (Larger numbers of mossy fibers than climbing fibers must be stimulated simultaneously to excite a Purkinje cell due to its weak synaptic connections.) (Guyton) |
|
|
The cerebellum
a. When the motor system is excited, a negative feedback signal occurs after a short delay to stop the muscle movement from overshooting its mark - where is the feedback signal from and how is it generated b. Basket and stellate cells - location, function |
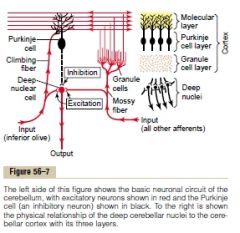
a. From the Purkinje cell.
Rapid motor movement -> mossy and climbing fibers greatly excite deep nuclear cells -(few ms delay)-> feedback inhibitory signal from Purkinje cell (Damping effect) (Purkinje cell inhibitory signal <- 1. From its intrinsic activity, 2. Climbing fiber -> stimulate Purkinje fiber -> inhibit deep nuclear cell, Mossy fiber -> stimulate granule cells -> parallel fibers stimulate purkinje cells -> purkinje cells inhibit deep nuclear cells (some delay in these pathways due to the higher-order) (This mechanism is probably responsible for the cerebellum's role in turn-on\turn-off and turn-off\turn-on (activate and inhibit agonist and antagonist muscle at initiation of movement, and the opposite at termination of movement.) mechanism, where the cerebellum plays an important part in timing. Cerebral cortex -> noncerebellar brain stem and cord pathways -> activate reciprocal inhibition pattern of agonist and antagonist, simultaneously parallel fibers are sent via pontile mossy fibers which via deep nuclear cells stimulate the pathway (strengthen turn-on\turn off) and after a short delay inhibit it (initiate turn-off\turn-on) (Damping: the capacity built into a mechanical or electrical device to prevent excessive correction and the resulting instability or oscillatory conditions.) b. In the molecular layer. Receive parallel fibers and send axons to cause lateral inhibition of adjacent Purkinje cells (Sharpening the signal) |
|
|
The cerebellum - The degree to which the cerebellum supports onset and offset of muscle contractions, as well as timing of contractions, must be learned by the cerebellum. Typically, when a person first performs a new motor act, the degree of motor enhancement by the cerebellum at the onset of contraction, the degree or inhibition at the end of contraction, and the timing of these are almost always incorrect for precise performance of the movement, but after the act has been repeatedly performed, the events become progressively more precise
a. What happens to the cerebellar circuit during the learning process b. How is this postulated to be achieved |
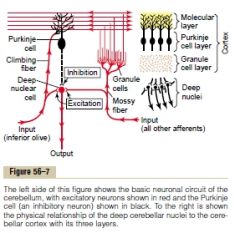
a. Sensitivity levels of cerebellar circuits progressively adapt, especially the sensitivity of the Purkinje cells to respond to the granule cell excitation becomes altered.
b. The climbing fibers from the inferior olive nucleus excite the Purkinje cells to cause complex spikes (long-duration). When a person performs a new movement, feedback signals from the muscle and joint proprioceptors feed back to the cerebellum and siganls it how much the actual movement fails to match the intended movement. As a result of this, the climbing fiber signals in some way alter long-term sensitivity of the Purkinje cells (Guyton) |
|
|
The vestibulocerebellum
a. Involved structures (6) b. Function c. Explain the anticipatory correction mechanism of the vestibulocerebellum for correction of postural motor signals necessary for maintaining equilibrium. |
a.
1. Flocculonodular cerebellar lobes 2. Vermis 3. Ventral part of the uvula 4. Small ventral parts of the lingula 5. Vestibular ganglion 6. Vestibular nuclei b. Help control equilibrium, especially during rapid motions and when they involve change in direction of movement and stimulation of the semicircular ducts. c. The signals from the periphery and vestibular apparatus tell the brain how rapidly and in which directions the body parts are moving. The vestibulocerebellum then calcuate in advance from these rates and directions where the different parts will be during the next few milliseconds. (Guyton) |
|
|
The spinocerebellum
a. Involved structures of the cerebellum (3) b. Input on the intermediate zone of the cerebellum (2) c. Role of the intermediate zone d. Role of the interposed nuclei |

a.
1. The intermediate zone 2. The vermis 3. The Interposed nucleus b. 1. Information about intended sequential plan of movement from the motor cortex (corticopontocerebellar tracts) and the red nucleus 2. Feedback information about the actual movements from the peripheral parts of the body (Especially the distal proprioceptors) c. Compare the intended movements with the actual movements -> transmit signal to the interposed nucleus d. <- Intermediate zone -> deep nuclear cells of the interposed nuclei -> 1. Cerebral motor cortex through relay nuclei in the thalamus -> corticospinal tract 2. The magnocellular portion of the red nucleus -> The rubrospinal tract (joins corticospinal tract) 1&2 -> Most lateral anterior motor neurons that innervate the distal parts of the limbs. (Thus the whole system help to provide smooth, coordinate movements of the agonist and antagonist muscles of the distal limbs for performing acute purposeful patterned movements.) (The ventral spinocerebellar tract transmits back to the cerebellum an efference copy of the actual motor control signals that reach the anterior motor neurons, this is integrated with the other peripheral afferent signals.) (Guyton) |
|
|
The cerebrocerebellum
a. Function b. Parts |
a. Plan, sequence, and time complex movements (intricate hand movements, speech), extramotor predictive functions (ie. predict from visual input when it will come in contact with an approaching object)
b. The lateral zones of the cerebellar hemispheres and the dentate nuclei <--> Premotor cortex, primary and association seomatosensory cortices (and to a less degree the primary motor cortex) (Seems that it starts in the sensory and premotor areas of the cortex and then is transmitted to the cerebellum, followed by active two-way traffic) (Guyton) |
|
|
Ballistic movements
a. What b. Examples (2) c. What change with these movements when the cerebellum is removed |
Movements that are performed so fast that there is not enough time for feedback information (either from periphery->cerebellum or cerebellum->motor cortex), so the entire movement is preplanned and set into motion to go a specific distance and then to stop.)
b. Saccadic (jerky\jumpy) movements of the eyes, movements of the fingers in typing c. 1. The movements are slow to develop and lack the extra onset surge that the cerebellum provides 2. The force developed is weak 3. The movements are slow to turn of, usually allowing the movement to go well beyond the intended mark (Inhibiting the turn-on\turn-off and turn-off\turn-on mechanism aided by the cerebellum) (Guyton) |
|
|
The putamen circuit
a. One of the principal roles of the basal ganglia in motor control is to b. Describe the Putamen circuit Abnormal function in the putamen circuit c. Lesion of globus pallidus often lead to d. Lesion of the subthalamus often lead to e. Multiple small lesiosn in the putamen lead to f. Lesions of the substantia nigra lead to |
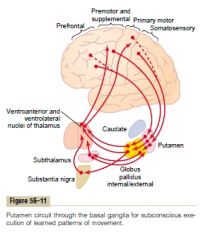
a. Function in association with the corticospinal system to control complex patterns of motor activity.
(Aspects of vocalization, shooting a basketball through a hoop, controlled movements of the eyes) b. Cerebral parts adjacent to the primary motor cortex (premotor, supplemental, somatosensory) -> Putamen -> internal portion of globus pallidus (pale) -> ventroanterior and ventrolateral relay nuclei of the thalamus -> primary, premotor, and supplementoary motor cortex (Accessory pathway from the putamen through the external globus pallidus, the subthalamus, and the substantia nigra) c. Athetosis (Spontaneous and often continuous writhing movements of a hand, an arm, the neck or the face) d. Hemiballismus (Sudden flexing movements of an entire limb) e. Chorea (Flickering movements in the hands, face, and other parts of the body) f. Parkinson's disease (Rigidity, akinesia, tremors) (Guyton) |
|
|
The caudate circuit
a. Responsible for what type of mtoor action b. Pathway |

a. Motor actions as a consequence of thoughts generated in the mind - cognitive control of motor activity
b. Pathway 1. Association areas of the cortex overlying the caudate nucleus -> (Caudate (head) - begin anteriorly in the frontal lobes, then pass posteriorly trough the parietal and occipital lobes to end up into the temporal lobes = large area of connection with the cortex) 2. Caudate nucleus -> 3. -> Internal globus pallidus -> 4. Ventroanterior and ventrolateral thalamus -> 5. Prefrontal, premotor, and supplementary motor areas (Motor areas concerned with putting together sequential patterns of movements lasting 5 or more seconds) (Guyton) |
|

Specific neurotransmitters in the basal ganglia system
|

(In addition to all these are multiple glutamate pathways that provide most of the excitatory signals that balance out the large number of inhibitory signals transmitted especially by the dopamine, GABA and serotonin.)
(Guyton) |
|
|
Parkinson's disease
a. Result from b. Signs & symptoms (3) c. Treatment options (3) |

a. Widespread destruction of pars compacta of substantia nigra, the portion that sends dopamine-secreting (inhibitory) nerve fibers to the caudate nucleus and putamen.
b. 1. Rigidity (Destruction of inhibitory signal -> caudate nucleus and putamen is not inhibited from becoming overly active and cause continuous output of excitatory signals to the corticospinal motor tract) 2. Resting tremor (3-6 Hz) (Involuntary tremor instead of intention tremor in cerebellar disease) (Loss of inhibition -> increased feedback gain -> tremor) 3. Akinesia (serious difficulty in initiating movement) (The mental effort, even mental anguish, that is necessary to make the desired movements is often at the limit of the patient's willpower.) (It has been suggested that the resulting simultaneous decreased dopamine secretion in the nucleus accumbens of the limbic system might reduce the psychic drive for motor activity so greatly that akinesia occurs) c. 1. L-Dopa (L-Dopa is converted in the brain into dopamine and alleviates especially the rigidity and akinesia, dopamine itself has poor penetrance through the BBB) 2. L-Deprenyl (MAO inhibitor, MAO destructs most of the dopamine after it has been secreted, for unknown reason, this helps to slow destruction of the dopamine-secreting neurons in the substantia nigra) 3. Treatments by destroying part of the feedback circuit in the basal ganglia (Ventroanterior and ventrolateral thalamic nuclei, subthalamic nuclei. Various results) (Guyton) |
|
|
Huntington's disease\Huntington's chorea
a. Caused by b. Symptoms c. structural and physiological mechanism |

a. Hereditary disorder caused by dynamic mutation of huntingtin gene
(repeating CAG codon coding for glutamine) (First cause symptoms at 30-40 years) b. 1. Flickering progressing to severe distortional movements of the entire body. 2. Dementia c. 1. Loss of most of the GABA-secreting neurons in the caudate nucleus and putamen and of acetylcholine-secreting neurons in many parts of the brain 2. The GABA-secreting neurons normally inhibit portions of the globus pallidus and substantia nigra, loss of inhibition -> spontaneous outbursts of globus pallidus and substantia nigra -> distortional movements The dementia is probably related to the loss of the acetylcholine-secreting neurons in certain areas of the cortex. (Guyton) |
|
|
The limbic system
a. What b. Parts c. Role of the subcortical areas, of the limbic cortex d. Connections between the limbic system and the brain stem |
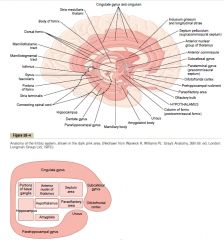
a. The entire neuronal circuitry that controls emotional behavior and motivational drives.
b. Interconnected complex of basal brain elements 1. The hypothalamus with its related structures (It also controls the vegetative functions of the brain: body temperature, osmolality of the body fluids, the drives to eat and drink etc. This vegetative control is closely linked to behavior.) (Central location) Subcortical structures of the limbic system 2. The septum area 3. The paraolfactory area 4. The anterior nucleus of the thalamus 5. Portions of the basal ganglai 6. The hippocampus 7. The amygdala The limbic cortex part of the limbic system. Ring of cerebral cortex (paleocortex) 8. Orbitofrontal area (ventral surface of the frontal lobes) 9. Subcallosal gyrus 10. Cingulate gyrus 11. Parahippocampal gyrus and uncus c. The subcortical areas are intimately associated with overall behavior and emotion, the limbic cortex (a paleocortical structure) functions as a two-way communication and association linkage between the neo-cortex and the lower limbic structures d. 1. Forebrain bundle: septal and orbitofrontal regions <--> middle of hypothalamus <--> the reticular formation 2. Thalamus, hypothalamus and other contiguous areas of the basal brain <--> the reticular formation (Guyton) |
|
The limbic system
|
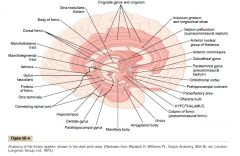
(Guyton)
|
|
|
Hypothalamus
a. It and its closely allied structures send output signals in three directions |
a.
1. Posterior and inferior -> brain stem: reticular areas -> peripheral nerves of the autonomic system 2. Superior -> many higher areas of the cerebrum (especially limbic portions) and diencephalon (especially anterior thalamus) 3. Hypothalamic infundibulum (Partially) Control most of the secretory functions of both the posterior and anterior pituitary glands (The hypothalamus is < 1% of the brain mass and a few cubic centimeters) (Guyton) |
|
|
Hypothalamus
a. It and its closely allied structures send output signals in three directions |
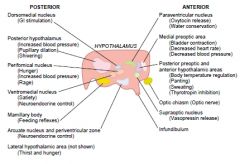
a.
1. Posterior and inferior -> brain stem: reticular areas -> peripheral nerves of the autonomic system 2. Superior -> many higher areas of the cerebrum (especially limbic portions) and diencephalon (especially anterior thalamus) 3. Hypothalamic infundibulum (Partially) Control most of the secretory functions of both the posterior and anterior pituitary glands (The hypothalamus is < 1% of the brain mass and a few cubic centimeters) (Guyton) |
|
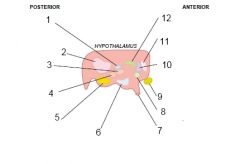
Control centers of the hypothalamus - name the different ones
|
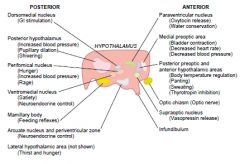
(Guyton)
|
|
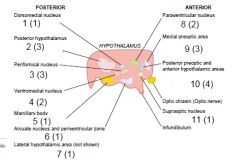
Control centers of the hypothalamus. List the functions for the different centers.
|
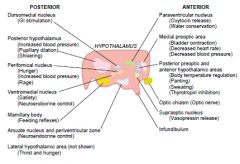
1. Dorsomedial nucleus
a. GI stimulatory 2. Posterior hypothalamus a. Increased blood pressure b. Pupillary dilation c. Shivering 3. Perifornical nucleus a. Hunger b. Increased blood pressure c. Rage 4. Ventromedial nucleus a. Satiety b. Neuroendocrine control (c. Tranquility) 5. Mamillary body a. Feeding reflexes (Licking the lips, swallowing) 6. Arcuate nucleus and periventricular zone a. Neuroendocrine control 7. Lateral hypothalamic area (not shown) a. Thirst and hunger (Thirst center, adjacent osmolality receptors) 8. Paraventricular nucleus a. Oxytocin release (Regulation of uterine contractility and of milk ejection by myoepithelial cells) b. Water conservation 9. Medial preoptic area a. Bladder contraction b. Decreased heart rate c. Decreased blood pressure 10. Posterior preoptic and anterior hypothalamic nucleus a. Body temperature regulation (Most important area for body temperature regulation, have temperature sensitive neurons) b. Panting (to breath rapidly in short gasps) c. Sweating d. Thyrotropin inhibition 11. Supraoptic nucleus a. Vasopressin release (Neurons sensitivity to osmolality) (12. Thin zone of periventricular nuclei: fear and punishment reactions. Also by stimulating central gray area of the mesencephalon that is continuous with this portion of the hypothalamus) (Sexual drive can be stimulated especially by the most posterior and anterior portions of the hypothalamus.) (Guyton) |
|
|
Rage
a. Stimulated by which areas b. Normally inhibited by which areas |
a. Strong stimulation of the punishment centers - the periventricular zone of the hypothalamus and the lateral hypothalamus
b. By inhibitory signals from 1. The ventromedial nuclei of the hypothalamus 2. Portions of the hippocami and anterior limbic cortex, especially in the anterior cingulate gyri and subcallosal gyri (Guyton) |
|
|
The hippocampal formation
a. Members b. The hippocampal formation has numerous but mainly indirect connections with c. Output of the hippocampal formation d. What is a special pathologically linked characteristic of the hippocampus e. What is the effect of bilateral removal of the hippocampi |
a. The hippocampus and its adjacent temporal and parietal lobe structures.
b. With many portions of the cerebral cortex as well as with the basal structures of the limbic system. (-> Almost any type of sensory experience causes activation of at least some part of the hippocampus) c. Extensive, mainly through the fornix to anterior thalamus, hypothalamus, and other parts of the limbic system. d. It can become hyperexcitable (Weak electrical stimuli can cause focal epileptic seizures associated with psychomotor effects such various hallucinations) (One of the reasons for this is probably that some part of the hippocampus only has three cell layers) e. Inability to consolidate memories. Anterograde amnesia. (Very early in evolutionary development of the brain, the hippocampi presumably became a critical decision-making neuronal mechanism, determining the importance of the incoming sensory signals. It seems to consolidate sensations by making the mind rehearse it over and over until the new information is permanently stored to some degree.) (Guyton) |
|
|
Dreaming
a. Difference between dreaming during slow-wave and REM sleep |
a. Those of REM sleep are associated with more bodily muscle activity, and the dreams of slow-wave sleep are usually not remembered (not consolidated into long-term memory).
(Guyton) |
|
|
REM sleep
a. Synonyms (2) b. Duration and frequency |
a.
1. Paradoxical sleep 2. Desynchronized sleep. b. 5-30 minutes, every 90 minutes in average. (Shorter when the person is extremely sleepy, increase during the night as the person becomes more rested.) c. 1. Associated with active dreaming and active bodily muscle movements (usually) 2. Waking from the REM stage The person is more difficult to arouse by sensory stimuli than during deep slow-wave sleep, yet people usually awaken spontaneously in the morning during an episode of REM sleep. 3. Muscle tone and movement Strongly inhibited throughout the body (Indicate strong inhibition of the spinal muscle control areas) Despite, irregular muscle movements do occur (in addition to REM) 4. Heart and respiratory rate usually become irregular (Characteristic of the dream state) 5. The brain is highly active (Overall brain metabolism may be increased as much as 20% and the EEG shows a pattern of brain waves similar to those that occur during wakefulness -> paradoxical sleep) (Guyton) |
|
|
Sleep
a. Sleep is believed to be caused by b. The most conspicuous area for causing almost natural sleep when stimulated is the raphe nuclei in the lower half of the pons and in the medulla. Where does neurons from here spread to (4)? what neurotransmitter is mainly secreted? |
a. An active inhibitory process
(Evidence: section at the level of the midpons creates a brain whose cortex never goes to sleep -> never fatigues as the passive theory of sleep assumes.) b. Spread to 1. The brain stem reticular formation 2. Thalamus, hypothalamus, and most areas of the limbic system 3. The neocortex of the cerebrum 4. Posterior horns of the spinal cord (Can inhibit sensory signals, including pain.) Serotonin (Blockage of serotonin formation in an animal makes the animal incapable of sleeping for the next several days) (Lesions of the raphe nuclei and the medial rostral suprachiasmal area in the anterior hypothalamus can cause intense wakefulness by releasing the excitatory reticular nuclei from its inhibition.) (Guyton) |
|
|
Sleep
a. Other possible transmitter substances related to sleep |
a. Muramyl peptide
(Increase in concentration in CSF and urine in animals kept awake for extended periods, induce sleep when injected into the brain ventricular system) (Also other substances) (Guyton) |
|
|
EEG and brain waves
a. Range of voltage recorded b. Range of frequency recorded c. The character or quality of the waves depends on, and change markedly during |
a. 0-200 uV
b. < 1 to > 50 Hz c. The degree of activity in respective parts of the cerebral cortex. Change markedly during the states of wakefulness, sleep, and coma. (Guyton) |
|
|
Brain waves and EEG - frequency, wave characteristics, when
a. Beta waves b. Alpha waves c. Theta waves d. Delta waves |

