![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
40 Cards in this Set
- Front
- Back
|
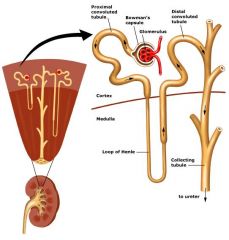
Nephron
|
|
|
|
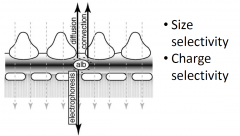
Barriers to proteinuria
|
|
|
|
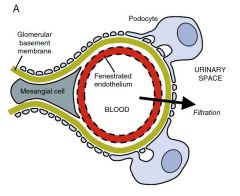
Glomerular filtration barrier
|

|
|
|
Forces across the glomerular filtration barrier
|
|
|
|
Normal Filtration
|
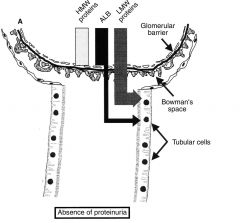
i.e no proteinuria
|
|
|
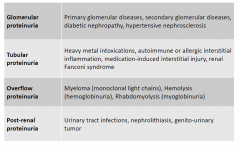
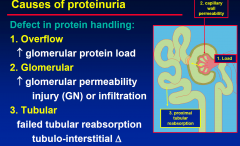
Glomerular proteinuria
|
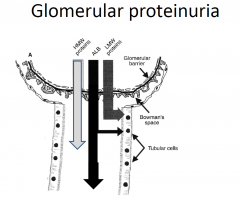
GLOMERULAR INJURY
- eg immune GN OR glomerular inflitration - DN - amyloidosis |
|
|
Tubular proteinuria
|
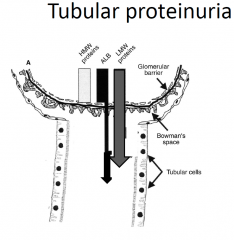
• tubulointerstitial disease
• failed small MW reabsorption eg analgesic nephropathy OR Chronic interstitial nephritis (thick & lots of fibrosis thus little reabsorption) |
|
|
Overflow proteinuria
|
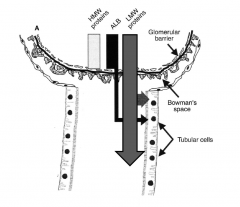
excerssive protien load
eg myeloma kidney |
|
|
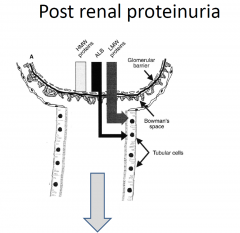
Post renal proteinuria
|
|
|
|
Proteinuria
types and their causes |
|
|
|
Detection of proteinuria
|
•Urinary dipstick
•24 hour urine collection for protein •Spot urine for protein and creatinine •Spot urine for microalbumin and creatinine |
|
|
Urinary dipstick
|
•Common screening tool
•Primarily detects albuminuria and cannot detect LMW proteins •Result is based on colour reaction •Considered positive if >+1 |
|
|
Proteinuria and Dipstick
|
•False positive results;
Concentrated urine Prolonged immersion Alkaline urine (pH>7) Antiseptics Pyuria, bacteriuria, mucoproteins •False negative results; Dilute urine Acidic urine (pH<4.5) |
|
|
24 hour urine collection
|
•Quantification of proteinuria
•Normal< 150mg/24h •Proteinuria 150-3.5g •Nephrotic >3.5 g/24h •?accuracy: check with u creatinine •inconvenient |
|
|
Spot urine pr/cr ratio
|
Uses creatinine to estimate concentration of urine
•Easy to perform •Good correlation with daily protein excretion across population •Measures all protein Positive if >30mg/mmol |
|
|
Spot urine alb/cr ratio
|
Measures only albumin but able to detect low levels
•Positive if >2.5 mg/mmol (men) and >3.5 mg/mmol (women) •Used as a screening test |
|
|
Microalbuminuria
|
•Dipstick negative for protein
•Glomerular protein •By lowering the threshold of detection of proteinuria, we increase the sensitivity of the test •Early detection of diabetic nephropathy and any other glomerular for of proteinuria |
|
|
Issues with pr/cr and alb/cr ratio
|
•Influenced by total daily creatinine production/excretion
–Muscle mass –Change to renal function •Variability in protein excretion |
|
|
Australasian Proteinuria Consensus Working Group 2012
|
•The preferred method for assessment of albuminuria in both diabetic and non-diabetic individuals is urinary albumin-to-creatinine ratio (UACR) measurement in a first-void (first morning) spot specimen. Where a first-void specimen is not possible or practical, a random spot urine specimen for UACR is acceptable.
