![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
63 Cards in this Set
- Front
- Back
|
Define Pressure injury: |
Localized area of tissue necrosis that develops when soft tissue is compressed between a firm surface and underlying bony prominence |
|
|
Who is at the greatest risk for pressure injuries? |
-individuals with spinal cord injuries -hospitilized pt -individuals in long-term care facilities |
|
|
What is the etiology of pressure-related cell death? |
Pressure Ischemia Acidosis Inflammation Increased capillary permeability and edema Local tissue anoxia Necrosis |
|
|
What is the formation of a pressure injury a result of? |
-inverse pressure- time relationship -individual hemodynamic factors -body location |
|
|
What areas are at greatest risk for pressure injury? |
areas overlying bony prominences |
|
|
Is skin or muscle more sensitive to pressure? |
muscle |
|
|
Will you immediately see a pressure injury? |
-no it may not develop for days after the pressure was applied -extensive skin damage may have already occurred before skin changes |
|
|
What is reactive hyperemia? |
localized area of blanchable erythema |
|
|
What is the shape of pressure distribution? |
cone |
|
|
What are the risk factors contributing to pressure injuries? |
Shear Malnutrition Excessive Moisture Impaired Mobility Impaired Sensation Advanced age Hx of pressure injury* |
|
|
Describe shear as a risk factor for pressure injuries: |
Shear= force parallel to soft tissue -may have teardrop appearance -undermining common -Friction= two surfaces moving across one another |
|
|
Describe Malnutrition as a risk factor for pressure injuries: |
-second most common risk factor -low serum albumin levels and/or hydration -correlated with injury* severity -pt. may be underweight, normal weight, or obese |
|
|
Describe Moisture as a risk factor for pressure injuries: |
Predisposes skin to PI by -causing maceration -increasing shear -increasing friction forces Maceration caused by -wound drainage -perspiration -incontinence Anhydrous skin also at risk |
|
|
Describe Impaired mobility as a risk factor for pressure injuries: |
-factors affecting pt. ability to move -affecting pt. desire to move -affecting pt. ability to perceive pn. -most frequently studied causes -hospitilization -fracture -SCI -infant/neonates |
|
|
Describe impaired sensation as a risk factor for pressure injuries: |
Unable to detect pain of ischemic tissue damage caused by pressure -SCI -spina bifida -storke -DM -Full-thickness burns -peripheral neuropathy |
|
|
Describe advanced age as a risk factor for pressure injuries: |
-more than half of pt. w/ pi are over 70 yo -age-related skin changes -increaed rate of comorbidities |
|
|
Describe Previous pressure injury as a risk factor for pressure injuries: |
-scar tissue only attains up to 80% strength of the original tissue -scar tissue alters tolerance to pressure and externally applied |
|
|
What are the additional risk factors for pressure injuries? |
-ischemia-reperfusion injuries -polypharmacy -low diastolic pressure -psychosocial factors -smoking -diabetes-related microvascular changes -increased skin temp -Alzheimer's disease -Parkinson's disease -RA |
|
|
What are the most widely used risk assessment tools for pressure injuries? |
-Braden Scale for Predicting Pressure Sore Risk -Norton Risk Assessment Scale -Gosnell Pressure Sore Risk Assessment |
|
|
Explain the Braden Scale: |
-score range from 6-23, with lower scores indicating greater impairment and higher risk -score <18 deemed at-risk pt. -higher interrater reliability -Braden Q scale for pediatric pt. |
|
|
Braden Scale for Predicting Pressure Ulcer Development: |
Mobility: ability to change and control body position (1=completely immobile, 4= no limitations) Activity: degrees of physical activity (1= bedfast, 4=walks frequently) Sensory Perception: ability to meaningully respond to pressure related discomfort (1=completely limited, 4= no impairment) Skin moisture: degree to which skin is exposed to moisture (1=constant, 4- rarely) Nutritional status: usual food intake (1=very poor, 4= excelent) Friction and shear: degree to which pt. is able to move without sliding (1=problem, 4= no apparent problem) |
|
|
Describe the Norton Risk Assessment Scale: |
-each scale is rated 1-4, with lower scores indicating greater risk of pressure injury development -score of < or = to16 considered at risk -may overpredict incidence of pressure injuries -norton plus pressure injury *scale |
|
|
Norton Pressure Ulcer Scale: |