(Brain waves originate by numerous (> thousands) neurons firing synchronously. Strong nonsynchronous nerve signals often nullify one another in the EEG due to opposing polarities.)
a. Beta waves 14-80 Hz Asynchronous, lower-voltage than alpha waves Awake, high cerebration (Recorded mainly from the parietal and frontal regions during specific activation of these parts) b. Alpha waves 8-13 Hz, 50 uV Awake healthy adults during a quiet, resting state of cerebration (activity of the mental processes, thinking). (Most intense in the occipital region, to a less degree in the frontal and parietal regions.) (Result from spontaneous feedback oscillation in the diffuse thalamocortical system, possibly including the reticular activating system as well.) c. Theta waves 4-7 Hz, Children (parietal and temporal regions), some adults especially during disappointment and frustration, many brain disorders (often in degenerative brain states) d. Delta waves < 3.5 Hz, voltage is 2-4 x the other brain waves Very deep sleep, infancy, serious organic brain disease, (+ surgical anesthesia, stupor) (Present in animals having subcortical transections -> occur in the cortex indepdendent of activities in lower regions of the brain. Supported by the fact that delta wave occurs during deep slow-wave sleep when the cortex is mainly released from the activating influences of the thalamus and other lower centers.) (Guyton) |
|
|
Brain waves and EEG
a. What happens with the average frequency during increased degrees of activities b. what happens with the voltage during increased cerebration, why |

a. Increase progressively
b. Usually falls considerably, because the waves usually become asynchronous rather than synchronous and thus partially nullify each other. (Guyton) |
|
|
Changes in the EEG at different stages of wakefulness and sleep
a. Alert wakefulness b. Quiet wakefulness c. Slow-wave sleep - waves during the different stages d. REM sleep |

a. Beta waves
b. Alpha waves c. 1. Stage 1 sleep Low voltage, spindle-shaped bursts of alpha waves occurring periodically 2. Stage 2-4 sleep Frequency decrease gradually, delta waves of 1-3 Hz in stage 4 Voltage increase gradually d. Beta waves (Hard to differentiate from awake state. High-frequency and irregular <- origin of REM being called desynchronized sleep) (Guyton) |
|
|
Epilepsy ("Seizures")
a. Characterized by b. The three major types |
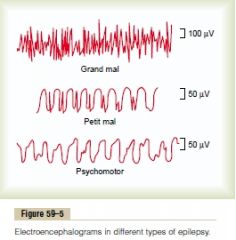
a. Uncontrolled excessive activity of either part or all of the central nervous system.
(A predisposed person has attacks when the basal level of excitability of the nervous system or the susceptible part of it rises above a certain critical threshold) b. 1. Grand mal epilepsy 2. Petit mal epilepsy 3. Focal epilepsy (Guyton) |
|
|
Grand mal epilepsy
a. What are the physioanatomical causes b. How is it stopped (2) c. What initiates a grand mal attack (6) d. Which parts of the nervous system are affected e. Characteristics of the EEG |

a. Massive simultaneous activation of many reverberating neuronal pathways throughout the brain.
b. Assumed to be stopped by neuronal fatigue and active inhibition by inhibitory neurons that have been activated by the attack. c. In a genetically predisposed individual (1\50-100) it is triggered by 1. Strong emotional stimuli 2. Alkalosis 3. Drugs 4. Fever 5. Loud noises or flashing lights 6. Hypoglycemia d. All of it, the cerebrum, the brain stem, and even the spinal cord (-> spinal cord -> generalized tonic seizures (followed toward the end by alternating tonic and spasmodic muscle contractions called tonic-clonic seizures), urination & defecation) e. High-voltage and high-frequency discharge over the entire cortex. (3-4 minutes on average, postictal depressed stupor states for many minutes after) (Guyton) |
|
|
Petit mal epilepsy
a. Caused by b. Typically affect who c. Typical course of a seizure |

a. Disturbances at the thalamocortical brain activating system
(Animal studies suggest that it results from oscillation of inhibitory thalamic reticular neurons (GABA) and excitatory thalamocortical and corticothalamal neruons.) b. Children (Appear first during late childhood and then disappear by the age of 30) c. 3-30 seconds of unconsciousness in which the person has twitch-like contractions of muscles usually in the head region (eyes) (This sequence is called the absence syndrome\epilepsy) (Can be one in months or rapid series of attacks) d. Spike and dome pattern (Can be recorded over most of the cerebral cortex, showing that the seizure involves much or most of the thalamocortical activating system) (Guyton) |
|
|
Focal epilepsy
a. Affected areas c. Causes (4) d. Pathophysiological mechanism - linked to Jacksonian epilepsy, grand mal epilepsy, and psychomotor seizure e. EEG characteristics |
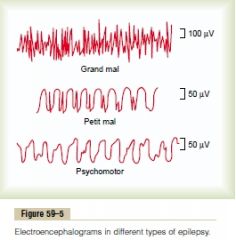
a. Almost any local part of the brain - regions in the cerebral cortex, deeper structures of the cerebrum, or the brain stem
b. Typically caused by some organic lesion or functional abnormality 1. Scar tissue (Pulls on the adjacent neuronal tissue) 2. Tumor (Compress) 3. A destroyed area of brain tissue 4. Congenitally deranged local circuitry d. Lesion\functional abnormality -> localized reverberating cirucits -> spread (recruit adjacent areas into the epileptic discharge zone) (mm\min-cm\s) -> 1. over cortex: contractions throughout opposite side of the body (This "marching" form over the motor cortex is called jacksonian epilepsy) 2. Spread to mesencephalic portion of reticular activating system -> grand mal seizure 3. Spread to limbic system -> psychomotor seizure (short period of amnesia, attack of abnormal rage, sudden anxiety\discomfort\fear, moment of inchorent speech or mumbling) (Can both not remember the event and remember the event, but not having conscious control over it) e. Low-frequency (2-4 Hz), rectangular waves (Sometimes with superimposed 14 Hz waves) (A surgical excision of the epileptogenic tissue frequently prevents future attacks.) (Guyton) |
|
|
Which two neurotransmitters are particularly linked to depression and manic-depressive psychoses
|
1. Norepinephrine
(Moderate number of norepinephrine-secreting neurons are located in the brain stem, especially in the locus ceruleus, these send fibers that project to most parts of the limbic system, thalamus, and cerebral cortex.) 2. Serotonin (There are many serotonin-producing neurons located in the midlien raphe nuclei of the lower pons and medulla that send fibers to many areas of the limbic system and to some other areas of the brain.) (Drugs that block these two, such as resorpine, frequently cause depression.) (70% of depressed patients can be treated effectively with drugs that increase the excitatory effects of these: MAO inhibitors, tricyclic antidepressants (imipramine, amitriptyline) (Drugs that diminish the formation or action of norepinephrine and serotonin, such as lithium compounds, can be effective in treating the manic phase of the condition) (Presumed that the norepinephrine and serotonin systems normally provide drive to the limbic areas of the brain to increase a person's sense of well-being, to create happiness, contentment, good appetite, appropriate sex drive, and psychomotor balance. <- Pleasure and reward centers receive large number of nerve endings secreting these neurotransmitters.) (Guyton) |
|
|
Schizophrenia
a. Characteristics of schizophrenic patients (5) b. Evidence for the theory that schizophrenia is caused by dysfunction in the prefrontal cortex c. Evidence for the theory that schizophrenia is caused by excessive excitement of a group of neurons that secrete dopamine in the behavioral centers of the brain - including the frontal lobes d. Evidence for the theory that schizophrenia is linked to abnormal function of a crucial part of the brain's limbic behavioral control system centered around the hippocampus |
a.
1. Hear voices and has delusions of grandeur (A false belief or wrong judgment held with conviction despite incontrovertible evidence to the contrary) 2. Intense fear or other types of feelings that are unreal 3. Highly paranoid (Often with a sense of persecution from outside sources) 4. Incoherent speech, dissociation of ideas, abnormal sequences of thoughts 5. Often withdrawn (Sometimes with abnormal posture and rigidity) b. Schizophrenic-like pattern of mental activity can be induced in monkeys by making multiple minute lesions in widespread areas of the prefrontal lobes. (Assumed to be due to blocking of signals or dysfunction of synapses that are normally excited by glutamate) c. 1. Many patients with Parkinson's disease who receive L-Dopa get schizophrenic-like symptoms 2. Most of the effective drugs (chlorpromazine, haloperidol, thiothixene) either decrease secretion or decrease the effect of dopamine on subsequent neurons (The dopamine-secreting neurons are postulated to lie in the ventral tegmentum of the mesencephalon, medial and superior to the substantia nigra. = Mesolimbic dopaminergic system. Project to medial and anterior portions of the limbic system, epsecially into the hippocampus, amygdala, anterior caudate nucleus and portions of the prefrontal lobes.) d. The hippocampus is often reduced in size in patients with schizophrenia. (Guyton) |
|
|
Alzheimer's disease
a. The three most common clinical features in the early stages b. A key role for the excess accumulation of beta-amyloid peptide in the pathogenesis of Alzheimer's disease is suggested by the following observations (5) |
a.
1. An amnesic type of memory impairment 2. Deterioration of language 3. Visuospatial deficits (Motor and sensory abnormalities, gait disturbances, and seizures are not common until a late stage of the disease) b. 1. All known mutations associated with Alzheimer's disease increase the production of beta-amyloid peptide 2. Patients with trisomy-21 (Downs syndrome) have three copies of the genes and develop neurological characteristics of Alzheimer's disease by midlife 3. Patients who have abnormality of a gene that controls apolipoprotein E (a blood protein that transports cholesterol to the tissues) have accelerated deposition of amyloid and greatly increased risk of Alzheimer's disease 4. Transgenic mice that overproduce the human amyloid precursor protein have learning and motor deficits in association with the accumulation of amyloid plaques 5. Anti-amyloid antibodies in humans with Alzheimer's disease appears to attenuate the disease process. (Guyton) |
|
|
Normal rate of cerebral blood flow
a. per 100 grams of brain tissue per minute b. For the entire brain per minute |
a. 50-65 ml\100 g brain tissue\ min
b. 750-900 ml\min (15% of cardiac output) (Guyton) |
|
|
Regulation of cerebral blood flow
a. The cerebral blood flow is autoregulated extremely well between mean arterial pressure limits of b. Effect of the sympathetic nervous system when the mean arterial pressure rises extremely high (as in strenuous exercise or during other states of excessive circulatory activity) on the cerebral vasculature |
a. 60-140 mmHg
(Up to 180 mmHg in people who have hypertension.) b. Constrict the large- and intermediate-sized arteries going to the brain enough to prevent the high pressure from reaching the smaller cerebral vessels. (Minimize cerebral vascular hemorrhages) (Guyton) |
|
|
The cerebrospinal fluid system
a. Volume of the entire cerebral cavity enclosing the brain and spinal cord b. How much of this capacity is occupied by cerebrospinal fluid c. Location of the cerebrospinal fluid (3) |
a. 1600-1700 ml
b. 150 ml c. In the 1. Ventricles of the brain 2. The cisterns around the outside of the brain 3. The subarachnoid space around the central nervous system (All are interconnected) (Guyton) |
|
|
Cerebrospinal fluid
a. Total amount b. Amount formed per day c. Sources (3) d. Pathway of CSF produced in the lateral ventricles |
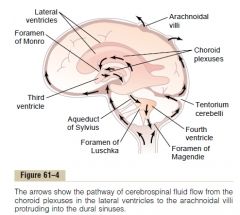
a. 150 ml
b. 500 ml c. 1. Secretion from the choroid plexuses in the four ventricles, mainly in the two lateral ventricles (2\3 of the total amount produced daily) 2. Secreted by the ependymal surfaces of all the ventricles and by the arachnoidal membranes 3. The brain itself through the perivascular spaces c. 1. Choroid plexuses of lateral ventricles -> 2. Foramen of Monro\Interventricular foramen -> (Short, slitlike passage that, on both the left and right side, connects the third brain ventricle (of the diencephalon) with the lateral ventricles (of the cerebral hemispheres), the passage is bound anteriomedially by the column of fornix and posterolaterally by the anterior pole and anterior tubercle of the dorsal thalamus) 3. Third ventricle -> 4. Aqueduct of Sylvius\Cerebral aqueduct -> (An ependyma-lined canal in the mesencephalon, about 20 mm long, connect the third and fourth ventricles) 5. Fourth ventricle -> 6. 3 canals a. 2 Lateral foramina of Luschka b. 1 midline foramen of Magendie 7. The cisterna magna\Posterior cerebellomedullary cistern -> 8. Subarachnoid space -> 9. Arachnoid villi -> 10. Sagittal venous sinus and other venous sinuses of the body (Guyton) |
|
|
The choroid plexus
a. Project into (3) b. Structure c. Relative composition compared to plasma - osmolarity, Na, K, Cl, Glucose |
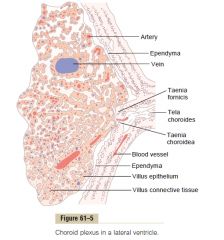
a.
1. The temporal horn of each lateral ventricle 2. The posterior portion of the third ventricle 3. The roof of the fourth ventricle b. Cauliflower-like outgrowth of blood vessels covered by a thin layer of villus epithelium c. Active transport of sodium by the villus epithelia, chloride follow due to generated charge differences, and water by osmosis. (Also transporters for glucose, and transporters moving K and HCO3 out) c. 1. Osmolarity - similar 2. Na - similar 3. K - lower (40% less) 4. Cl - slightly higher (15% higher) 5. Glucose - lower (30% less) (Guyton) |
|
|
Cerebrospinal fluid
a. How is it absorbed b. Where is the perivascular space c. 'Lymphatic system' in the brain |
a. Through arachnoidal villi.
I. Microscopic fingerlike inward projections of the arachnoidal membrane through the walls and into the venous sinuses (Conglomerates of these villi form macroscopic structures called arachnoidal granulations). The endothelial cells covering the villi have vesicular transcellular passages that allow relatively free flow of particles as large as white blood cells. b. Between larger vessels that penetrate into the brain and the pia mater surrounding them. (the pia is only loosely adherent to the vessels) c. Lymphatic function I. Transudate, cells and cellular debris due to infection -> perivascular spaces -> subarachnoid space (No lymphatics in the brain besides this) (Guyton) |
|
|
Cerebrospinal fluid pressure
a. Normal value when lying in a horizontal position b. The arachnoid villi functions like valves that only allow movement from the subarachnoid space to the venous sinus, how big must the pressure gradient be for cerebrospinal fluid to start flowing into the blood c. Causes of increased cerebrospinal fluid pressure (3) |
a. 10 mmHg
(130 mmH2O, normal range from 60-195 mmH20) b. 1.5 mmhg (Higher pressure -> higher flow) c. Causes of increased CSF pressure 1. Blockage of large brain tumor (CSF pressure can rise to 37 mmHg - 4x normal value) 2. Hemorrhage or infection in the cranial vault - the cells block the small absorption channels through the aracnhoid villi (Same pressure as above) 3. Congenital - high resistance to fluid reabsorption through the aracnhoidal villi <- too few villi, abnormal absorptive properties (Guyton) |
|
|
Papilledema
a. What b. Mechanism for formation in increased intracranial pressure |
a. Edema of the optic disk
(Often due to increased intracranial pressure) (Papilla = papilla nervi optici = optic disk = an oval area of the ocular fundus devoid of light receptors where the axons of the retinal ganglion cells converge to form the optic nerve) b. 1. The dura of the brain extends aroudn the optic nerve (and then connects with the sclera of the eye.) -> the increased ICP spreads to the optic nerve 2. High ICP push fluid a. First into the optic nerve sheath b. Second along the spaces between the optic nerve fibers to the interior of the eyeball 3. The high ICP decrease outward fluid flow in the optic nerves -> accumulation of excess fluid in the optic disk 4. The increased ICP impede venous return -> increase retinal capillary pressure -> increased edema 5. The tissues of the optic disc are more distensible than the rest of the retina, so that the disc becomes far more edematous than the remainder of the retina and swells into the cavity of the eye = papilledema (Guyton) |
|
|
Hydrocephalus - excess water in the cranial vault
a. Causes of noncoomunicating hydrocephalus b. Treatment |
a.
1. Block in the aqueduct of Sylvius (<- atresia (closure) before birth in many babies) 2. Blockage by brain tumor b. Placement of a silicone tube from the brain ventricles to the peritoneum. (Guyton) |
|
|
Blood-cerebrospinal fluid and blood-brain barriers
a. The barriers exist at both the choroid plexus and at the tissue capillary membranes in essentially all areas of the brain parenchyma except b. Give an example of a carrier molecule in the blood-brain barrier |
a. Some areas of the
1. Hypothalamus 2. Pineal gland 3. Area postrema (Chemoreceptor area associated with vomiting, small elevated area in the lateral wall of the inferior recess of the fourth ventricle) (These have sensory neurons and receptors that respond to osmolarity, glucose concentration, receptors for peptides (ie ATII) that regulate thirst) b. The carrier for leptin (Guyton) |
|
|
Brain edema
a. How does brain concussions cause brain edema b. Describe the two vicious positive feedback circles than can be initiated by brain edema c. How can the vicious circles be stopped (2) |
a. The brain tissues and capillaries become traumatized so that capillary fluid leaks into the traumatized tissue.
b. 1. Edema compress the vasculature -> Decrease blood flow -> brain ischemia -> arteriolar dilation -> increase capillary pressure further -> increased edema -->--> 2. Edema compress vasculature -> decreased cerebral blood flow -> decreased oxygen delivery -> increase the permeability of the capillaries -> increased edema -->--> c. 1. Adminster concentrated osmotic agent, such as Mannitol 2. Remove fluid quickly from the lateral ventricles by a ventricular needle puncture (Guyton) |
|
|
Brain metabolism
a. The total mass of the brain is only 2% of the body weight, how many % of the metabolism does the brain account for in an awake, relaxed state? b. How many seconds without blood flow to the brain does it take to cause unconsciousness c. How is glucose transported into neurons? |
a. 15%
(Under resting conditions, brain metabolism per unit mass of tissue is about 7.5 times the average metabolism in non-nervous system tissues) (Most is by the neruons, not the glial cells) (The neurons can increase their metabolism up to 150% during intense brain activity) b. 5-10s (The brain is not capable of much anaerobic metabolism, primarily due to its high metabolic rate) c. By insulin-independent glucose transporter. (Guyton) |
|
|
The autonomic nervous system
a. The autonomic nervous system is activated mainly by centers located in the .. (3) |
a.
1. The spinal cord 2. The hypothalamus (close association with cerebral cortex and limbic system) 3. The brain stem |
|
|
The sympathetic nervous system
a. Components (3) b. Point of origins in the spinal cord c. Where is the location of the preganglionic soma d. Describe the pathway from the spinal cord to the terminal organ |
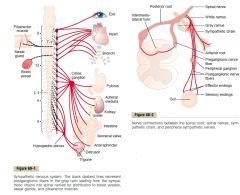
a.
1. The paravertebral sympathetic chains of ganglia (Interconnected with the spinal nerves on the side o fthe vertebral column) 2. Prevertebral ganglia (Arise from paravertebral sympathetic chain)(ie. celiac and hypogastric) 3. Nerves extending from the ganglia (paravertebral and prevertebral) to the different internal organs b. T1-L2 (-> Thoracolumbar) c. The intermediolateral horn of the spinal cord d. 1. Intermediolateral horn of spinal cord -> 2. Anterior root of spinal nerve -> spinal nerve -> 3. White ramus communicans -> 4. Ganglia of paravertebral sympathetic chain -> 5. 3 choices -> a. Synapse with postganglionic neuron in the ganglion that it enters b. It can pass up or down in the chain and synapse in one of the other ganglia of the chain c. It can pass for variable distances through one of the sympathetic nerves from the chain and synapse in prevertebral ganglion -> terminal "organ" via nerves extending from the ganglia or in skeletal nerves via the gray ramus communicans (Gray ramus communicans exist over the entire cord, type C nerve fibers, -> blood vessels, sweat glands, piloerector muscles, account for 8% of fibers in an average skeletal nerve) (Guyton) |
|
|
Splanchnic nerves
a. What b. The three groups - which, ->, what do they transmit |
a. One of the nerves supplying the viscera.
b. 1. Cardiopulmonary nerves Postganglionic sympathetic fibers to thoracic viscera 2. Abdominopelvic nerves Convey preganglionc sympathetic fibers to the sympathetic ganglia of the abdominal cavity 3. Pelvic splanchnic nerves Preganglionic parasympathetic fibers to the pelvic ganglia (Stedman) |
|
|
The parasympathetic nervous system
a. Leave the central nervous system through (2) b. The preganglionic fibers pass uninterrupted all the way to the organ that is to be controlled where the ganglion with the postganglionic cell is locateed in the wall of the organ. What are the exception this? |
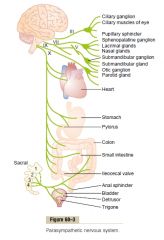
a.
1. CN III, VII, IX, X (75% of the parasympathetic nerve fibers) 2. 2nd and 3rd sacral spinal nerves (Occasionally the 1st and 4th as well) b. A few of the cranial nerves (CN III -> ciliary ganglion, CN VII -> sphenopalatine ganglion, submandibular ganglion, CN IX -> otic ganglion) (Guyton) |
|
|
Basic characteristics of sympathetic and parasympathetic function
a. Which of the postganglionic sympathetic neurons are cholinergic (3) |
a. Those that innervate
1. Sweat glands 2. Piloerector muscles 3. Some of the blood vessels (Guyton) |
|
|
Draw the molecular structure of acetylcholine.
|
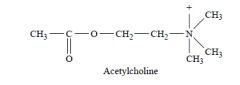
(Guyton)
|
|
|
Draw the molecular structure of norepinephrine.
What is the structural difference of norepinephrine and epinephrine. |
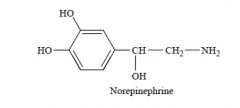
Epinephrine contains a methyl group connected to the amine radical.
(nor- is a chemical prefix for "stripped-down" molecules lacking groups, such as methyl groups, ie norepinephrine) (Guyton) |
|
|
Autonomic nervous system
a. What is the structural and functional equivalent to the neuromuscular junctions of the motor fibers - describe them |
a. Varicosities.
I. Bulbous enlargements of nerve filaments. II. Contain transmitter vesicles and mitochondria III. The mechanism for release is similar as in the neuromuscular junction, but they have more diffuse and weaker connections to the targets. (Some nerve terminals end in the surrounding connective tissue, some (especially parasympathetics) are very similar to the neuromuscular junctions, but are much smaller.) (Guyton) |
|
|
Acetylcholine
a. Site of synthesis b. The chemical synthesis c. How is it degraded |
a. Terminal endings and varicosities of the cholinergic nerve fibers.
b. Choline acetyl-transferase: choline + acetyl-CoA --> Acetylcholine (Then stored in vesicles in highly concentrated forms until it is released.) c. By acetylcholinesterase (-> choline + acetate), which is bound to collagen and glycosaminoglycans in the local connective tissue. (The choline is reabsorbed in the presynaptic neuron) (Guyton) |
|
|
Norepinephrine
a. Site of synthesis b. The steps of its synthesis (4) c. Mechanisms for removal (3) |
a. Begins in the axoplasm of the terminal nerve endings of adrenergic nerve fibers and is completed in the secretory vesicles.
b. 1. Tyrosine --(tyrosine hydroxylase)--> Dopa 2. Dopa --(dopa decarboxylase)--> Dopamine 3. Transport of dopamine into vesicles 4. Dopamine --(dopamine beta-hydroxylase)--> norepinephrine (Adrenal medulla: norepinephrine --(phenylethanolamine N-methyltransferase (use s-adenosylmethionine))--> epinephrine) c. 1. Reuptake into the presynaptic neuron (Active transport, 50-80%) 2. Diffusion away from the nerve endings into the surrounding body fluids and then into the blood (Account for removal of most of the remaining) 3. destruction of small amounts by tissue enzymes a. Monoamine oxidase (Found in nerve endings) b. Catechol-O-methyltransferase (Present diffusely in all tissues, mainly in the liver) (Guyton) |
|
|
Acetylcholine receptors
a. Where are muscarinic receptors found b. Where are nicotinic receptors found |
a.
1. All effector cells that are stimulated by the postganglionic cholinergic neurons of either the sympathetic or parasympathetic nervous system (Muscarine is a poison from toadstool (mushroom species) that only activate muscarinic receptors) b. 1. Autonomic ganglia at the synapses between preganglionic and postganglionic neurons of the autonomic nervous system 2. The neuromuscular junction (Nicotine activates only nicotine receptors) (Guyton) |
|
|
Eyes
a. Sympathetic stimulation cause b. Parasympathetic stimulation cause |
a. SNS - Contract the meridional fibers of the iris -> pupil dilation
b. PNS 1. Contract the circular muscle of the iris -> constrict the pupil (Light reflex) 2. Contract the ciliary muscle -> slacken lens radial ligaments -> allow the lens to become more convex (accommodation) (Guyton) |
|
|
The autonomic nervous system and glands of the body, effect of the sympathetic and parasympathetic nervous system on
a. The glands of the upper alimentary tract and the nasal and lacrimal glands b. The glands of the small and large intestine c. The sweat glands d. The apocrine glands |
a. Glands of upper alimentary tract, nasal glands, lacrimal glands
I. Parasympathetic nervous system stimuli cause copious quantities of watery secretion II. The sympathetic nervous system stimuli cause secretion of concentrated enzymes and mucus, vasoconstriction cause decreased secretion b. Only minor influence of the autonomic nervous system (Controlled by local factors in the intestinal tract itself and by the intestinal enteric nervous system.) c. Sweat glands PNS: no effect SNS: stimulatory effect to secrete large amounts of sweat (Stimulated primarily by centers in the hypothalamus (usually considered to be parasympathetic) and the postganglionic sympathetic neuron is cholinergic.) d. The apocrine glands PNS: no effect SNS: cause secretion of a thick, odoriferous secretion (Functions as lubricant to allow easy sliding motion of the inside surfaces under the shoulder joint) (Innervated by adrenergic fiber and controlled by the sympathetic centers of the central nervous system) (Guyton) |
|
|
Sympathetic and parasympathetic tone
a. What is sympathetic and parasympathetic tone b. What is the value of the basal tone c. Examples - sympathetic, parasympathetic d. What is the effect of loss of sympathetic or parasympathetic tone after denervation e. What is denervation supersensitivity |
a. The basal rates of activities of the two systems
b. It allows a single nervous system both to increase or decrease the activity of a stimulated organ. c. Vascular tone GI tone d. Intrinsic compensation (ie. contractility of smooth muscle) soon develops to return the function of the organ almost to its normal basal level. e. Increased sensitivity to the signal molecule after it has been removed. (Uncertain mechanism, partly by up-regulation of receptors) (Guyton) |
|
|
The autonomic nervous system
a. The sympathetic nervous system often responds by mass discharge throughout the body. Give examples of when activation occurs in isolated portions of the sympathetic nervous system b. The parasympathetic nervous system usually causes specific localized responses. Give two examples of when there is some association between closely related parasympathetic functions |
a.
1. Heat regulation - sweat gland, vascular tone of skin 2. Local reflexes 3. Many of the gastrointestinal reflexes - don't even enter the spinal cord. Sensory -> parevertebral ganglia -> gut b. 1. Simultaneous salivation, gastric secretion, and pancreatic secretion. Even though all three can be regulated individually. 2. The rectal emptying reflex often initiates a urinary bladder emptying reflex. (Guyton) |
|
|
Autonomic nervous system - how does the parasympathetic and sympathetic nervous systems affect
a. Blood coagulation b. Blood glucose c. Blood lipids d. Basal metabolism e. Mental activity f. Skeletal muscles g. Fat cells |
a. Blood coagulation
PNS: no effect. SNS: increased. b. Blood glucose PNS: no effect. SNS: increased. c. Blood lipids PNS: no effect. SNS: increased d. Basal metabolism PNS: no effect SNS: increased (up to 100%, beta-receptor mediated) e. Mental activity PNS: no effect SNS: increased f. Skeletal muscles PNS: no effect SNS: increased glycogenolysis and increased strength g. Fat cells PNS: no effect SNS: lipolysis. (Guyton) |
|
|
Function of ephedrine, tyramine, and amphetamine
|
Cause spontaneous release of norepinephrine from its storage vesicles
(Guyton) |
|
|
Name the drug that prevent the synthesis and storage of norepinephrine in the sympathetic nerve endings.
|
Reserpine.
(Adjunct agent to essential hypertension) (Guyton) |
|
|
Name two drugs that act as parasympathomimetics
|
Pilocarpine (only muscarinic) and methacholine (muscarinic and nicotinic).
(Acetylcholine administered intravenously does not cause the same effects throughout the body as parasympathetic stimulation because most of it is destroyed by cholinesterase in the blood and body fluids.) (Guyton) |
|
|
Function of neostigmine, pyridostigmine, and ambenonium
|
Cholinesterase inhibitors.
(Neostigmine - Myasthenia gravis, postoperative distention, urinary retention, antagonist of stabilizing neuromuscular blocking drugs (similar use as physostigmine)) (Pyridostigmine - Myasthenia gravis, reverse neuromuscular blockade produced by curare and similar agents at termination of a surgical procedure) (Ambenonium - Myasthenia gravis, intestinal and urinary tract obstruction) (Edrophonium - Short-duration, used as antidote for curariform drugs, as diagnostic agent in myasthenia gravis, myasthenic crisis) (Guyton) |
|
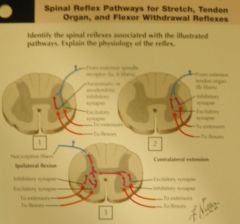
|
(Netter)
|
|
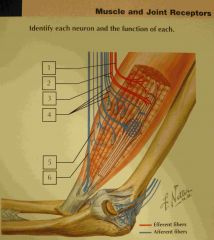
|
(Netter)
|
|