•Adults with one or more risk factors for CKD should be assessed using UACR and eGFR every 1–2 years, depending on their risk-factor profile. •A positive UACR test should be repeated to confirm persistence of albuminuria. CKD is present if two out of three tests (including the initial test) are positive. |
|
|
Assessment of proteinuria
|
•Quantify proteinuria:
–Microalbuminuria –Non nephrotic range proteinuria –Nephrotic range proteinuria –Nephrotic syndrome •Examine the urine for other abnormalities •Assess renal function •Assess blood pressure |
|
|
Proteinuria Ranges
|
-Normal <150mg/24h
–Microalbuminuria >30mg/day –Non nephrotic range proteinuria 150-3500mg/day –Nephrotic range proteinuria (>3.5g/24h) –Nephrotic syndrome Urine dipstick UNITS; mg/dL UACR: units mg/day |
|
|
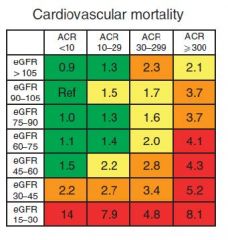
Implications of persistent proteinuria
|
•May be the sign of an underlying kidney disease (e.g glomerulonephritis)
•May be the only indicator of ongoing kidney damage (e.g. diabetic nephropathy) •Typically precedes the deterioration of GFR •Not only a marker of disease but can contribute to scarring itself •With or without CKD, proteinuria is a cardiovascular risk factor |
|
|
Proteinuria and CV Risk
|
|
|
|
Pathophysiology of proteinuria
|
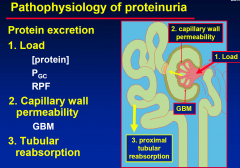
|
|
|
Causes of Proteinuria
|
|
|
|
Types of Proteinuria
|
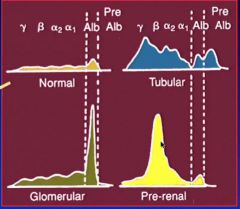
|
|
|
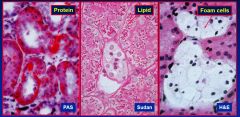
Effects of proteinuria
|
Presentations:
• asymptomatic • frothy urine • nephrotic syndrome Clinical consequences: • tubular overload & CRF • urinary losses & deficits |
|
|
Tubular overload by proteinuria
• filters potentially toxic substances -> CRF |
|
|
|
Proteinuria: Clinical questions
|
Proteinuria: Clinical questions
1. How much? 2. What conditions? • orthostatic, transient or persistent 3. Type of protein excreted • glomerular or tubular, overflow 4. Other urinary findings (hematuria etc.) 5. Associated conditions & age |
|
|
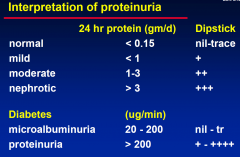
1. Degree of proteinuria
|
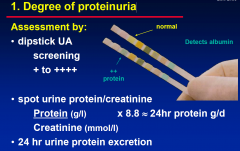
|
|
|
Interpretation of Proteinuria
|
|
|
|
Dipstick urinalysis: Problems:
|
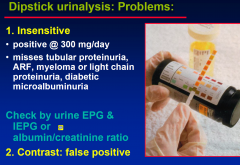
|
|
|
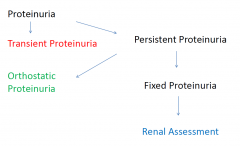
Conditions of proteinuria
|
(i) Transient proteinuria
(ii) Orthostatic proteinuria (iii) Persistent proteinuria |
|
|
Transient proteinuria
|
Transient proteinuria
• common: 4% of male & 7% of females • stressors: fever & exercise (up to 1.5 mg/min) • albumin & LMW proteins Diagnosis: • repeat urine protein estimation |
|
|
Orthostatic proteinuria
|
Definition:
• “upright position” proteinuria & • normal supine protein excretion (< 50 mg / 8hrs) Characteristics • children & adolescents • normal renal function • no hematuria |
|
|
Orthostatic proteinuria
Prognosis: Dx: |
Orthostatic proteinuria
Prognosis: • generally benign • 50% resolution in 10 yrs, 83% by 20 yrs Diagnosis: split urine collection 1. Daytime collection (16 hrs) • 7am - 11pm upright with last 2 hrs supine 2. Overnight collection (8 hrs) • 11pm - 7am, supine |
|
|
Persistent proteinuria
|
1. Primary renal disease
• membranous, FSGS, MCD, MCGN • mesangial proliferative GN, PSGN 2. Secondary to systemic disorder • diabetic nephropathy • benign hypertensive nephrosclerosis • amyloid, myeloma, CCF etc. |
|
|
Approach to proteinuria
|
Define
• grade of proteinuria (> 1 gm/day) • hematuria • renal function • blood pressure • associated diseases (e.g. diabetes) • renal pathology |
|
|
Proteinuria workup
|
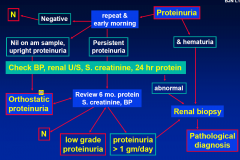
• repeat urine protein
• MSU for hematuria & casts • urine EPG/IEPG • serum creatinine • 24 hr urinary protein (split in young) • renal ultrasound • renal biopsy if high grade, hematuria or impaired renal function |
|
|
Treatment of proteinuria
|
Treat underlying condition
• nil, steroids and/or cytotoxics Salt restriction 100 mmol/day Adequate protein intake (not excessive) Diuretics: frusemide +/- spironolactone ACE inhibitors Control hypertension (BP can enhance renal injury) Warfarin if thromboembolism Pneumovax |