|
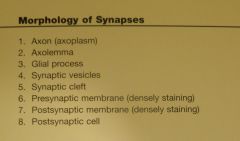
(Netter)
|
|

|

(Netter)
|
|

|
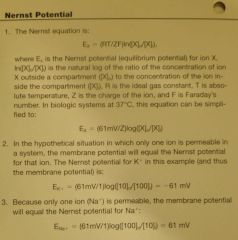
(Netter)
|
|
|
Serotonin\5-HT
a. Principally made in b. Number of receptors c. 5-HT3 - Clinically most important function, clinical application d. Which subreceptor mediate hallucination (and no other known function), and which agents work on it e. Which disorder is connected to serotonergic dysfunction, and how is it treated |
a. Raphe nuclei
(Nerve cell groups in and along the median plane of the medulla oblongata) b. 6 - 5-HT1-6, many has different subgroups as well. c. Involved in the pathway where toxic substances is detected by the area postrema (area in the lateral wall of the inferior recess of the fourth ventricle, lack BBB) and initiates vomiting. Blocked by -setrons (ondansetron). Used in chemotherapy. d. 5-HT2A Psilocybin (of magic mushrooms), LSD (Lysergic acid diethylamide), Meskalin) e. Depression 1. SSRI - Prozac (fluoxetine) 2. TCA (tricyclic antidepressants) (Also inhibit uptake of norepinephrine, 1950s, more effective than SSRI, but lower therapeutic window) (Ie. amitryptiline, imipramine) 3. MAO inhibitor (Non-selective and inhibit MAO peripherally (ie gut peristalsis) (Ie. hydrazines - hydralazine, iproniazid) (Trnka, Stedman) |
|
|
Noradrenaline
a. Principal nuclei b. Basic theory of depression, fallacy of this theory c. How is it involved in depression |
a. Locus ceruleus
(-> cerebellum, hypothalamus, cortex) (Bottom of fourth ventricle, part of RAS (stimulate aggressive behavior in the limbic system)) b. Too low serotonin and norepinephrine -> depression. Even though the neurotransmitter concentration rise within hours, the medications takes a couple of weeks to become effective. c. NA seems to be involved in the lack of energy component of depresison. (Explains TCA's higher efficacy compared to SSRI?) (Trnka) |
|
|
Amphetamines
a. Members b. Mechanism |
a.
1. Methoxy-diamine-meth-amphetamine (MDMA)(Ecstacy) 2. Ritalin 3. Amphetamines, Methamphetamines (#3 was used as an early antidepressant in the 30s, and used by the military as a stimulant) b. Interfere with transport of neurotransmitters into the secretory vesicles -> as they accumulate in the presynaptic nerve endings they begin to leak out uncontrolled. (Trnka) |
|
|
Cocaine
a. Symptoms (3) b. Mechanism |
a.
1. Euphoria 2. Energy 3. Potentiate other pleasurable things (food, drinks, sex) b. Inhibit the dopamine transporter (DAT) involved in reuptake. (Trnka) |
|
|
Dopamine (DA)
a. The four major pathways and their function b. Which two major disorders are linked to the dopaminergic system c. List the side effects of a dopaminergic antagonist according to the systems, with which condition would it be used |
a. The four major pathways and their function
1. Meso-cortical pathway I. Ventral tegmental area (VTA) of mesencephalon -> cortex (mostly frontal lobes II. 'Appropriate thinking' (Dysfunction: overactivation -> disorganized thought and speech pattern -> Schizophrenia) 2. Meso-limbic pathway I. Mesencephalon -> limbic system, especially amygdala and nucleus accumbens II. Involved in addiction (Cocaine and heroine's euphoria seems to be regulated via this system) 3. Nigro-striatal I. Substantia nigra (from crus cerebri to subthalamic region) -> Striatum II. Important in initiation of movement (Dysfunction -> Parkinson syndrome, elevated dopamine -> Parkinsonism) 4. Tubero-infundibular I. In hypothalamus II. Regulates secretion of prolactin, Dopamine\Prolactin-inhibiting factor (PIF) b. Which two major disorders are linked to the dopaminergic system 1. Parkinson disease, dysfunction of nigro-striatal system 2. Schizophrenia, overactivation of mesocortical dopaminergic system (Antipsychotics\Neuroleptics (European continental name) are mostly antagonists at the D2 receptor (ie. haloperidol, chlorpromazine), however, one of the most effective, clozapine, has almost no effect on the D2 receptors) c. Schizophrenia - ie. haloperidol 1. Nigrostriatal system -> Parkinsonism 2. Tubero-infundibular system -> hyperprolactinemia -> gynecomastia, amenorrhea, infertility 3. Meso-limbic system -> less ability to feel pleasure (Trnka) |
|
|
Rexed's zones
a. What b. Functions of the zones |
a. Separation of the gray matter of the spinal cord into 10 layers based on function.
b. Functions 1. Dorsal horns - Rexed's zones I-VI I. Sensory function 2. Lateral horns - VII I. Autonomic function 3. Ventral horns - VIII-IX I. Motor function 4. Zone X is around central canal I. Involved in integration of all functions (Slamberova) |
|
|
Eponyms of spinal cord fascicles
a. Fasciculus gracilis b. Fasciculus cuneatus c. Dorsal spinocerebellar tract d. Ventral spinocerebellar tract e. Rubrospinal tract |
a. Fasciculus gracilis\Goll
b. Fasciculus cuneatus\Burdach c. Dorsal spinocerebellar tract\Flechsig d. Ventral spinocerebellar tract\Gowers e. Rubrospinal tract\Monakow (Slamberova) |
|
|
The pyramidal\corticospianl tract
a. Origin b. Point of decussation |
a. Cells in layer V of the primary motor cortex.
b. Point of decussation I. 85% cross over in the pyramidal decussation in caudal medulla oblongata and forms lateral corticospinal tract II. 15% cross at the level they synapse with the ventral horn and form the medial\anterior corticospinal tract (Slamberova) |
|
|
Extrapyramidal motor systems - Parts and their function
|
1. Reticulospinal tract
I. Voluntary movements II. Autonomic functions 2. Vestibulospinal tract I. Posture II. Postural reflexes III. Voluntary and involuntary movements 3. Tectospinal tract I. Head movements based on the eye and ear inputs 4. Olivospinal tract I. Coordination (<- Cerebellum, striatum, cortex) 5. Rubrospinal tract I. Coordination (<- Cerebellum, motor cortex) (Slamberova) |
|
|
Respiration
a. Medullary centers for respiration - Which, function b. Pontine centers for respiration - Which, function |
a. Medullary centers for respiration
1. Dorsal respiratory group - Inspiratory II. Medullary reticular formation - part of solitary tract nucleus 2. Ventral respiratory group - Expiratory I. Part of reticular formation - 4 cell groups - Rostral nucleus retrofacialias, caudal nucleus retroambiguus, nucleus para-ambiguus, pre-Botzinger complex II. Inactive during normal quiet breathing II. Ventral and dorsal respiratory group exhibit reciprocal inhibition on each other's function b. Pontine centers for respiration 1. Apneustic center I. Part of reticular formation, caudal pons II. Apneusis - Inspiratory gasp (Generally, the apneustic center kicks the inspiratory center into gear if you go too long without breathing) III. Facilitates inspiration - prolong inspiration when your oxygen requirements become elevated, as during exercise (Help to control depth of respiration) IV. Activate dorsal respiratory group (If the brainstem is cut just above the apneustic center (damage connections of afferents from CN X and pneumotaxic center), apneustic breathing patterns will be induced (stop breathing, then inspiratory gasps)) 2. The pneumotaxic center I. Cranial pons II. Cuts of inspiration at a certain point to make sure that inspiration does not continue too long - Helps to control the rate of respiration in a sense (Achieve this by activating ventral respiratory group and inhibiting dorsal respiratory group) (Ie, lets say you were exercising strenuously and your inspiratory center was so hyperstimulated that it was trying to make you inhale when your lungs were already fully inflated, you need the pneumotaxic center to shut off the inspiratory center in such a case so that you can keep ventilating the lungs) (Slamberova) |
|
|
Cerebellum
a. General functions b. Layers of the cerebellar cortex c. Number of lobules d. Phylogenetic division of the cerebellum e. Functional divisions of the cerebellum |
a. General functions
1. fine-tune motor movements 2. Involved in language processing and selective attention (recent fMRI studies) b. 3 c. 10 d. Phylogenetic division 1. Archicerebellum\Vestibulocerebellum (Associated with flocculonodular lobe) 2. Paleocerebellum\Spinocerebellum (Associated with anterior lobe) 3. Neocerebellum\Cerebrocerebellum (Associated with posterior lobe) The oldest are closest to the brainstem) e. Functional division 1. Cerebellar vermis 2. Lateral hemispheres (Slamberova) |
|
|
Archicerebellum\Vestibulocerebellum
a. Associated with which cerebellar lobe b. <- c. -> d. Functions\Involved with e. Synonym |
a. The flocculonodular lobe
b. <- 1. Inferior and medial vestibular nuclei c. -> 1. Vestibular nuclei (Feedback loop) d. Function I. Continuous maintenance of balance I. Involved in eye movement functions e. Vestibulocerebellum (Slamberova) |
|
|
Paleocerebellum
a. Synonym b. Associated with which cerebellar lobe c. <- d. -> e. Function |
a. Spinocerebellum
b. Anterior lobe c. <- 1. Dorsal and ventral spincerebellar tracts (Ipsilateral involuntary proprioception) d. -> I. Deep cerebellar nuclei e. Maintenance of posture via muscle tone (Slamberova) |
|
|
Neocerebellum
a. Synonym b. Associated cerebellar lobe c. <- d. -> e. Function |
a. Cerebrocerebellum
b. Posterior lobe of cerebellum c. <- Pontocerebellar tract d. -> Deep cerebellar nuclei e. Function - Motor control I. Coordination of fine movements II. Feedback correction of motor activity III. Operates in conjunction with the cortical motor centers to plan movement (Slamberova) |
|
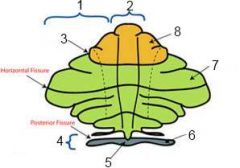
|
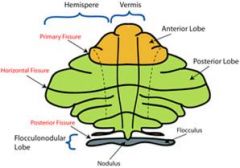
(Slamberova)
|
|
|
Cerebellum - Functional organization
a. Vermis - <-, ->, Function\involved in b. Intermediate zone\Paravermis - <-, ->, function\involved in c. Lateral zone - <-, ->, function\involved in |
a. Vermis
I. <- Spinocerebellar tracts about trunk mainly II. -> Fastigial nucleus -> vestibular nuclei III. Involved in position and balance b. Intermediate zone\Paravermis I. <- Corticopontocerebellar fibers <- motor cortex, <- spinocerebellar tracts (distal) II. Control of muscles c. Lateral zone I. <- Pontocerebellar mossy fibers <- parietal cortex (Integrated information regarding spatial position) II. Involved in integration of body position (Slamberova) |
|
|
Deep cerebellar nuclei
a. Location b. Which - from lateral to medial c. Input d. Most output of the cerebellum originates from these nuclei, what is the exception |
a. In the white matter of the cerebellum
b. From lateral to medial 1. Dentate nuclei (In lateral hemisphere) 2. Emboliform nuclei 3. Globose nuclei (2-3 in intermediate zone\paravermis) 4. Fastigial nuclei (In vermis) (Don't Eat Greasy Food) c. Input 1. Purkinje cells in the cerebellar cortex (Inhibitory GABAergic) 2. Mossy fiber pathways (Excitatory glutamatergic) d. Fibers from the flocculonodular lobe synapse directly on vestibular nuclei without first passing through the deep cerebellar nuclei. (Slamberova) |
|
|
Pain
a. Emotional\Psychological aspects influencing the pain perception b. Differences between acute and chronic pain - Duration, Causative factor, Carried by, Other |
a. Anxiety, sleep deprivation, fear.
b. Differences between acute (AP) and chronic pain (CP) 1. Duration I. AP - Short-lasting II. CP - > 6 months, or regular recurrences (Angina pectoris, neuralgias) 2. Causative factor I. AP - Normally ascertainable II. CP - Reason are not always known 3. Carried by I. AP - Abeta and Adelta fibers (6-30 m\s, Glu)) II. CP - C fibers (0.5-2 m\s, Glu & Substance P) 4. Other I. AP - Mostly don't repeat, ends when the lesion of the tissue which caused it is cicatrized (formed scar) II. CP - Intensity of pain is always higher than corresponding stimulation intensity. (Cause significant body suffering. Seriously influence the quality of life by increasing depression incidence and fear Needs repeated and permanent medical consultation and treatment) (Rokyta) |
|
|
Pathophysiological classification of pain, according to Lindblom
|
Pathophysiological classification of pain according to Lindblom
1. Nociceptive 2. Peripheral neurogenic (<- Neuropathies) 3. Central neurogenic 4. Dysautonomous pain (From sympathetic system dysfunction) 5. Visceral 6. Psychogenic 7. Nonspecified (Rokyta) |
|
|
Pain
a. Nocisensors\Nociceptors - Types b. Pain sensitization - Gene expression c. Pain mediators |
a. Nocicensors\Nociceptors
1. High-threshold mechanoceptors (Adelta -> fast conduction and localizeable. Responds to high pressure) 2. Polymodal nociceptors (<- Respond to various stimuli (noxious, mechanical, thermal (heat - Ruffini, cold: Krausse)), C-fibers -> Slow conduction and low accuracy, large receptive area) 3. Specific nociceptors - Free afferent nerve endings (Adelta, mechanothermal, responds to extreme hot or cold temperature) b. Pain sensitization - Gene expression 1. Increased Susbstance P NK1 receptors (Antagonist - MK0869\Aprepitant) 2. Increased calcitonin gene related peptide (CGRP) c. Pain mediators 1. Tetrodotoxin-resistant Na channels (TTX R) are opened 2. Postsynaptic receptors for excitatory transmittors are upregulated I. Glutamate NMDA II. Substance P - NK1 3. Activity of inhibitor systems is reduced I. Endogenous opioids II. GABA 4. ATP of deteriorating cells is liberated and probably operates as a pain transmitter I. Among ATP receptors are purinergic receptors - P2X 5. Vaniloid receptors (VR1) are activated 6. There are receptors for capsaicin which increase by deteriorating temperature 7. Acid-sensing ion channels (ASIC) are activated (Applied especially by acidification of tissue) (Rokyta) |
|
|
Neuropathic pain
a. Originates from b. Contributing factors |
a. From hypersensitivity of primary afferent fiber C and Adelta
b. Contributing factors 1. Ephatic transmission between peripheral nerve fibers (Sprouting to nearby fibers with transport of abnormal chemical mediators) 2. Change of the organization of neuronal responses 3. Channelopathy - Na, Ca, K (Rokyta) |
|
|
Algorithm of pain treatment
|
Algorithm of pain treatment
1. Physical therapy (Ie in lower back pain) 2. Pharmcotherapy - Non-opioidal (Antidepressants (NK1 receptor is both involved in pain and depression), antiepileptic drugs, capsaicin (found in chili) depletes substance P from nerve endings and is sometimes used for pain in postherpetic neuralgia) 3. Pharmacotherapy - Opioidal 4. Psychotherapy 5. Invasive methods I. Spinal neuromodulation (Stimulation) II. DREZ myelotomy (Dorsal root entry zone myelotomy), DREZ rhizotomy (Rhizotomy is also used for relief of spastic paralysis) 6. Non-invasive method I. Repetitive transcranial magnetic stimulation (rTMS) (Rokyta) |
|
|
Pain
a. Two characteristics of nociceptors b. Components of pain c. Gate theory |
a. Two characteristics of nociceptors
I. Nonadapting II. Hyperalgesia (Continuous stimulation of nociceptors increase sensitivity to pain receptors, so does inflammation) b. Components of pain 1. Sensory perception - How pain is felt 2. Affective component 3. Vegetative component - BP, HR, sweating (4. Motor component) c. Gate theory I. Proposed by Melzack and Wall (1963) II. Substantia gelatinosa is the modulating gate where non-noxious stimuli can modify pain (Bible) |
|
|
Pain
a. Pain stimulants b. Stimulants of nociceptors c. Mechanisms of increased sensitization of nociceptors |
a. Pain stimulants
1. Nociceptive agents I. Acids and alkali solution II. K ions III. Neurotransmitters - Histamine, Ach, Serotonin IV. Tryptamine V. Bradykinin VI. Proteolytic enzymes VII. Lactic acid 2. Tissue ischemia 3. Extreme heat or cold 4. Pressure 5. Painmodulating molecules I. Substance P II. Calcitonin-gene related peptide (CGRP) IV. Neurokinin A V. Prostaglandins b. Stimulants of nociceptors 1. Direct stimulation by nociceptive agents 2. Inflammation -> vasodilation & increased permeability -> edema -> pain from pressure c. Mechanisms for increased sensitization of nociceptors 1. Prostaglandins (PLs --COX--> prostaglandins) 2. Gene expression of NK1 receptor of substance P 3. Calcitonin-gene related peptide (CGRP) (Decrease pain threshold) (Bible) |
|
|
Descending analgesia system
a. What b. The analgesic effect arises from activation of descending pain-modulating pathways that project, via the medulla, to neurons in the dorsal horn. What are the three major structures involved b. Mechanism |
a. Pain control system
b. 1. Periaqueductal gray matter (Enkephalin) 2. Raphe nuclei (Serotonin) 3. Dorsal horn pain inhibitory system (Endorphins (beta-endorphin, dynorphin) and enkephalins (met-enkephalin, leu-enkephalin) b. Mechanism 1. Descending fibers from periaqueductal gray (enkephalin) and raphe nuclei (serotonin) stimulate dorsal horn pain inhibitory system -> 2. Dorsal horn pain inhibitory system secrete endorphins and enkephalins in substantia gelatinosa that inhibit input from C and Adelta fibers both pre- and postsynaptically (Cells in SG receive pain input from nociceptors and forward it to the lateral spinothalamic tract and thus determines the degree of pain felt. This analgesia lasts for minutes or even hours) (Other structures involved in the descending analgesia system - Reticular formation, locus ceruleus, parabrachial area, anterior pretectal nculeus, thalamus and cerebral cortex, several components of the limbic system) (Bible) |
|
|
Learning and memory - Definitions
a. Memory b. Learning |
a. Memory
I. Process of encoding, storing and retrieving of knowledge. b. Learning I. Generic term for the relatively permanent change in behavior that occurs as a result of practice. (Schutova, Stedman) |
|
|
Memory
a. Declarative memory - Components b. Nondeclarative memory - Components |

a. Declarative\Explicit memory
I. Semantic - Facts, names.. II. Episodic - Events b. Nondeclarative\Implicit memory I. Procedural - Memory of motor skills and habits II. Associative learning III. Non-associative learning - Sensitization, habituation (Habituation - The method by which the nervous systems reduces responsiveness during repeated stimulation. Sensitization is the opposite) IV. Priming (Priming is the implicit memory effect in which exposure to a stimulus influences response to a later stimulus.) (Classical conditioning\Stimulus substitution - Pavlov, A previously neutral stimulus becomes a conditioned stimulus when presented together with an unconditioned stimulus\The new stimulus evokes the response in question) (Unconditional stimulus - A stimulus that elicits an unconditional response, ie. food is an unconditional stimulus for salivation, which in turn is an unconditional response in a hungry animal) (Operant conditioning - Skinner box, Reinforce new behavior patterns by reward, funded on relationship between behavior and consequences) (Schutova) |
|
|
Declarative memory
a. Involved structures b. Effect of large cortical lesions on memory c. The four components of the information processing |
a. Involved structures
1. Hippocampal formation I. Dentate II. Hippocampus (Left - words, objects, people. Right - Spatial information) III. Subiculum IV. Entorhinal cortex 2. Perirhinal and parahippocampal cortex (Amygdala may play a modulatory part) 3. Neocortex - Multimodal association cortices (Prefrontal cortex is important for episodic memory) b. Retrograde amnesia c. The four components of the information processing 1. Encoding 2. Consolidation (Gradual process of reorganization and stabilization of different cortical representations of one memory) 3. Storage 4. Retrieval (Working memory is necessary for 1 and 4) (Schutova) |
|
|
Molecular approach to memory and learning. What was the conclusion of Ramon and Cajal in 1984
|
1. Learning does not result in proliferation of nerve cells
2. Learning cause neurons to I. Branch II. Strengthen their connections with other neurons (Schutova) |
|
|
Molecular approach to learning
a. Memory trace b. Habituation c. Sensitization |
a. Memory trace
I. The hypothetical structural alteration in neurons following learning II. Based on change in synaptic transmission - facilitation or depression b. Habituation I. Weakening of synaptic transmission - Depression I. By decreased release of neurotransmitter short-term (Seconds) and by decreasing number of synapses long-term (Weeks) c. Sensitization\Facilitation I. Facilitation of synaptic transmission II. Short and long term as with habituation (Involved serotonergic facilitatory interneuron activating G protein-coupled receptors?) (Schutova) |
|
|
Memory
a. What did Bliss and Lomo discover in 1973 b. Which related discovery did Morris make |
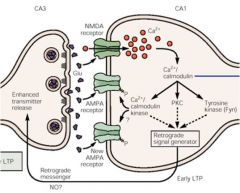
a. The remarkable plasticity of hippocampus - termed long-term potentiation (LTP)
I. A brief high-frequency sequence of APs produce an increase in synaptic strength lasting hours to days (Mediated by glutamate, NMDA and non-NMDA receptor postsynaptically) b. Pharmacological blockade of NMDA receptors caused animals to navigate in maze but not remember the information. (Also proven by NMDA-receptor knock-out strains of mice. Also necessary for declarative memory) (Schutova) |
|
|
Memory - Mechanisms
a. Short-term memory - Synaptic\Molecular mechanism b. Long-term memory - Synaptic\Molecular mechanism |
a. Short-term memory - Synaptic\Molecular mechanism
I. Change of pre-existing proteins - phosphorylation, dephosphorylation b. Long-term memory - Synaptic\Molecular mechanism 1. Synthesis of new proteins I. Increased number of transmitter releasing sites II. Increased number of vesicles III. Increased number of presynaptic 2. Growth of new synapses 3. change of dendritic spines postsynaptically (Schutova) |
|
|
Sleep
a. The 4 behavioral criteria b. Polysomnography - What, The 3 parameters needed to distinguish sleep from wakefulness c. Two characteristic EEG findings in nREM stage 2 sleep |
a. 4 behavioral criteria
1. Decreased motor activity 2. Decreased responsiveness 3. Stereotype posture 4. Reversible b. Polysomnography I. Simultaneous and continuous monitoring of relevant normal and abnormal physiologic activity during sleep II. Need 3 parameters to distinguish sleep from wake state - EEG, EMG, EOG (EOG - Electrooculography - Electrodes placed on the skin adjacent to the eyes) c. K-complexes and sleep spindles (Schutova) |
|
|
nREM sleep
a. Stages b. Characteristics of EEG c. Characteristics of brain, muscle, reflexes, and autonomic nervous system |
a. 1-4
b. Highvoltage, slow waves c. Characteristics I. Low metabolism -> low nerve activity, low brain temperature II. Muscle tone and reflexes present III. Increased activity of parasympathetic NS (Schutova) |
|
|
nREM sleep
a. Stage 1 - Behavior, muscle tone, eyes b. Stage 2 - Behavior, eyes, EEG c. Stage 3-4 - EMG, EEG, behavior |
a. Stage 1
I. Sleepiness, transition to sleep, decreased responsiveness II. Decreased muscle tone III. Slow eyes b. Stage 2 I. Quiet sleep without movements, strongly decreased responsiveness II. No eye movements III. Sleep spindles and K-complexes on EEG c. Stage 3-4 I. Highest threshold for awakening II. EEG - Delta waves (slow-wave) III. EMG - Low tone (Schutova) |
|
|
REM sleep\Paradoxical sleep
a. Neural activity b. Muscle c. Autonomic nervous system d. Other characteristics |
a. Increased relative to nREM.
(Increased metabolism, increased brain temperature) b. Atony of almost all skeletal muscles except diaphragm and oculomotor muscles c. Increased parasympathetic tone d. Dreams (Schutova) |
|
|
Sleep cycle
a. Average length b. Changes in relative parts spent in the different stages during sleep d. Sleep of newborn - Length, relative time spent in different phases e. Trends of sleep into adulthood and senescence |
a. 90-110 minutes
(-> 4-6\night) b. nREM III-IV shortens and REM lengthens (50-60% in nREM II, 25% REM, 15-25% nREM III, 5% nREM IV) d. Sleep of newborn I. 17-18 hours a day (3-4 hours sleep interrupted by feeding) II. 50% in REM, almost no slow-wave sleep e. Slow-wave decrease (little after 50 years) (Schutova) |
|
|
Nuclei responsible for n-REM and REM sleep
|
1. RF in medulla is active in sleep
(RF in mesencephalon is active in wakefulness) 2. Anterior hypothalamus contains nREM-on cells I. GABAergic II. Cause sleep by inhibiting posterior hypothalamus and RF in mesencephalon (Posterior hypothalamus is involved in wakefulness, histaminergic) 3. Reticular nucleus of thalamus -> Slow-wave sleep (Sleep spindles) I. GABAergic 4. Ncl reticularis pontis -> REM sleep I. Acetylcholine II. -> Atonia III. Inhibit reticular nucleus of thalamus (Schutova) |
|
|
Sleep
a. Significance |
a. Significance of sleep
1. Conservation of energy (<- Increased food intake after sleep deprivation, decreased BMR during sleep, people with increased metabolic turnover have more delta sleep) 2. Cognitive functions (Cognition deteriorate after sleep deprivation, consolidation in REM sleep (but learning is possible also without sleep)) 3. Thermoregulation (Cooling of the organism, increased heat loss from acral body parts during sleep) 4. CNS maturation (High REM-content sleep in newborns) (Schutova) |
|
|
Chronobiology
a. Chronobiology b. Circadian rhythm c. Ultradian rhythm d. Infradian rhythm |
a. Chronobiology
I. The aspect of biology concerned with the timing of biological events, especially repetitive\cyclic phenomena b. Circadian (circa, dies - day) rhythm I. Biological rhythms with a cycle of about a day c. Ultradian rhythm (More) I. Biological rhythms\variations with cycle more frequent than every day d. Infradian rhythm (Less) I. Biological rhythm\variation with cycles occurring less frequently than once a day (Schutova) |
|
|
Circadian rhythms
a. Is the circadian rhythm dependent on external stimuli b. Which nuclei functions as the internal oscillator (determinant of frequency) or internal 'biological clock' c. External stimuli act as synchronizers - Which factors affect the internal oscillator d. Peripheral oscillators - What, ie |
a. No, its endogenous.
(It persists even if the influence of the environment is blocked, as in blind people) b. Suprachiasmatic nucleus (SCN) (Core - input of information about light changes, shell - synchronization of neurons. VIP, switching on & off the transcription of the 'clock genes (influenced by the synchronizers)) c. Synchronizers 1. Light and dark (Main synchronizer for humans, via retinohypothalamic tract) 2. Activity 3. Melatonin (<- Pineal gland, increase 10-fold just before sleep and peak around midnight, the decline of melatonin secretion with age has been blamed for the increased incidence of insomnia in the elderly) 4. Temperature 5. Food intake d. Peripheral oscillators I. In every cell II. Synchronized by SCN and affected by changes in their surrounding environment II. Ie GIT cells and food intake (Schutova) |
|
|
Circadian rhythms
a. Changes in the morning b. Changes in the day c. Changes in the evening |
a. Morning
I. Increased body temperature II. ACTH and cortisol peak b. Day I. Increased activity II. Decrease of melatonin c. Evening I. Decrease of body temperature (Via acral vasodilation, temperature is lowest at biological midnight) II. Lowest cortisol and ACTH levels III. Low activity IV. Melatonin peak -> onset of sleep (Schutova) |
|
|
Circadian rhythms
a. Jet-lag - What, S&S b. Jet-lag - Effect of west-east flight c. Therapeutical uses for melatonin |
a. Jet-lag
I. Circadian rhythm sleep disorder resulting from rapid long-distance transmeridian travel II. S&S - Headache, fatigue, dyssomnia, digestive problems (Dyssomnia - disturbance of normal sleep or rhythm pattern) b. West->East flight I. Shortening of the rhythms (cycle < 24 hours) II. Dark period is shorter -> must wake up earlier (Accommodation is harder and slower than the other-way-around) c. Melatonin - Indications 1. Avoiding jet-lag 2. Blind people - To ease synchronization of circadian rhythm 3. Insomnia in elderly patients (Schutova) |
|
|
Thalamus
a. Specific relay nuclei - What b. Medial geniculate body - <-, -> c. Lateral geniculate body - <-, -> d. Ventral posterior nucleus (VP) - Components with <- and -> |

a. Specific relay nuclei
I. Nuclei that project fibers and receive fibers from well-defined areas of the cerebral cortex that are considered to be related to a specific function. b. Medial geniculate body I. <- Auditory information mostly arising from the inferior colliculi II. -> Auditory radiations -> Auditory cortex (41,42)(Heschl's transverse gyri) c. Lateral geniculate body I. <- Optic tract II. -> Visual radiations -> Calcarine cortex (17) d. Ventral posterior nucleus (VP) (1-2 Collectively called ventrobasal complex) 1. Ventral posterior lateral (VPL) nucleus I. <- Medial lemniscus and spinothalamic tract II. -> Primary somesthetic area in the postcentral gyrus (1,2,3) 2. Ventral posterior medial (VPM) nucleus I. <- CN V analogue II. -> Primary somesthetic area in the postcentral gyrus (1,2,3) 3. Ventral medial (VM) nucleus I. <- Parabrachial nuclei of the reticular formation (Taste) II. -> Primary gustatory area (43) (Generally - Dorsal thalamus is comprised of roughly 15 nuclei with relay cells that project to the cerebral cortex. Ventral thalamus (mainly represented by GABA-ergic reticular nucleus) project into the dorsal thalamus to inhibit relay cells) (Zack) |
|
|
Thalamus
Specific relay nuclei a. Ventral lateral (VL) - <-, -> Less specific or association nuclei b. Where does the projections from these less specific nuclei generally go c. Anterior nucleus - <-, -> |

a. Ventral lateral (VL) nucleus
I. <- Superior cerebellar peduncle <- contralateral cerebellar cortex (pars caudalis\posterior part of VL), ipsilateral striatum (pars oralis\anterior part of VL) (Information dealing with motor control) II. -> Primary motor cortex (4), Premotor cortex (6), and supplemental motor area (8) (Complete the feedback system of the motor nuclei mechanisms) b. To the association areas of the cerebral cortex c. Anterior nucleus I. <- 1. Mammillary bodies via mammillothalamic tract 2. Other hypothalamic nuclei 3. Cingulate gyrus II. -> 1. Cingulate gyrus 2. Cerebral cortex 3. Hypothalamus 4. Hippocampus (+ Collaterals to other limbic system structures) (This nuclei is involved with memory, learning, and emotional behavior relating to our basic drives for food, shelter, and sex. This nucleus also works closely with other limbic system structures in the coupling of our autonomic functions and emotional behaviors) (Zack) |
|
|
Thalamus - Less specific or association nuclei
a. Medial dorsal nucleus - <-, ->, Function b. Lateral nucleus - <-, -> c. Posterior group nuclei - <-, -> d. Pulvinar nuclei - <-, -> |

a. Medial nucleus
I. <- 1. All major afferent tracts 2. Hypothalamus 3. Amygdala 4. 9,10,11,12 of prefrontal cortex II. -> 1. Prefrontal cortex (9,10,11,12) 2. Hypothalamus 3. Hippocampus 4. Striatum III. Deals with our emotional response in relation to our external and internal environment, also deals with it the other way around - emotional state -> autonomic responses b. Lateral nucleus I. <- Hypothalamus, cingulate gyrus II. -> Cingulate gyrus, other limbic system structuers (Associated functionally with anterior nucleus in regard to our basic emotional drives) c. Posterior group nuclei I. <- Pain from lateral spinothalamic tract and CN V II. -> Insular cortex (Part of a system dealing with the total conscious perception of pain at the cortical level) d. Pulvinar nuclei I. Reciprocal connections with association areas of the parietal, occipital, and temporal lobes (Involved in integration of all incoming sensory input to allow for total comprehension of that moment in time when we are experiencing it) (Zack) |
|
|
Hypothalamus
a. ADH is primarily formed in b. Oxytocin is primarily formed in c. In the anterior pituitary gland there are chromophobe and chromophilic cells. The chromophobes are mostly inactive cells with only a few secretory granules. The chromophils are active cells and we have two types - What are these and what do they secrete |
a. Magnocellular neurons in supraoptic nuclei -> ADH
b. Magnocellular neurons in paraventricular nuceli -> Oxytocin c. Chromphils 1. Acidophils I. Somatotrophic cells - hGH (50% of total secretory cells) II. Lactotrophic cells - PRL (10-30%) (The acidophilic cells make up the cells which secrete hormones that don't act on a primary gland) 2. Basophilic cells I. Corticotrophic cells -> ACTH (10%) II. Thyrotrophic cells -> TSH (5%) III. Gonadotrophic cells -> FSH, LH (20%) (Slamberova) |
|
|
hGH
a. Mechanisms for increasing protein deposition b. Mechanisms for increasing fat utilization for energy c. Mechanisms for decreasing carbohydrate utilization |
a. Mechanisms for increasing protein deposition
1. Enhance AA transport through the cell membrane 2. Enhance transcription and translation 3. Decrease catabolism of proteins and AAs (Cartilage and bone are the main tissues of hGH effect. Also cause increased rate of reproduction of these cells and conversion of chondrocytes to osteogenic cells) b. Mechanisms for increasing fat utilization for energy 1. Increased release of FAs from adipose tissue -> Increase in FA concentration in plasma 2. Increased FA -> Acetyl Coa conversion (GH have a ketogenic effect - Ketosis may occur when the amount of hGH is too high and causes great mobilization of fatty acids from adipose tissue that requires large amounts of acetoacetic acid to be formed by the liver) c. Mechanisms for decreasing carbohydrate utilization 1. Decrease in glucose uptake in tissues (Skeletal muscles, fat) 2. Increase in glucose production by the liver 3. Increase in insulin secretion (Diabetogenic effect - Induce insulin resistance. Oppose insulins effect on stimulating uptake and utilization of glucose in skeletal muscle and fat, and to inhibit glucose output by the liver) (Slamberova) |
|
|
Midbrain - Tectum
a. Tectum - Divsion of the midbrain, Components b. The superior colliculus - Involved with, -> c. The inferior colliculus - Involved with, -> |
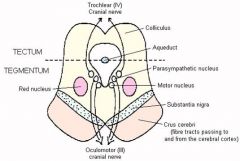
a. Tectum
I. Posterior to cerebral aqueduct II. Inferior and superior colliculi -> Quadrigeminal body b. Superior colliculus I. Involved with preliminary visual processing - Include 1. Saccadic eye movements 2. Eye-head movements 3. Pupillary light reflex II. -> Lateral geniculate nucleus -> primary visual cortex c. Inferior colliculus I. Involved in preliminary auditory processing and head-ear movements induced by sound stimulus II. -> Medial geniculate nucleus -> primary auditory cortex (Slamberova) |
|
|
Midbrain - Tegmentum
a. Tegmentum - Location, components b. The ventral tegmental area (VTA) - Neurotransmitters, part of two major dopamine pathways c. The ventral tegmental area -- Function |
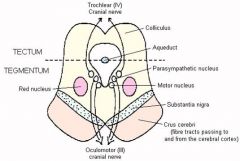
a. Tegmentum
I. Between the substantia nigra and cerebral aqueduct II. Ventral tegmental area and red nucleus b. Ventral tegmental area I. Rich in dopamine and serotonin neurons II. Part of two major dopamine pathways 1. The mesolimbic pathway - VTA -> Nucleus accumbens 2. The mesocortical pathway - VTA -> Parts of frontal lobe c. The ventral tegmental area I. Part of the pleasure\reward system (Sources of incentive and behavioral motivation) (Psychostimulants such as cocaine directly target VTA -> implied neurobiological theories of addiction) II. May be involved in avoidance and fear-conditioning (Slamberova) |
|
|
Substantia nigra
a. Location b. Main neurotransmitter c. Components |
a. Part of midbrain
b. Dopamine (Main site for dopaminergic neurons in the brain -> Vital role in reward and addiction) c. Components 1. Pars compacta (Contains neurons which are colored black (black stripes) by the pigment neuromelanin that increases with age) 2. Pars reticulata - Dendrites from pars compacta neurons (One of the two primary output nuclei of the basal ganglia along with internal segment of globus pallidum) (Slamberova) |
|
|
Basal ganglia
a. Interconnections b. General functions c. Components |

a. Interconnections with the cerebral cortex, thalamus, and brain stem.
b. General functions 1. Motor control 2. Cognition 3. Emotions 4. Learning c. Components 1. The striatum I. Putamen II. Caudate (III. Nucleus accumbens - The region of fusion between the head of the caudate and the putamen. Not considered part of striatum in Stedman's) 2. Globus pallidus 3. Subthalamic nucleus 4. Substantia nigra - SNpc, SNpr (Slamberova) |
|
|
Nucleus accumbens
a. Nucleus accumbens and other structure forms .... b. Function c. Parts d. Types of neurons |
a. Nucleus accumbens and the olfactory tubercle form the ventral striatum
b. Function - Involved in 1. Reward 2. Pleasure and laughter 3. Addiction 4. Placebo effect c. Parts - core and shell d. Types of neurons 1. Mainly GABA-ergic (95%) 2. Cholinergic interneurons (Slamberova) |
|
|
Caudate nucleus
a. Input b. Functions\Involved with c. Related pathologies |
a. Input - dopaminergic neurons from VTA and SNpc
b. Functions 1. Control of voluntary movement 2. Involved with the brain's learning and memory system 3. Left caudate is implied in language comprehension (Increased activity observed on fMRI during falling in love, along with ventral tegmental area.) c. Related pathologies 1. Huntington's disease 2. OCD (Slamberova) |
|
|
Thalamus
a. Non-specific sensory nuclei - What b. Which |
a. Unspecific function, part of ascending tracts from RF going to cortex
b. Components 1. Nucleus centralis lateralis 2. Nucleus centralis medialis 3. Nucleus parafascicularis 4. Nucleus habenularis (Important for pain information) (Slamberova) |
|
|
Dopamine
a. Subtypes of receptors b. Function in hypothalamus c. Effect on autonomic nervous system d. Effect in CNS e. Pathologies associated with dysfunction |
a. D1-D5, with further subdivisons.
b. Neurohormone - inhibits the release of prolactin form the adenohypophysis c. Catacholaminergic - Ie increase heart rate and BP (Can't cross the BBB so giving it directly won't affect its function as a central neurotransmitter) d. Effect in CNS - 1. Involved in reward system. Increased when an unexpected reward is presented. Believed to provide a teaching signal to parts of the brain responsible for acquiring new motor sequences\behaviors 2. Movement 3. Cognition 4. Regulating prolactin secretion 5. Motivation and pleasure (food, sex, drugs) e. Associated pathologies 1. Parkinson's disease 2. Schizophrenia 3. Psychosis 4. Depression (Slamberova) |
|
|
Serotonin\5-Hydroxytryptamine
a. Function b. Associated disorders c. Serotonin syndrome |
a. Function - Regulation of
1. Anger and aggression 2. Mood 3. Sleep 4. Vomiting 5. Sexuality 6. Appetite b. Associated disorders 1. Psychiatric diseases I. Aggressive and angry behaviors (Increased) II. Depression and bipolar disorder III. Anxiety disorders - OCD 2. 'Peripheral' disorders I. Migraine II. Irritable bowel syndrome (Serotonin is found in gut) III. Tinnitus IV. Fibromyalgia c. Serotonin syndrome I. Toxic and potentially fatal effects of extremely high levels of serotonin (In practice such toxic levels are essentially impossible to reach through an overdose of a single anti-depressant drug) (Slamberova) |
|
|
Parkinson's disease
a. S&S |

a. S&S
TRAP 1. Tremor - Resting 2. Rigidity - Coghweel 3. Akinesia (Lack of movement or slowness in initiating and maintaining movement) 4. Postural instability I. Bending\flexion of body II. Shuffling gait III. Balance problems (Slamberova) |
|
|
Emotion
a. Emotion b. Motivation - What, relation to emotion c. Emotionality d. Emotional maturity |
a. Emotion (Emoveo - To move out\agitate)
I. A strong feeling\aroused mental state\intense state of drive or unrest which may be directed toward a definite object II. Manifested in behavior, psychologic changes, and autonomic responses (Stedman) b. Motivation I. An attempt to avoid or achieve something II. Emotions can be considered the external manifestations of motivations c. Emotionality I. A set of dispositions to emotional reactions II. Associated with temperament (The psychological and biological organization peculiar to the individual, including one's character or personality predispositions, that influence the manner of thought, action, and general views of life) III. Emotionality determines psychological characteristics of personality d. Emotional maturity I. A way to control the processing of expressions and feelings (Rokyta) |
|
|
The limbic system
a. Phylogenesis b. Cortical areas of the limbic system c. The subcortical limbic system components |
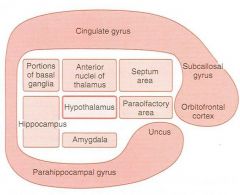
a. The phylogenetically oldest part of the cerebral cortex
(Consist of allocortex with 3 layers and juxtaallocortex with 3-6 layers) b. Cortical areas of the limbic system 1. Insula 2. Frontal cingular cortex 3. Medial part of orbitofrontal cortex of frontal lobe 4. Rhinencephalon - the olfactory brain c. The subcortical limbic system 1. Amygdala 2. Hippocampus 3. Central nuclei 4. Hypothalamus (A separate part of the limbic system) (Rokyta) |
|
|
Hypothalamus - Functions associated with
a. Dorsomedial nucleus b. Posterior hypohalamus c. Perifornical nucleus d. Ventromedial nucleus |
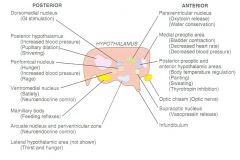
a. Dorsomedial nucleus
I. GI stimulation b. Posterior hypothalamus I. Sympathetic NS -> Increased BP, mydriasis II. Heat-conservation center -> Shivering c. Perifornical nucleus I. Hunger II. Rage (+ Increased BP) d. Ventromedial nucleus I. Satiety (Rokyta) |
|
|
Hypothalamus - Nuclei associated with
a. Food intake - Hunger, Satiety b. Autonomic NS - Sympathetic, parasympathetic c. Temperature regulation - Heat-conservation, heat-loss d. Neurohypophysis hormones - ADH, Oxytocin e. Adenohypophysis neuroendocrine control |
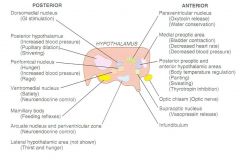
a. Food intake
I. Hunger center -> Perifornical nucleus, Lateral hypothalamic area II. Satiety center -> Ventromedial nucleus (Also thirst) b. Autonomic nervous system I. Sympathetic NS - Posterior hypothalamus (And perifornical ncl) II. Parasympathetic NS - Anterior hypothalamus (Medial preoptic area) c. Temperature regulation I. Heat-conservation center - Posterior hypothalamus (Shivering, vasoconstriction) II. Heat-loss center - Anterior hypothalamic areas (Panting, sweating, thyrotropin inhibition) d. Neurohypophysis hormones I. Vasopressin - Supraoptic ncl (V close to S) II. Oxytocin - Paraventricular ncl (O close P) e. Neuroendocrine control over adenohypophysis - Ventromedial, arcuate nucleus, periventricular (Rokyta) |
|
|
Hypothalamus - Functions associated with
a. Mammillary bodies b. Lateral hypothalamic area c. Medial preoptic area d. Anterior hypothalamic and posterior preoptic areas |
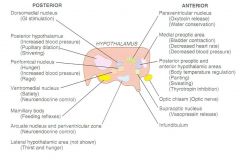
a. Mammillary bodies
I. Feeding reflexes b. Lateral hypothalamic area I. Thirst II. Hunger c. Medial preoptic area I. Parasympathetic I. Bladder contraction d. Anterior hypothalamic and posterior preoptic areas I. Heat-loss: Panting, sweating, thyrotropin inhibition (Rokyta) |
|
|
Nervous system
a. Is UMN lesions or LMN lesions associated with pain perception impairment b. Which spinal cord layers of Rexed corresponds to the terminals of nociceptive primary neurons c. What type of general tone will appear 2-3 weeks after a spinal cord transection |
a. LMN lesions
(Clinical finding - due to proximity in peripheral nerves, cauda equina, and spinal cord) b. Rexed's layer involved in pain transmission 1. I, II-III (Substantia gelatinosa), 2. IV, V, IX - Pain modulation c. Flexor tone (Mechanism not known) (Vacoulin) |
|
|
? |
(Slamberova)
|
|
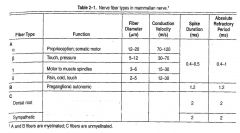
|
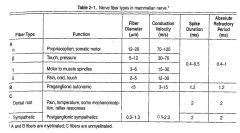
(Slamberova)
|
|
|
Kluver-Bucy syndrome
a. What b. S&S |
a. Syndrome caused by bilateral lesion of amygdala
b. S&S 1. Visual agnosia 2. Increased oral (hyperphagia) and sexual activity 3. Depressed drive and emotional reactions (Stedman, Vacoulin) |
|
|
NS test
a. Which nuclei are involved in sleep induction (REM, and n-REM) b. List the two main descending pain inhibitory pathways, where do they originate from c. Allodynia |
a. Nuclei involved in sleep induction
I. Locus ceruleus and its ascending pathway -> REM induction (Noradrenergic) II. Magnus raphe nucleus and its ascending pathway -> non-REM induction (Serotonergic) b. Descending inhibitory pain pathways 1. Periaqueductal gray matter --Endorphins--> 2a. Nucleus raphe magnus --serotonin--> descending pathway -> dorsal horn of spinal cord 2b. Locus ceruleus --NA--> descending pathway -> dorsal horn of spianl cord c. Allodynia I. Pain elicted from nonpainful stimuli (Vacoulin) |
|
|
Nerve cells
a. Bipolar neurons - Examples b. Myelin - Mechanism of myelinization of nerve fibers c. The four functional zones of neurons |
a. Bipolar neurons
1. Optic 2. Auditory 3. Vestibular 4. Olfactory 5. Cutaneous b. Myelinization I. Schwann in PNS and oligodendrocyte in CNS envelops a axon II. It then wraps its membrane around it up to a 100 times III. Protein zero (P0) interlock apposing parts of the myelin membrane (Defects of P0 cause peripheral neuropathies, > 30 have been described) c. Functional zones of neurons 1. Receptor zone I. Graded electrogenesis - Local potentials are integrated 2. Site where propagated action potentials are generated I. The initial segment of axon in most neurons II. The initial node of Ranvier in cutaneous sensory neurons 3. Axon - All or none transmission 4. Nerve endings - Synaptic transmission (Ganong) |
|
|
Neurons
a. Wallerian degeneration b. Normal resting potential c. Normal threshold\firing level d. Strength-duration curve of initiation of action potentials - What, why |
a. Wallerian degeneration
I. The degeneration of a neuron distal to a cut of the axon b. -70 mV c. 15 mV -> -55 mV d. Strength-duration curve I. Slowly rising currents need a stronger threshold intensity than faster stimuli II. Due to adaptation of the nerve to the applied stimulus in the cases of slowly applied stimuli - accommodation (Ganong) |
|
|
Opioid receptors
a. Type b. Endogenous opioids c. Mu receptors - Location, function d. Delta receptors - Location, function e. Kappa receptors - Location, function |
a. G-protein coupled receptors
b. Endogenous opioids 1. Dynorphins 2. Enkephalins 3. Endorphins 4. Endomorphins c. Mu receptors I. Location 1. Brain - Cortex, thalamus, PAG 2. Spinal cord - SG 3. Peripheral sensory neurons 4. GIT II. Function 1. Mu1 - Analgesia, physical dependence 2. Mu2 - Respiratory depression, miosis, euphoria, reduced GI motility, physical dependence (Named mu since Morphine was the first chemical shown to bind to them, also Mu3 but unknown function) d. Delta receptors I. Location 1. Brain - Pontine nuclei, amygdala, olfactory bulbs 2. Peripheral sensory neurons II. Function 1. Analgesia 2. Physical dependence 3. Antidepressant effects (Named after the mouse vas deferens tissue in which it was first discovered) e. Kappa receptors I. Location 1. Brain - Hypothalamus, PAG, claustrum 2. Spinal cord - SG 3. Peripheral sensory neurons II. Function 1. Analgesia 2. Sedation 3. Miosis 4. Dysphoria (Named after ketocyclazocine) (Also other less known types - nociceptin receptor) (Wiki) |
|
|
Gate theory
a. Devised by b. Principle c. Draw the basic neuronal circuitry d. Applications |
a. Wall and Melzack in 1965
b. Principle I. Pain is a function of the balance between the information traveling into the spinal cord through large nerve fibers and information traveling into the spinal cord through small nerve fibers. If the relative amount of activity is greater in large nerve fibers, there should be little or no pain. If there is more activity in small nerve fibers, then there will be pain. c. Basic neuronal circuitry I. E = Enkephalin-containing inhibiting interneuron II. Thus to feel pain the stimulus in the C fiber must be strong enough to overcome the inhibitory effect of the Abeta on the inhibitory interneuron of lamina II (The inhibitory enkephalinergic neuron may act as a trophic factor to amplify the response of the dendrites to the action of GABA) d. Applications 1. Trans-electrical nerve stimulators 2. Acupuncture (Anesthesiauk.com) |
|
|
Gate theory
a. Devised by b. Principle c. Draw the basic neuronal circuitry d. Applications |
a. Wall and Melzack in 1965
b. Principle I. Pain is a function of the balance between the information traveling into the spinal cord through large nerve fibers and information traveling into the spinal cord through small nerve fibers. If the relative amount of activity is greater in large nerve fibers, there should be little or no pain. If there is more activity in small nerve fibers, then there will be pain. c. Basic neuronal circuitry I. E = Enkephalin-containing inhibiting interneuron II. Thus to feel pain the stimulus in the C fiber must be strong enough to overcome the inhibitory effect of the Abeta on the inhibitory interneuron of lamina II (The inhibitory enkephalinergic neuron may act as a trophic factor to amplify the response of the dendrites to the action of GABA) d. Applications 1. Trans-electrical nerve stimulators 2. Acupuncture (Anesthesiauk.com) |
|
|
Gate theory
a. Devised by b. Principle c. Draw the basic neuronal circuitry d. Applications |
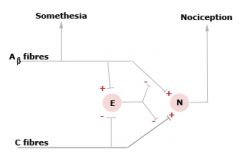
a. Wall and Melzack in 1965
b. Principle I. Pain is a function of the balance between the information traveling into the spinal cord through large nerve fibers and information traveling into the spinal cord through small nerve fibers. If the relative amount of activity is greater in large nerve fibers, there should be little or no pain. If there is more activity in small nerve fibers, then there will be pain. c. Basic neuronal circuitry I. E = Enkephalin-containing inhibiting interneuron II. Thus to feel pain the stimulus in the C fiber must be strong enough to overcome the inhibitory effect of the Abeta on the inhibitory interneuron of lamina II (The inhibitory enkephalinergic neuron may act as a trophic factor to amplify the response of the dendrites to the action of GABA) d. Applications 1. Trans-electrical nerve stimulators 2. Acupuncture (Anesthesiauk.com) |
|
|
Pain pathways
a. The four pathways from the spinal cord b. Dimensions of pain and their anatomical substrate |

a. Pain pathways
1. Spinal cord -> tractus spinoparabrachialis hypothalamicus -> Hypothalamus 2. Spinal cord -> tractus amygdalaris -> Amygdala 3. Spinal cord -> tractus spinoreticulothalamicus -> reticular formation -> Thalamic nuclei - parafascicular nuclei, central lateral nuclei, central medial nuclei -> Cingulate gyrus, insula 4. Spinal cord -> spino\trigeminothalamicus ventrolateralis -> Thalamic nuclei - VPL, VPM -> Postcentral gyrus b. Dimensions of pain 1. Sensory-discriminative I. Where it hurts II. VPL & VPM, postcentral gyrus 2. Motivational-affective aspect I. How it hurts and how unpleasant it is II. Amygdala, cingulate gyrus 3. Cognitive-evaluative aspect I. Consequences (Ie social advantages\disadvantages from being in pain) II. Cortex 4. Executive I. Autonomic response (sweating, heart rate..) II. Hypothalamus (Vacoulin) |
|
|
Evoked potentials
a. What b. Types c. Applications |
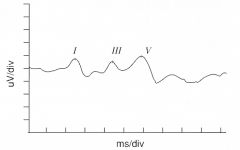
a. Evoked potentials
I. Electrical potential recorded using EEG following presentation of a stimulus II. Use mV b. Types I. Brainstem auditory evoked potential (BAEP) - Auditory stimulus II. Visual evoked potential (VEP) - Checkerboard pattern III. Somatosensory evoked potential (SSEP) - Electrical stimulus c. Applications 1. BAEP - MS, neuroma of acoustic nerve, audiometry in children 2. VEP - Eye movement disorders, nerve dysfunction, cortical blindness 3. SSEP - Spinal cord function during\after surgery (Stimulate peripheral nerve) (Example is BAEP. Wave 1 is a manifestation of the AP of CN VIII in the distal portion adjacent to the cochlea, wave II is generated by CN VIII or cochlear nuclei, wave III is generated at superior olive, wave IV and V are generated in rostral pons or in the midbrain near the inferior colliculus) (Vacoulin) |
|
|
The limbic system
a. Emotion - Components b. Motivation - the two subdivisions and their difference c. Example of drives |
a. Emotion - Combination of
1. Cognition 2. Affect (Reward\satisfaction vs punishment\aversion) 3. Conation (How one act on thoughts and feelings) 4. Physical changes (Autonomic) b. Drives vs instincts I. Instincts - Genetically fixed II. Drive - Genetically fixed, but modifiable according to experience c. Drives I. Vegetative drive - Hunger, thirst II. Defensive drive - Fear, rage III. Reproductive drive - Sex, parental care IV. Educational drive - Exploration, searching V. Social motivation - To belong in some group (Instinct - Enduring disposition\tendency to act in an organized and biologically adaptive manner characteristic of its species) (Vacoulin) |
|
|
The limbic system
a. The two main functional structures b. Papez (1973) circle - Components c. Papez circle - afferents and efferents |
a. Hippocampus and amygdala
b. Papez circle I. Hippocampus -> II. Mammillary bodies -> III. Anterior nucleus of thalamus -> IV. Cingulate gyrus -> I. c. Papez circle I. Afferents 1. Association cortices 2. Cingulate gyrus II. Efferents 1. Association cortices 2. Mesencephalic reticular formation (Vacoulin) |
|
|
The limbic system
a. Effect of stimulating amygdala or hippocampus b. Effect of ablation of hippocampus c. Effect of ablation of amygdala |
a. Effect of stimulating hippocampus or amygdala
I. Via hypothalamus - Changes in BP, pulse, GIT motility, defecation and micturition, piloerection, ACTH and gonadotropin secretion II. Epileptoid seizures (III. Non-conscious movements (only amygdala)) c. Stops declarative learning and memory - no consolidation d. Kluver-Bucy syndrome I. Hypersexuality, oral examination of objects, loss of fear, decrease of aggressiveness, tameness (Observed in apes) (Vacoulin) |
|
|
Lability and parabiosis
a. Lability b. Parabiosis |
a. Lability
I. Maximal frequency of stimulation to which a neuron is able to respond II. Inversely proportional to chronaxy (Chronaxie - A measurement of excitability of nervous or muscular tissue. The shortest duration of an effective electrical stimulus having a strength equal to twice the minimum strength required for excitation) b. Parabiosis I. Axonal state during altering conditions (Ie heat, cold, chemicals) II. The nerve responds in 3 steps 1. Provisory phase - Excitability is lower 2. Paradoxical phase - Nerve is excitable but only by a low intensity stimulus 3. Inhibition phase - Nerve is inhibited by stimulation of parabiotic part (Vvedenskij, almost unknown in Anglo-saxon physiology) (Vacoulin) |
|
|
Electrophysiological manifestations of memory
a. Post-tetanic potentiation b. Habituation c. Sensitization d. Long-term potentiation e. Long-term depression |
a. Post-tetanic potentiation
I. 60s II. Tetanic stimulation cause an accumulation of Ca in presynaptic neuron b. Habituation I. Gradually diminshed response to repeated benign stimulus II. Due to inactivation of Ca channels c. Sensitization I. Increased response to repeated stimulus II. Due to serotonin-mediated presynaptic facilitation of sensory neuron-endings via slowing the repolarization (rapid closing of K-channels) of presynaptic membrane and prolonging the AP d. Long-term potentiation I. Similar to post-tetanic stimulation, but lasts for days (Well known in hippocampus) II. Ca accumulation in post-synaptic neuron III. Mechanism 1. Depolarization of postsynaptic membrane via AMPA receptor activation relieves the Mg block of NMDA receptor -> allows Ca to enter the neuron 2. Unknown cascade cause long-term enhancement of AMPA receptors (AMPA and NMDA receptors is glutamate subtype receptors) e. Long-term depression I. Happens under partial depolarization of postsynaptic neuron II. Up to -20 mV III. Physiological role unknown (Vacoulin) |
|
|
Biphasic action potential
a. Caused by b. Mechanism |
a. Biphasic action potential
I. Seen when a nerve is stimulated and two electrodes are connected to the surface of the axon, one after the other b. Mechanism 1. As the wave of depolarization reaches the first electrode, this becomes negative relative to the other (Its normal to connect the leads in such a way that this is shown as an upward deflection) 2. When the impulse passes to the portion of the nerve between the two electrodes, the potential returns to zero - isoelectric interval 3. When the action potential passes the second electrode, the first electrode becomes positive relative to the second (Normally shown as a downward deflection) (If one electrode is placed in the cell and one outside it will be detected as a monophasic action potential) (Ganong) |
|
|
Ions and electric properties of cells
a. Na - Effect of decreasing the external concentration on the size of the action potential and the resting membrane potential b. K - Effect of decreasing the external concentration on the size of the action potential and the resting membrane potential c. Ca - Effect of decreasing its external concentration on excitability |
a. Hyponatremia
I. Decrease the size of the action potential II. Little effect on resting membrane potential (Little Na flux during resting state) b. Hypokalemia I. Increase size of action potential II. Decrease resting potential c. Hypocalcemia I. Increase excitability (Think of Ca and Mg as being attracted to cation channels first due to their stronger positive charge but not being able to pass through, and blocking the channels for Na and K) (An increase in extracellular Ca concentration stabilize the membrane by decreasing excitability) (Ganong) |
|
|
Relative susceptibility of mammalian A, B, and C nerve fibers to conduction block produced by various agents. List from most to least susceptible
a. Hypoxia b. Pressure c. Local anesthetics |
a. Hypoxia - B,A,C
(A,B, C but B and A is changed) b. Pressure - A,B,C (Depend on size and activity. Thus pressure can affect A fibers selectively at first, this is often seen in Saturday night palsy) c. Local anesthetics - C,B,A (Inversely related to myelinzation) (Ganong) |
|
|
Neurotrophins
a. Neurotrophin b. Examples c. Receptors d. Other factors affecting neuronal growth |
a. Neurotrophin
I. Proteins necessary for survival and growth of neurons (Some are produced by other cells (ie astrocytes, myocytes, bind to receptors on neurons, get internalized, and then get transported by retrograde transport to the cell body where they affect proteosynthesis. Others are produced by neurons, transported anterograde and then function to maintain the integrity of the postsynaptic neuron) b. Examples I. Nerve growth factor (NGF) (trk A, its active beta subunit is very homologous to insulin, transported retrograde, especially associated with sympathetic neurons) II. Brain-derived neurotrophic factor (BDNF) (trk B) III. Neurotrophin 3 (NT-3) c. Receptors I. trk A,B,C (Tyrosinase kinase receptors, as insulin) II. Dimerize and autophosphorylate each other d. Other factors affecting neuronal growth 1. Ciliary neurotropic factor (CNTF) (<- Schwann cells and astrocytes, assumed to promote survival of embryonic spinal cord neurons) 2. Glial cell line-derived neurotropic factor (GDNF) 3. Leukemia inhibitory factory (LIF) (Enhance growth of neurons) 4. Non-specific growth factors - IGF-1, TGF, FGF, PDGF (Ganong) |
|
|
Astrocytes
a. Types and their characteristics b. Function |
a. Astrocytes
1. Fibrous astrocytes I. ↑White matter II. ↑Intermediate filaments 2. Protoplasmic astrocytes I. ↑Gray matter II. Granular cytoplasm b. Function 1. Send processes to blood vessels where they induce capillaries to form the tight junctions that form the BBB 2. Send processes that envelop synapses 3. Produce substances that are tropic to neurons I. Ciliary neurotropic factor (CNTF) (For embryonic spinal cord neurons) 4. Help maintain the appropriate extracellular concentration of ions and neurotransmitters I. Take up K (K levels is determinant of resting membrane potential) II. Take up GABA and glutamate (Glu released into synaptic cleft is taken up by Glu-3Na symporter, transformed to Gln and released, Gln is then taken up by presynaptic neuron and reused after it has been transformed to Glu) (Ganong) |
|
|
Synapses
a. Terminal bouton\synaptic knob b. Anatomical types of synapses c. Average synaptic endings per neuron d. Width of synaptic cleft e. Proteins involved in the fusion of synaptic vesicles to the cell membrane of the presynaptic neuron, clinical application |
a. Terminal bouton\synaptic knob
I. The enlarged end of a presynaptic fiber that participate in the synapse b. Anatomical types of synapses 1. Axodendritic I. On shaft of dendrite II. On spine of dendrite (1.II. is most frequent in cortex and cerebellum, 98% of synapses in the cortex is axodendritic) (Climbing fibers of the cerebellum intertwine with the dendrites of the Purkinje cells) 2. Axosomatic synapses (More frequent in spine (20% vs 2% in cortex) (Basket cells of cerebellum form a basket\net around the soma of the postsynaptic cell) 3. Axoaxonic c. 2 000 (100 billion x 2 000 = 2 x 10^14) d. 20-40 nm e. Proteins - These 2 interlock 1. Synaptic vesicle - Synaptobrevin I. V-snare type protein II. Tetanus toxin and botulinum toxin B,D,F, and G act on it 2. Cell membrane - Syntaxin I. T-snare type protein II. Botulinum toxin C act on it (The toxins are zinc endopeptidases and they block neurotransmitter release. Tetanus toxin cause spastic paralysis by blocking by acting in CNS, botulinum toxin cause flaccid paralysis by acting on the neuromuscular junction. Botulinum toxin is used to treat conditions characterized by muscle hyperactivity, achalasia, wrinkles..) (Ganong) |
|
|
Neurons
a. Distribution of organelles b. Types of synaptic vesicles c. Differences between small and large synaptic vesicles d. Which proteins maintains the structural integrity of the synapses |
a. Distribution of organelles
I. All the organelles except the proteosynthetic apparatus are distributed over the entire neuron. II. The proteosynthetic apparatus is not present in the axon and its distal part b. Types of synaptic vesicles 1. Small clear synaptic vesicles I. Ach, Gly, GABA, Glu (All except neuropeptides and catecholamines) 2. Small vesicles with a dense core I. Catecholamines 3. Large vesicles with a dense core I. Neuropeptides (Largest molecules, largest vesicles) c. Differences between small and large synaptic vesicles 1. Recycling of neurotransmitters I. S: Yes II. L: No 2. Discharge mainly into active zones or more diffuse I. S: Active zones II. L: Diffuse (The active zones contain many proteins and calcium channels) d. Neurexins (Neurexins on the pre- and postsynaptic membranes bind) (Ganong) |
|
|
Synaptic transmission
a. Synaptic delay b. IPSPs and EPSPs - Peak time, time constant ('duration') c. How can IPSPs be produced d. Slow postsynaptic potentials |
a. 0.5 ms
b. 1-1.5 ms, 3 ms c. IPSP production 1. Opening of Cl channels 2. Opening of K channels 3. Closing of Na or Ca channels d. Slow postsynaptic potentials I. Time constant of several seconds and latency of > 100 ms (Time constant can be up to 30 min in sympathetic ganglia) II. Autonomic ganglia, cardiac and smooth muscle, cortical neurons III. Mainly by regulating K conductance (Ganong) |
|
|
Synaptic transmission
a. Postsynaptic direct and indirect inhibition b. Presynaptic inhibition c. Presynaptic facilitation d. Renshaw cell |
a. Postsynaptic direct and indirect inhibition
I. Direct - Not a consequence of previous discharges of the postsynaptic neuron, IPSP II. Indirect - Consequence of previous discharges of the postsynaptic neuron - Refractory period, after-hyperpolarization b. Presynaptic inhibition I. Axoaxonal synapses II. Increase K or Cl conductance, direct inhibition of transmitter release independent of Ca influx III. GABA (Baclofen is a GABA-B agonist that is used in treating the spasticity of spinal cord injury and MS) c. Presynaptic facilitation I. Produced when the AP is prolonged and the Ca channels are open for a longer period (In the snail Aplysia it is mediated by serotonin. Serotonin is released at an axoaxonal ending -> ↑cAMP -> close K channels by phosphorylation -> Slow repolarization -> Prolong AP) d. Renshaw cell I. Inhibitory interneuron II. Innervated by recurrent collateral of motor neuron, terminate on the cell body of the spinal neuron and other spinal motor neuron III. Example of negative feedback inhibition (Similar mechanisms is seen in the cerebral cortex and limbic system) (Ganong) |
|
|
Catabolism of catecholamines
a. What are the 4 ways norepinephrine is removed from the synaptic cleft b. How are epinephrine and norepinephrine catabolized c. What is the most numerous metabolite in the urine |
a. Removal of norepinephrine from the synaptic cleft
1. Binding to postsynaptic receptors 2. Binding to presynaptic receptors 3. Reuptake into presynaptic neurons 4. Catabolism b. Catabolism of epinephrine and norepinephrine 1. Oxidative deamination by monoamine oxidase I. On the outer surface of the mitochondria II. MAO A and B, both are found in neurons and are plentiful in the nerve endings in which they are secreted 2. Methylated by catecholamine-O-methyltransferase (COMT) I. In liver, kidneys, smooth muscle, glial cells, small amounts in postsynaptic neurons II. Main extracellular route III. O-methylated derivatives - Normetanephrine\3-methoxynorepinephrine), metanephrine (3-methoxyepinephrine) (Excreted in the urine or further metabolized (oxidized, conjugated) c. Vanillylmandelic acid (VMA)\3-methoxy-4-hydroxymandelic acid (After COMT+MAO) (Ganong) |
|
|
Serotonin
a. Location b. Synthesis c. Catabolism d. Receptors |
a. Location
1. Thrombocytes 2. GIT - Enterochromaffin cells, the myenteric plexus 3. Brain 4. Retina b. Synthesis 1. Tryptophan hydroxylase I. Tryptophan -> 5-hydroxytryptophan II. Tetrahydrobiopterin 2. 5-hydroxytryptophan decarboxylase I. 5-hydroxytryptophan -> Serotonin (-> Can continue in melatonin pathway) c. Catabolism I. Most is captured by active reuptake then oxidized by MAO to 5-hydroxyindoleacetic acid (5-HIAA) which is the principal urinary metabolite d. Receptors 1. 5-HT1 2. 5-HT2 (5-HT2A mediate platelet aggregation and smooth muscle contraction) 3. 5-HT3 (Linked to ion channels, all others are Gs or Gq, present in area postrema and the GIT and linked to vomiting) 4. 5-HT4 (Facilitate secretion and peristalsis in the GIT) 5. 5-HT5 6. 5-HT6 (Limbic system, high affinity for antidepressant drugs) 7. 5-HT7 (Ganong) |
|
|
Histamine
a. Location b. Synthesis c. Catabolism d. Receptors |
a. Location
1. Tuberomammillary nucleus of the posterior hypothalamus (Project to all parts of the cortex and spinal cord) 2. Cells in the gastric mucosa 3. Mast cells b. Synthesis 1. Histidine decarboxylase I. Histidine -> histamine c. Catabolism I. Primarily by histamine-N-methyltransferase to methylhistamine d. Receptors - All are found in both brain and peripheral tissue 1. H1 (Gq) 2. H2 (Gs) 3. H3 (Presynaptic) (Related to arousal, sexual behavior, regulation of the secretion of some anterior pituitary hormones, blood pressure, drinking, pain threshold) (Ganong) |
|
|
Glutamate
a. Responsible for .... of the excitatory transmission in the brain b. Synthesis c. Receptors d. NMDA receptors - Type, unique characteristics |
a. 75%
b. Synthesis I. Reductive deamination of alpha-ketoglutarate from the Krebs cycle II. Concentrated in synaptic vesicles by BPN1 (Taken up by 3 transporters that import glutamate from the interstitial fluid) c. Receptors 1. Metabotropic receptors I. G-protein coupled, Gs or Gi II. 11 subtypes (Widely distributed, involved in synaptic plasticity, particularly in the hippocampus and cerebellum) 2. Ionotropic receptors - 3 types I. Kainate receptors (Kainate is an acid isolated from seaweed, simple channel that permit Na influx and K efflux) II. AMPA receptors (2 types - simple Na and one that also passes Ca, kainate and AMP receptors are found in glia as well) III. NMDA receptors (N-methyl-D-aspartate, high concentration in hippocampus, blockade prevent long-term potentiation) d. NMDA receptors I. Cation channel that also permit passage of relatively large amounts of Ca II. Unique properties 1. Glycine facilitates its function by binding to it (Appears to be essential for its normal response to glutamate) 2. When glutamate binds to it, it opens, but at normal membrane potentials, its channel is blocked by an Mg ion. This block is removed only when the neuron is partially depolarized by activation of AMPA (Phencyclidine and ketamine, which produce amnesia and a feeling of dissociation from the environment, bind to another site inside the channel) (Ganong) |
|
|
Glutamate
a. Mechanism of its excitotoxic effect b. Association with stroke |
a. Produce so much Ca influx that neurons die
(Used in research to produce discrete lesions) b. Association with stroke I. Glutamate is usually cleared from the brain ECF by Na-dependent uptake systems in the neurons and glia II. Partially ischemic cells in the pneumbra (the region around the completely infarcted area) lose tehir ability to maintain the transmembrane Na gradient that drives the glutamate uptake -> Glutamate accumulation (Ganong) |
|
|
Gamma-aminobutyric acid (GABA)
a. Location b. Synthesis c. Catabolism d. Receptors e. Clinical applications |
a. Location
1. Brain (Major inhibitory mediator in the brain, 20% of CNS synapses, responsible for presynaptic inhibition) 2. Retina b. Synthesis 1. Glutamate decarboxylase (GAD) I. Glutamate -> GABA II. Pyridoxal phosphate (Autoimmunity to GAD cause the stiffman syndrome (SMS), a disease characterized by fluctuating but progressive muscle rigidity and painful muscle spasms, presumably due to GABA deficiency) 2. Vesicular GABA transporter (VGAT) I. Transports GABA and Glycine into secretory vesicles (Also get GABA by active reuptake) c. Catabolism 1. GABA transaminase (GABA-T) I. GABA -> Succinic semialdehyde (-> succinate) II. Pyridoxal phosphate d. Receptors 1. GABA-A I. Widely distributed in the CNS II. Ion channel for Cl III. Pentamer 2. GABA-B I. Widely distributed in the CNS I. Metabotropic - Gi, increase K conductance, inhibit Ca influx 3. GABA-C I. Retina II. Ion channel for Cl e. Clinical application 1. Barbiturates bind to the alpha subunit of GABA-A and potentiate them (Diazepam.., antianxiety, muscle relaxants, anticonvulsants, sedatives) 2. At least in part, barbiturates, volatile anesthetics, and alcohol also act by facilitating Cl conductance through the GABA-A (Also have similar function on Glycine receptors, some evidence that they inhibit NMDA and AMP receptors) 3. Metabolites of progesterone and deoxycorticosterone bind to GABA-A receptors and increase Cl conductance (Explain their sleep-inducing effect) (Ganong) |
|
|
Glycine
a. Function b. Mechanism |
a. Function
1. When it binds to NMDA receptors, it makes them more sensitive (Pain transmission in spinal cord?) 2. Direct inhibition - primarily in brain stem and spinal cord b. Mechanism I. Ionotropic - increase Cl conductance (Antagonized by strychnine which cause convulsions) (Ganong) |
|
|
Substance P
a. Location b. Belong to which group c. Receptors d. Clinical application |
a. Location
1. Intestine 2. Various peripheral nerves - Found in high concentrations in the endings of primary afferent neurons in the spinal cord (Probably the mediator at the first synapse in the pathways for slow pain) 3. Many parts of CNS I. Nigrostriatal system II. Hypothalamus b. Tachykinins I. 6 mammalian polypeptides that have a common carboxy terminal sequence II. Members 1. Substance P\Neurokinin 1 2. Neurokinin A 3. Neuropeptide K 4. Neurokinin B (5\6 is formed by substance P\neurokinin A gene, the last is formed by NKB gene) b. Receptor - Substance P\NK1 receptor I. Gq d. Clinical application 1. NK-1 receptor antagonist have antidepressant, antiemetic, and anxiolytic properties I. Ie aprepitant II. Used as antiemetic agent for chemotherapy (Ganong) |
|
|
Opioid peptides
a. Opioid peptides b. Members and their precursor c. Catabolism d. Receptors and their function |
a. Opioid peptides
I. Peptides that bind to opioid receptors b. Members 1. Proenkephalin -> I. Met-enkephalin (Tyr-Gly-Gly-Phe-Met) II. Leu-enkephalin (Tyr-Gly-Gly-Phe-Leu) (+ Octapeptide, heptapeptide) 2. Pro-opiomelanocortin I. Beta-endorphin (Found in anterior and intermediate lobe of pituitary gland and the brain) 3. Prodynorphin I. Alpha-neoendorphin II. Beta-neoendorphin (Neoendorphins in hypothalamus) III. Dynorphin 1-8 (Posterior pituitary, hypothalamus) IV. Dynorphin 1-17 (Duodenum) (More than 20 active opioid peptides have been identified) c. Catabolism 1. Enkephalinase A - Split Gly-Phe 2. Enkephalinase B - Split Gly-Gly 3. Aminopeptidase - Split Tyr-Gly (Ganong) |
|
|
Opioid peptides
a. Type of receptors b. Mu receptor - Effect, function c. Kappa receptor - Effect, function d. Delta receptor - Effect, function |
a. Serpentine receptors coupled to Gq and inhibit adenylyl cyclase
b. Mu receptors I. Increase K conductance -> hyperolarization II. Main site of action of morphine III. Function 1. Analgesia 2. Respiratory depression 3. constipation 4. Euphoria 5. Sedation 6. Increased secretion of GH and PRL 7. Miosis (In mice in which the mu receptors have been knocked out, morphine fails to produce analgesia and withdrawal symptoms. Selective blockade of the other receptors fail to produce this blockade) c. Kappa receptor I. Close Ca channels II. Function - Analgesia, diuresis, sedation, miosis, dysphoria d. Delta receptors I. Close Ca channels II. Function - analgesia (Ganong) |
|
|
Somatostatin
a. Types b. Functions c. receptors |
a. Preprosomatostatin -> somatostatin 14, somatostatin 28
b. Functions 1. Neurotransmitter in brain 2. GHIH in hypothalamus 3. Inhibit secretion of pancreatic hormones in the islets of Langerhans (Somatostatin 28 is most active in inhibiting insulin secretion) 4. Inhibitory GI hormone c. Receptors I. 5 - SSTR1-5 (SSTR2 - Cognitive effects and inhibition of GH secretion, SSTR5 - inhibition of insulin secretion) II. G protein-coupled - Gi (Ganong) |
|
|
Purine and pyrimidine transmitters
a. Where does ATP in the ECF of the CNS originate from b. Adenosine - Receptors, clinical application c. Other purine and pyrimidines which function as transmitters |
a. Its the ATP released with monoamines and acetylcholine
b. Adenosine I. 4 receptors 1. 2Gs - A2A, A2B 2. 2Gi - A1, A3 II. The stimulatory effects of tea and coffee appear to be due to blockade of adenosine receptors (Adenosine is a vasodilator in the heart) c. 1. ATP (Receptors - P2Y, P2U, P2X, P2Z) 2. ADP 3. Uridine (Ganong) |
|
|
Cannabinoids
a. What are the two receptors with high affinity for delta9-tetrahydrocannabinol (THC), the psychoactive ingredient in marijuana b. What is the endogenous ligands of these receptors |
a. CB1, CB2
b. CB1 - Anandamide I. Derivative of arachidonic acid (-> Euphoria, calmness, dream states, drowsiness and analgesia, peripheral receptors cause vasodilation) 2. CB2 - May be palmitoylethanolamide (PEA) (The physiological role is uncertain) (Ganong) |
|
|
Cotransmitters
a. Cotransmitters of serotonin in the brainstem b. Cotransmitters of many cholinergic neurons c. Cotransmitters of many noradrenergic and adrenergic neurons |
a. Cotransmitters of serotonin in the brainstem
1. Serotonin 2. Substance P 3. TRH b. Cotransmitters of many cholinergic neurons 1. Acetylcholine 2. VIP c. Cotransmitters of many adrenergic and noradrenergic neurons 1. ATP 2. Neuropeptide Y (Ganong) |
|
|
Nerve endings in smooth and cardiac muscle
a. Characteristics of the end plates (postsynaptic part) of smooth muscle b. From which structure is the neurotransmitter released from noradrenergic and cholinergic neurons |
a. No recognizable end plates
b. Varicosities I. Enlarged that are not covered by Schwann cells and contain synaptic vesicles (Up to 20 000 varicosities per noradrenergic neuron) (This type of contact in which a neuron forms a synapse on the surface of a smooth muscle cell or neuron and then passes onto make similar contacts with other cells is called a synapse en passant) (The same type are found in ventricular muscle, the exact nature of the nodal endings (SA, AV; bundle of His) is unclear) (Ganong) |
|
|
Denervation
a. Effects of denervation |
a. Effects of denervation
1. Hypersensitivity of the postsynaptic structure to the transmitter previously secreted by the axon endings (Synthesis or activation of more receptors, lack of reuptake of neurotransmitters (ie ) 2. Wallerian degeneration - Orthograde 3. Retrograde degeneration (To the nearest collateral - sustaining collateral) 4. Chromatolysis - Decrease in Nissl body 5. Regenerative sprouting (Strengthened by administration of neurotrpins - NGF, neurotropin 3, GDNF) (Ganong) |
|
|
Sense organs
a. Classification |
a. Classification - 2 ways
1. Traditional I. Special senses - Taste, hearing, smell, vision, rotational and linear acceleration II. Cutaneous senses - Those with receptors in the skin III. Visceral senses - Those concerned with perception of the internal environment 2. Other I. Teleceptors - Concerned with events at distance II. Exteroceptors - Concerned with the external environment near the hand III. Interoceptors - Concerned with the internal environment IV. Proprioceptors - Provide information about the position of the body in space (Ganong) |
|
|
Sensory modalities - List the receptor and sense organ for
a. Muscle length b. Muscle tension c. Temperature of blood in head d. Arterial PO2 e. pH of CSF f. Osmotic pressure of plasma g. Arteriovenous blood glucose difference |
a. Muscle length
I. Nerve endings II. Muscle spindle b. Muscle tension I. Nerve endings II. Golgi tendon organs c. Temperature of blood in head I. Neurons in hypothalamus d. Arterial PO2 I. Glomus cells II. Carotid and aortic bodies e. pH of CSF I. Receptors on ventral surface of medulla oblongata f. Osmotic pressure of plasma I. Cells in OVLT (And possibly other circumventricular organs in anterior hypothalamus) g. Arteriovenosu blood glucose difference I. Cells in hypothalamus (Glucostats) (Ganong) |
|
|
Graded potentials - Terminology
a. In CNS neurons b. In receptors c. Skeletal muscle d. Smooth muscle |
a. EPSP and IPSP
b. Receptor potential\generator potential c. End plate potential d. Excitatory junction potentials (EJPs) and IJPs (Ganong) |
|
|
Sensory physiology
a. Doctrine of specific nerve energies b. The law of projection |
a. Doctrine of specific nerve energies
I. If a nerve pathway from a particular sense organ is stimulated, the sensation evoked is that for which the receptor is specialized no matter how or where along the pathway activity is initiated. (Muller 1835, ie tumor pressing on pathway in spinal cord evoke same sensation) b. The law of projection I. No matter where a particular sensory pathway is stimulated along its course to the cortex, the conscious sensation produced is referred to the location of the receptor. (Ie pain and proprioceptive sensations in amputated leg - phantom limb. the ends of the nerves cut at the time of amputation often form nerve tangles called neuromas. These may discharge spontaneously or when pressure is put on them.) (Ganong) |
|
|
Pain
a. Lewis's P factor b. Guarding c. Dermatomal rule d. Cause of referred pain |
a. Lewis's P factor
I. Nociceptie agent released during muscle contraction when perfusion is inadequate II. Maybe K III. Ie Angina pectoris, Intermittent claudication, occlusive vascular disease b. Guarding I. Pain - somatic or visceral -> Reflex contraction of nearby skeletal muscles II. Peritoneum is especially sensitive for abdominal muscles c. Dermatomal rule I. The phenomenon that when pain is referred, it usually goes to a structure that developed from the same embryonic segment or dermatome as the structure in which the pain originates. d. Cause of referred pain I. Plasticity in CNS II. Convergence of peripheral and visceral pain fibers on the same second-order neurons that project to the brain (Lamina I-VI of ipsilateral dorsal horn) (Lamina VII receive afferents from both sides of the body - a requirement if convergence is to explain referral to the side opposite that of the source of pain) (Ganong) |
|
|
Pain innervation - GIT
a. Pharynx b. Hypopharynx -> Lower 2\3 of trachea c. Stomach d. Liver and gallbladder e. Small intestine f. Colon g. Sigmoid colon and rectum |
a. Pharynx - CN IX, X
(Parasympathetic) b. Hypopharynx -> Lower 2\3 of trachea - CN X (Parasympathetic) c. Stomach I. Splanchnic nerves -> T7-T9 (Sympathetic) d. Liver and gallbladder I. Right splanchnic nerves -> T7-T9 e. Small intestine I. Splanchnic nerves -> T9-T11 f. Colon I. T11-L1 g. Sigmoid colon, rectum I. Parasympathetic rami -> S2-S4 (Ganong) |
|
|
Inflammatory pain
a. What b. Characteristics of the pain c. Mechanism |
a. Inflammatory pain
I. Pain brought on by inflammation - after anything more than a minor injury, inflammatory pain sets in and persists until the injury heals b. Characteristics of the pain I. Hyperalgesia II. Allodynia c. Mechanism I. Inflammation -> Release of many different cytokines and growth factors II. Many of these facilitate perception and transmission in cutaneous areas as well as in the dorsal horn (Ganong) |
|
|
Neuropathic pain
a. Causalgia b. Possible mechanism |
a. Causalgia (Kausis - burning)
I. Persistent severe burning pain, usually following injury of a peripheral (Injury can be trivial) (Especially median, tibial, and brachial plexus nerves) II. Often accompanied by allodynia and hyperalgesia b. Possible mechanism - Reflex sympathetic dystrophy I. Nerve injury -> Sprouting and overgrowth of noradrenergic sympathetic nerve fibers into the dorsal root ganglia of the sensory nerves from the injured area II. Sympathetic discharge then brings on the pain (Skin in the affected area is thin and shiny, and there is increased hair growth) (This type of pain can be relieved by alpha-adrenergic antagonist, (phentolamine). Alpha-1-adrenegic blockers (prazosin) are more effective than alpha-2-adrenergic blockers (idozoxan) (Ganong) |
|
|
Pharmacological analgesic agents
a. Morphine and endorphins b. Acetylcholine c. Cannabinoids d. Others |
a. Morphine and endorphins
1. Peripheral receptors at site of an injury (Inflammation cause the production of opioid peptides by immune cells, and these presumably act on the receptors in the afferent nerve fibers to reduce the pain) 2. Opioid receptors in dorsal horn (Presynaptically to decrease release of substance P as one possible mechanism) 3. Periaqueductal gray matter (Injection of morphine relieve pain by activating descending pathways that produce inhibition of primary afferent transmission in the dorsal horn. Mostly indirectly via serotonin from raphe magnus) b. Acetylcholine I. Epibatidine, a cholinergic agonist exert analgesia by a mechanism other than activation of opiate receptors or COX inhibition (Extract from poisonous South American frog) II. The effects are blocked by cholinergic blocking drugs) c. Cannabinoids I. Anantamide and PEA are produced endougenously and bind to CB1 and CB2 receptors, respectively II. Anandamide-containing neurons in the periaqueductal gray and other areas concerned with pain, shown to have analgesic effect III. PEA acts peripherally to augment the analgesic effect of anandamide d. Others 1. Capsaicin I. Depletes Substance P from sensory nerve endings II. Found in chili III. Sometimes used for postherpetic neuralgia 2. Alpha-adrenergic antagonists for causalgia 3. Substance P antagonist - Aprepitant (Ganong) |
|
|
Taste and smell
a. Abnormalities of taste b. Drugs which can cause temporary loss of taste sensation c. Organ responsible for detection of pheromones, present in humans d. G-protein associated with many of the sweet and bitter taste receptors e. Role of Ebner's gland in relation to taste |
a. Ageusia, hypogeusia, dysgeusia
b. Captopril, penicillamine (Drugs that contain sulfhydryl groups) c. Vomeronasal organ I. Present in humans but in a rudimentary form - homolog II. Distinct molecular and anatomical spot in a pit on the anterior 1\3 of the nasal septum d. alpha-Gusducin e. Ebner's gland I. Produce mucus which dissolve molecules and allow them to come in contact with the taste pore II. Secrete protein similar to odorant-binding protein (ODP) in olfactory mucosa, which bind lipophilic chemicals and facilitate their contact through the hydrophilic mucus to the taste receptor (Ganong) |
|
|
Evoked potential
a. What b. Parts and their cause\mechanism |
a. The electrical events that occur in the after stimulation of a sense organ
b. Evoked potential 1. Primary evoked potential I. First positive then negative wave sequence, when recorded from surface of cortex II. Highly specific in its location, can be observed only where the pathways from a particular sense organ end (From depolarization-hyperpolarization\Layer 1 is first positive in relation to the deeper hyperpolarized layers, then negative when it is hyperpolarized in relation to the deeper layers) 2. Diffuse secondary response I. Not highly localized - Appears at the same time over most of the cortex II. Due to activity in projections from the midline and related thalamic nuclei (The primary evoked potential is largely obscured by spontaneous activity of the brain. In experimental animals, this background activity can be reduced by barbiturate-anesthesia) (Ganong) |
|
|
EEG
a. Bipolar and unipolar EEG recording b. Rhythms - Which, characteristics c. Frequency decreased by, increased by |
a. Bipolar and unipolar EEG recording
1. Unipolar I. Show potential differences between a cortical electrode and a theoretically indifferent electrode on some part of the body distant from the cortex 2. Bipolar I. Show fluctuations in potential between two cortical electrodes b. Rhythms 1. Gamma oscillations I. 30-80 Hz II. When an individual is aroused and focuses attention on something 2. Beta rhythm I. 18-30 Hz, lower amplitude than alpha II. Sometimes seen over frontal regions 3. Alpha rhythm I. 8-12 Hz, 50-100 uV II. Adult humans who are awake but at rest with eyes closed III. Most prominent at parieto-occipital area 4. Theta rhythm I. 4-7 Hz, large amplitude II. Children 5. Delta waves I. < 4 Hz, Large waves c. Determinants of frequency 1. + I. Hypoglycemia II. Hypothermia III. Hypercapnia IV. Low level of adrenal glucocorticoids 2. - I. Opposite of 1 (Forced hyperventilation to lower the PaCO2 is sometimes used clinically to bring out latent EEG abnormalities) (Ganong) |
|
|
EEG
a. Alpha block b. REM sleep - Muscle activity c. REM sleep - PGO spikes |
a. Alpha block
I. When attention is focused on something, the basal alpha rhythm is replaced by beta waves, also produced by any form of sensory stimulation II. Alpha block\Arousal or alerting response b. REM sleep - Muscle activity I. Paralysis of voluntary activity, mediated by locus ceruleus II. Involuntary REMs however (In cats with locus ceruleus lesions, REM sleep is associated with thrashing about, as if they were acting out their dreams) c. REM sleep - Ponto-geniculo-occipital (PGO) spikes I. Large phasic potentials, in groups of 3-5 II. Originate in the pons -> lateral geniculate body -> occipital cortex (Ganong) |
|
|
Sleep
a. The 3 subcortical regions that can produce slow-wave sleep when stimulated b. Role of serotonergic neurons c. Combined role of serotonergic and noradrenergic brainstem neurons on sleep d. Role of adenosine |
a. The 3 subcortical regions that can produce slow-wave sleep when stimulated
1. The diencephalic sleep zone I. Posterior hypothalamus, anterior and intralmainar thalamic nuclei 2. Medullary synchronizing zone I. In RF of medulla oblongata at the level of the nucleus of tractus solitarius 3. Basal forebrain sleep zone I. Preoptic area and diagonal band of Broca (1 and 2 cause sleep when stimulated at low frequency and arousal when stimulated at high frequency, 3 cause sleep when stimulated regardless of frequency) b. Serotonergic system I. Appears that serotonin agonist suppress sleep and that serotonin antagonist such as ritanserin increase slow-wave sleep c. NA and 5-HT I. Locus ceruleus and serotonergic neurons in the midbrain raphe contribute to wakefulness II. These neurons are silent when cholinergic PGO spike discharge initiated REM sleep (Reserpine (->essential hypertension) which deplete serotonin and catecholamines, blocks slow-wave sleep and some aspects of REM sleep but increases PGO spike activity) d. Adenosine I. Its concentration changes in some of the sleep areas during sleep -> Sleep producing factor? II. Consistent with alerting effects of caffeine, which is an adenosine antagonist |
|
|
Sleep disorders
a. Somanmbulism b. Narcolepsy c. REM behavior disorder |
a. Somnambulism\Sleep walking
I. Occur during slow-wave sleep\arousal from slow-wave sleep (So does bed wetting\nocturnal enuresis and night terrors) II. More common in children and males III. Walk with eyes open and avoid obstacles, but have no recollection b. Narcolepsy I. Disease characterized by episodic hypotonia and irresistible urge to sleep during daytime activities II. Awave -> REM (sometimes) (Uncommon in normal individuals) III. Orexins\Hypocretins deficiency seem to be involved (Lower levels in CSF of patients with narcolepsy, Labrador strain with defect of receptors have narcolepsy) c. REM behavior disorder I. Hypotonia fails to occur during REM -> Patients 'Act out' on their dreams - Thrash about, jump out of bed, ready to battle with imagined aggressors (Like cats with locus ceruleus lesions, respond to benzodiazepine treatment) (Ganong) |
|
|
EEG
a. Diagnostic applications |
a. Diagnostic applications of EEG
1. Hematomas (ie subdural) overlying a part of the brain can dampen the cortical activity recorded 2. Cortical lesions -> Irregular or slow waves 3. Epilepsy - Epileptogenic foci -> High-voltage waves (Ganong) |
|
|
Motor systems
a. UMN lesion - Distinction b. General scheme of control of voluntary movement c. ALS - Synonym, what, cause of most of the familial cases |
a. UMN lesion - Distinction
1. Lesions of the posture-regulating pathways -> Spastic paralysis 2. Lesions limited to the corticospinal and corticobulbar tracts -> Paresis (Demonstrated by selective lesions in monkeys. The anatomic arrangement in humans are such that disease processes rarely, if ever, damage the corticospinal and corticobulbar tracts without also destroying posture-regulating pathways) 3. Cerebellar lesions -> Incoordination b. General scheme for control of voluntary movement 1. Idea -> 2. Cortical association areas -> 3. Premotor and motor cortex -> I. Collaterals of the projections of the cortical association areas project to basal ganglia and the lateral cerebellum as well. These in turn have reciprocal connections with 3. via VL of thalamus 4. -> Movement I. Collaterals to intermediate cerebellum which functions as a comparator - It receives constant feedback information from propriocepive receptors and adjust\smoothes the movement II. Feedback-system with premotor and motor cortex as well c. Amyotrophic lateral sclerosis (ALS)\Lou Gehrig Disease I. Degeneration of lower motor neurons and corticospinal tract II. Most of the familial cases have a mutation in the gene for Cu\Zn superoxide dismutase (SOD-1) -> Permit free radicals to accumulate and kill neurons (Only 5% are familial) (Ganong) |
|
|
Babinski sign
a. +Babinski sign b. Occur when c. Mechanism |
a. +Babinski sign
I. Dorsiflexion of the great toe and fanning of the other toes in response to scratching of the lateral aspect of the sole II. The normal response is plantar flexion b. The lateral corticospinal tract is damaged c. The Babinski sign is believed to to be a flexor withdrawal reflex that is normally held in check by the lateral corticospinal system (Pathological except in infants) (Ganong) |
|
|
Motor system - Spinal cord
a. Cause of hyperactivity in the area below a spinal cord lesion b. Spinal cord - Reflexes c. Spinal shock - Duration d. Spinal shock - Change in LMNs |
a. Cause of hyperactivity in the area below a spinal cord lesion
1. Release\Removal of an inhibitory control by higher neural centers 2. Loss of differentiation of the reaction, so that it no longer fits into the broader pattern of motor activity 3. Denervation hypersensitivity b. Spinal cord - Reflexes 1. Stretch reflexes 2. Golgi tendon reflexes 3. Positive supporting (magnet) reaction (Contact with sole of palm -> foot extends to support body) 4. Negative supporting reaction c. Spinal shock - duration I. Minimum 2 weeks in humans (Related to degree of encephalization - lasts for minutes in frogs and rats) d. Spinal shock - Change in LMNs I. The resting membrane potential is 2-6 mV greater than normal - hyperpolarized (Ganong) |
|
|
Spinal cord transection - Paraplegia and quadriplegia
a. Complications b. Mortality c. Treatment options |
a. Complications of quadriplegia and paraplegia
1. Decubitus ulcers I. Negative nitrogen balance (like all immobilized patients) -> Less 'protective' tissue between skin and bony prominences II. Heal poorly and are prone to infection due to protein depletion 2. Calcium stones in urinary tract I. Protein depletion in bone matrix -> Release of calcium -> Hypercalcemia -> Hypercalciuria 3. Urinary tract infection I. Most common complication of spinal cord injury II. Usually followed by urinary stasis caused by urinary stones and paralysis of bladder b. Mortality - 6% c. Treatment options 1. High-dose glucocorticoids immediately following the injury I. Reduce the inflammatory response in the damaged tissue 2. Baclofen I. GABA-B agonist II. Muscle relaxing effect on spasticity, analgesic (Experimental - Neurotrophin administration, Embryonic stem cell implantation, Bypass the site of transection by brain-computer interface devices) (Ganong) |
|
|
Decerebrate rigidity
a. Decerebration - What, effect b. Decerebrate rigidity - Mechanism c. Significance of decerebrate rigidity d. Decorticate rigidity - What |
a. Decerebration
I. Operative procedure where the brainstem is sectioned at the superior border of the pons II. Produce decerebrate rigidity a. Decerebrate rigidity - Mechanism I. Due to diffuse facilitation of stretch receptors - From 1. Increased general excitability of the motor neuron pool - Vestibulospinal tract in particular II. Increase in the rate of discharge in the gamma efferent neurons - The balanced is shifted toward facilitation (Facilitatory centers - RF facilitatory area (dominant), Inhibitory - Cortical, Basal ganglia, Cerebellum, RF inhibitory area) c. Significance of decerebrate rigidity I. Sherrington - "Caricature of the normal standing position" (Activation of the muscles which resist gravity, the extension in the arms of humans is due to the near relationship phylogenetically to quadruped ancestors) (Additional evidence that it is facilitation of the normal standing\base position comes from decerebration in sloth, an arboreal animal that hangs upside down from branches most of the time. Decerebration here cause rigidity in flexion) d. Decorticate rigidity I. Extension in lower limbs, flexion in upper II. Due to lesions of the cerebral cortex, with msot of the brainstem intact (Ganong) |
|
|
Decorticate rigidity
a. What b. Caused by c. When is it usually seen in humans d. Suppressor strip |
a. Decorticate rigidity
I. Upper limb flexion, lower limb extension b. Caused by removal of cortex in experimental animals. This removes the cortical and basal ganglia inhibition of the gamma efferent system c. On the hemiplegic side in humans after hemorrhages or thromboses in the internal capsule (Certain characteristics of the arteries to the internal capsule make them especially prone to rupture or thrombosis. 60% of intracerebral hemorrhages occur here, 10% in cerebral cortex, 10% in the pons, 10% in the thalamus, and 10% in the cerebellum) d. Suppressor strip\4s I. Anterior edge of the precentral gyrus II. In certain experiments, stimulation has caused inhibition of the stretch reflexes (Ganong) |
|
|
Vomiting
a. Mechanism\Procedure b. Location of vomiting center c. Afferents d. Treatment options |
a. Mechanism\Procedure
1. Salivation and sensation of nausea 2. Reverse peristalsis - Upper small intestine -> Stomach 3. Glottis close to prevent aspiration 4. The breath is held at mid-inspiration, abdominal muscles contract increasing intra-abdominal pressure, and the lower esophageal sphincter and esophagus relax 5. Vomit b. Vomiting center - Part of RF in medulla oblongata I. Various scattered groups of neurons in this region that control the different components c. Afferents 1. Irritation of mucosa of the upper GIT -> Sympathetic and vagal afferents 2. Vestibular nuclei afferents mediate the nausea and vomiting of motion sickness 3. Descending from diencephalon and limbic system - "Nauseating smells" and "sickening sights" 4. Chemoreceptor trigger zone in area postrema I. V-shaped band of tissue on the lateral walls of the fourth ventricle near the obex II. One of the circumventricular organs III. React to apomorphine, digitalis glycosides, chemotherapeutic drugs IV. Mediate vomiting of radiation sickness and uremia (Both may produce endogenous emetig substances) 5. Enterochromaffin cells in the small intestine mediate vomiting serotonergically by acting on 5-HT3 receptors d. Treatment options 1. 5-HT3 antagonists I. Ondansetron II. 5-HT3 peripherally associated with enterochromaffin cells, 5-HT3 in the area postrema and adjacent nucleus of the solitary tract 2. Dopamine D2 antagonists I. Chlorpromazine, haloperidol II. Dopamine D2 receptors in the area postrema and nucleus of the solitary tract 3. Corticosteroids I. Unknown mechanism 4. Cannabinoids I. Unknown mechanism 5. Benzodiazepines I. Probably reduce the anxiety associated with chemotherapy (Ganong) |
|
|
Hypothalamus
a. Median eminence b. Mechanism of circadian genes and their products in the suprachiasmatic nucleus (SCN) c. CRH - Integrating areas, afferents from |
a. Median eminence
I. The portion of the ventral hypothalamus from which the portal vessels arise II. Outside the BBB b. Mechanism of circadian genes and their products in the SCN 1. Genes are activated diurnally 2. Their protein products enter the cytoplasm where they modify cell function and neuronal discharge 3. They then migrate into the nucleus where they exert negative feedback on the genes that they produced them c. CRH I. Integrating area in paraventricular nuclei II. Afferents from 1. Limbic system - Emotional stimuli 2. Reticular formation - "Systemic" stimuli 3. Hypothalamic and anterior pituitary cells sensitive to circulating blood cortisol level 4. SCN - Diurnal rhythm (Ganong) |
|
|
Feeding and satiety
a. Feeding center - Location, effect of stimulation and lesion b. Satiety center - --||-- c. Orexigenic substances - Increase food intake d. Antiorexigenic substances - Decrease food intake |
a. Feeding center
I. The bed nucleus of the medial forebrain bundle at its junction with the pallidohypothalamic fibers (MLF course laterally through hypothalamus. Hypothalamus <--> midbrain tegmentum, limbic system. Also carries NA and 5-HT fibers to hypothalamus and cerebral cortex and the nigrostriatal path) II. Stimulation -> Eating behavior III. Lesion -> Fatal anorexia b. Satiety center I. Ventromedial nucleus of hypothalamus II. Stimulation -> Cessation of eating III. Lesion -> Hyperphagia, hypothalamic obesity c. Orexigenic substances 1. Neuropeptide Y I. Its mRNA increase during feeding and decrease during satiety in hypothalamus II. Y5 receptor 2. Orexin-A and B I. Synthesized in neurons of lateral hypothalamus (Mutation in one of its receptors genes cause narcolepsy in a Labrador dog strain) 3. Melanin-concentrating hormone (MCH) I. Lateral hypothalamus, zona incerta 4. Endogenous cannabinoids I. Via CB-1 receptors 5. Ghrelin (Ghre- growth, stimulate GH-releasing cells in hypophysis, produced by gut, higher during fasting) (+ AGRP, Beta-endorphin. galanin, ghrelin, GHRH, MCH) d. Antiorexigenic substances 1. POMC derivatives - alpha-MSH I. MC4-R mediate effects on apeptite (MC1-R - Skin pigmentation, MC2-R - Adrenal glucocorticoid prudcution..) (A mutant strain of obese mice called agouti overproduces the agouti protein that inhibits the action of alpha-MSH on the MC4-receptor) 2. Cocaine- and amphetamine-regulated transcript (CART) 3. CRH 4. Leptin (+ Bombesin, CCK, CGRP, Glucagon, GLP-1,2, GRP, Neurotensin, Oxytocin, Peptide YY, Somatostatin) (Ganong) |
|
|
Food intake regulation
a. Afferent mechanisms involved in the control of food intake b. Leptin - Evidence for its role, mechanism c. Leptin - Peripheral effects\associations d. Monogenic causes of morbid obesity |
a. Afferent mechanisms involved in the control of food intake
1. The lipostatic hypothesis I. Adipose tissue produces a humoral signal that is proportionate to the amount of fat and acts on the hypothalamus to decrease food intake and increase energy output II. Leptin 2. The gut peptide hypothesis I. Food in the GIT -> Release of peptides that act on the hypothalamus to inhibit food intake II. Peptide YY (<- Small intestine and colon) III. GRP, glucagon, Somatostatin, CCK 3. Glucostatic hypothesis I. Increased glucose utilization in the hypothalamus produce a sensation of satiety I. Appear to be in ventromedial nucleus (Food intake is rapidly increased by intraventricular administration of compounds such as 2-deoxyglucose that decrease glucose utilization in the cells, polyphagia in diabetes) 4. The thermostatic hypothesis I. Fall in body temperature below a given set point stimulates appetite while a rise above the set point inhibits appetite b. Leptin ('Thin') I. Homozygous recessive mice with defect ob gene (obesity gene - its gene product is leptin) do not become sated after eating and become obese and diabetic, so does mice with mutations of its receptor and mice where the arcuate nuclei (which contains the highest density of its receptors) is lesioned by gold thioglocuse (Long form of receptor in arcuate nucleus, short form in brain microvessels associated with transport across BBB) II. Seems to inhibit Neuropeptide Y and stimulate POMC-secreting neurons c. Leptin - Peripheral effects\associations 1. Low levels in rodents cause inhibition of onset of puberty, ↓thyroid function, ↑glucocorticoids d. Monogenic causes of morbid obesity 1. Homozygous defective ob\ob I. -> Leptin II. Uncommon 2. Homozygous defective db\db I. -> Leptin receptor II. More common as evidenced by high leptin levels in many obese individuals 3. Loss-of-function mutation of the gene for the MC4 receptor I. Ligand is the antiorexigenic derivatives of POMC, especially alpha-MSH (Ganong) |
|
|
Thirst
a. Regulation - The 2 main mechanisms b. Other factors regulating water intake |
a. Regulation
1. Osmolality I. Hypertonicity -> osmoreceptors in anterior hypothalamus 2. Hypovolemia I. RAS -> ATII, receptors in subfornical organ (SFO) and probably in organum vasculosum of lamina terminalis (OVLT) (Circumventricular organs) II. Baroreceptors - Heart, blood vessels (Postulated since ATII blockers don't completely block the thirst response to hypovolemia) b. Other factors regulating water intake 1. Prandial drinking - ↑Intake during eating (Osmolality? GIT hormone?) 2. Dryness of the pharyngeal mucosa (Ganong) |
|
|
Vasopressin
a. Synthesis b. Receptors c. Effects d. Desmopressin\DDVP e. Regulation + f. Regulation - |
a. Synthesis
I. Synthesized as prepropressophypophysin -> Signal peptide, vasopressin, neurohypophysin II, glycopeptide II. By magnocellular neurons of supraoptic nuclei mainly (Nonapeptide with disulfide bond) b. Receptors 1. V1A, V1B - Gq 2. V2 - Gs c. Effects 1. V2 in kidneys -> Translocation of aquaporin 2 from endosome to luminal membrane in principal cells of the collecting ducts (AP1-3 in kidneys, AP4 in brain) 2. Vasoconstriction I. V1A (Partly antagonized by its effect to decrease CO by acting on area postrema) 3. Neurotransmitter in brain and spinal cord 4. Mediate ↑ACTH from corticotropes in anterior pituitary I. V1B\V3 d. Desmopressin I. Synthetic analog II. High antidiuretic effect relative to vasopressor effect (-> Valuable in central diabetes insipidus to avoid hypertension) e. Regulation + 1. ↑Osmolality - OVLT, 285 mOSM 2. ↓ECF I. Via low-pressure receptors primarily (atria, great veins, pulmonary vessels) 3. Pain, emotion, "stress", exercise 4. N&V 5. ATII - Act on circumventricular organs 6. Clofibrate, carbamazepine f. Regulation - 1. ↓Osmolality 2. Hypervolemia 3. Alcohol (Ganong) |
|
|
Vasopressin
a. Regulation + b. Regulation - c. SIADH - What, Effect, Cause, Treatment |
a. Regulation +
1. ↑Osmolality - OVLT, 285 mOSM 2. ↓ECF I. Via low-pressure receptors primarily (atria, great veins, pulmonary vessels) 3. Pain, emotion, "stress", exercise 4. N&V 5. ATII - Act on circumventricular organs 6. Clofibrate, carbamazepine b. Regulation - 1. ↓Osmolality 2. Hypervolemia 3. Alcohol c. SIADH I. Hypersecretion II. -> Dilutional hyponatremia (Worsened by ↑ECF -> ↓Aldosterone -> ↑Renal salt loss) III. Paraneoplastic - lung cancer (Can also be by the cancer interrupting the inhibitory impulses vagal afferents from stretch receptors in the atria and great veins) IV. Demeclocycline is used for treatment, its a antibiotic that reduce the renal response to vasopressin |
|
|
Motivation and addiction
a. Points where self-stimulation leads to repeated bar pressing b. Points where self-stimulated leads to decreased bar-pressing c. Involved neurotransmitter d. Addiction e. Common mechanism of opioids, cocaine, amphetamine, nicotine, alcohol, cannabinoids |
a. Points where self-stimulation leads to repeated bar pressing
I. MEdial band of tissue from the ventral tegmentum to the frontal cortex - Ventral tegmentum, medial forebrain bundle, nucleus accumbens, prefrontal cortex (Feeling described as pleasurable - "relief of tension", "quiet, relaxed feeling", not joy\ecstacy) b. Points where self-stimulated leads to decreased bar-pressing 1. Lateral posterior hypothalamus 2. Dorsal midbrain 3. Entorhinal cortex (Described as vague fear, terror) c. Neurotransmitter I. Dopamine D3 antagonist reduce the rate of self-stimulation, dopamine agonist increase it II. The main site of D3 receptors is in nucleus accumbens d. Addiction I. The repeated, compulsive use of a substance despite negative health consequences. d. Increase the amount of dopamine available to act on D3 receptors in the nucleus accumbens (Ganong) |
|
|
Serotonin
a. Serotonergic projections from the raphe nuclei b. 5-HT2 agonists - Which, effect c. 3,4-Methylene-dioxy-meth-amphetamine (MDMA) - Street name, effect, mechanism d. Other effects |
a. Serotonergic projections from the raphe nuclei
1. The hypothalamus 2. The limbic system 3. The neocortex 4. The cerebellum 5. The spinal cord b. 5-HT2 agonists I. Hallucinogenic II. Members 1. Lysergic acid diethylamide (LSD) 2. Psilocin, N,N-dimethyltryptamine (DMT), Psilocybin - Mushrooms (1-2 are derivatives from tryptamine) 3. Mescaline - Cactus c. MDMA I. Ecstacy II. Produce euphoria followed by concentration problems, depression, and insomnia III. Cause release of serotonin followed by serotonin depletion - analogous to the effect d. Other effects 1. Descending analgesic system 2. Serotonergic innervation of SCN of hypothalamus is involved in the regulation of circadian rhythm 3. Mood (ganong) |
|
|
Norepinephrine
a. The locus ceruleus system b. The lateral tegmental systems c. Function |
a. The locus ceruleus system
1. Locus ceruleus -> 2. Dorsal noradrenergic bundle -> 3. Spinal cord, cerebellum, hypothalamic nuclei, thalamus, basal telencephalon, neocortex b. The lateral tegmental system 1. Cell bodies in the dorsal motor nucleus of vagus, the nucleus of tractus solitarius, areas in the dorsal and lateral tegmentum -> 2. Ventral noradrenergic bundle -> 3. Spinal cord, brainstem, hypothalamus, basal telencephalon c. Function I. Locus ceruleus system - Uncertain, behavioral vigilance? (Increased activity by unexpected sensory stimuli) II. The ventral tegmental system - Regulation of hypothalamic hormones III. Other - Mood, body temperature (Ganong) |
|
|
Dopamine
a. Ultrashort dopamine neurons b. Intermediate-length dopamine neurons c. The long dopamine systems d. Association with schizophrenia |
a. Ultrashort dopamine neurons
1. Cells between the inner nuclear and the inner plexiform layer in the retina 2. Periglomerular cells in the olfactory bulb b. Intermediate-length dopamine neurons 1. Tuberoinfundibular system 2. Incertohypothalamic system (Zona incerta - Aggregate in subthalamic region) (Link hypothalamus and the lateral septal nuclei) 3. Medullary periventricular group c. The long dopamine systems 1. The nigrostriatal system 2. The mesocotical system (Large part from VTA to nucleus accumbens) d. Association with schizophrenia 1. Amphetamine which cause release of dopamine (+NA) in the brain cause a schizophrenia-like psychosis 2. Brain levels of D2 receptors are elevated in schizophrenic patients 3. Clear +correlation between the antischizophrenic activity of many drugs and their ability to block D2 receptors (However, several effective antipsychotic agents have their main antagonistic effect on D4) (Ganong) |
|
|
Higher mental functions |
a. Angular gyrus\39 - Effect of isolated lesion
I. Only trouble understanding written language\pictures, since visual information is not processed at transmitted to Wernicke's area b. Dyslexia 1. Reduced ability to recall speech sounds -> Problems with translating them mentally into phonemes (sound units) 2. Defect in the magnocellular portion of the visual system -> Slowed visual processing, phonemic deficit (5% of population, associated with decreased blood flow to angular gyrus in the categorical hemisphere) c. Prosopagnosia I. caused by lesion in the inferior temporal lobe of the representational hemisphere d. Acalculia - Caused by lesion in I. Frontal lobe |