Physical Condition: 1=very bad, 4=good Mental condition: 1=stupor, 4= alert Activity: 1=bed bound, 4= ambulatory Mobility: 1=immobile, 4=full Incontinence: 1=incontinent of bowel and bladder, 4=not incontinent (one point deductions for each of the following: DM, hyptn, low hematocrit, low hemoglobin, low albumin, fever, 5+ medicaitons, or changes in mental status over past 24 hours) |
|
|
Describe the Gosnell Pressure Sore Risk Assessment: |
-five subscales: mental status, continence, mobility, activity, and nutrition -each scale is rated 1 to 5, with 1 being the least impaired -16 is the critical cut-off score -least researched |
|
|
What is the interdisciplinary intervention for pi prevention? |
-education -positioning -mobility -nutrition -manage incontinence |
|
|
What is the NO ULCERS mnemonics for pressure ulcer prevention? |
N: nutrition and fluid status O: observeation of skin U: up and walking or assist with position changes L: lift, don't drag C: clean skina nd continence care E: elevate heels R: risk assessment S: support surfaces |
|
|
What is the SKIN mneumonic for pressure ulcer prevention? |
S: surface selection K: keep turning I: incontinence management N: nutrition |
|
|
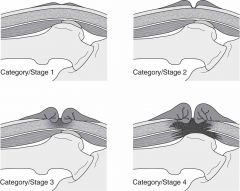
Explain category/stage I for the International NPUAP/EPUAP Pressure injury Classification system: |
-nonblanchable erythema of intact skin -skin color may appear different from surrounding tissue -area may be painful, warmer, cooler, firmer, softer than surrounding tissue Tissues involved: -may be superficial -may be first sign of deeper tissue involvement |
|
|
Explain category/stage II for the International NPUAP/EPUAP Pressure injury Classification system: |
-superficial injury * -shallow crater without slough or bruising -may be ruptured or intact blister Tissue involved: -partial thickness (with exposed dermis) |
|
|
Explain category/stage III for the International NPUAP/EPUAP Pressure injury Classification system: |
-deep injury * -may have undermining or tunneling and epibole Tissue involved: -full thickness (epidermis, dermis, subcutaneous tissue) -bone/tendon not visible -slough and/or eschar may be visible |
|
|
Explain category/stage IV for the International NPUAP/EPUAP Pressure injury Classification system: |
Deep injury* with extensive necrosis -often has underming or sinus tracts Tissue involved: -full thickness -underlying deep tissue exposed bone, muscle, tendon or palpable -if eschar obscures the extent of tissue loss it becomes unstageable |
|
|
Explain category/stage UNSTAGEABLE/UNCLASSIFIED for the International NPUAP/EPUAP Pressure injury Classification system: |
Pressure injury* with base obscured by eschar or slough Tissue invovled: -full thickness -will be category III or IV |
|
|
Explain category/stage Deep tissue injury for the International NPUAP/EPUAP Pressure injury Classification system: |
Local area of purple or maroon discoloration of intact skin or a blood-filled blister Persistent non-blanchable -may be painful, firm, mushy, boggy, warmer, or cooler than surrounding tissue -may evolve and become eshcar covered Tissue involved unknonw |
|
|
Categories/stages of pressure injury pics: |
|
|
|
What are the benefits of international NPUAP/EPUAP PU classification system? |
-promotes uniform understanding of the depth of tissue involved -excellent reliability -clinicians must stage pressure injuries for medicare reimbursement -determines type of support surface to be used -can be used for research studies |
|
|
What are the limitaitons of internation NPUAP/EPUAP PU classification system? |
-Category/stage I pressure injury is not an injury by definition -Clinicians may erroneously 'reverse stage' a pressure injury * -significant revision of prior system - may take time to adapt to and use correctly |
|
|
What can we use to look at the characteristics of pressure injury? |
5 PT method Pain Position Presentation Periwound Pulses Temperature |
|
|
Describe pain as it relates to a characteristic of pressure injuries: |
-McGill pain questionare, Visual analog scale, faces pain scale -category I pi may be tender instead of painful -pt. with neurological deficits may not perceive pain -pt. who are unable to communicate may demonstrate pn. by grimacing, withdrawal, or moaning |
|
|
Describe position as it relates to a characteristic of pressure injuries: |
-Majority on lower half of body over boney prominence -95% or pi located over: sacrum, greater trochanter, ischial tuberosity, posterior calcaneous, lateral malleolus -areas of outside pressure: casts, tubing, shoes |
|
|
What are the most common locations for pi while in supine position? |
-posterior heel -sacrum/coccyx -scapula -occiput -medial humeral epicondyle -spinous process if emaciated |
|
|
What are the most common locations for pi while in prone? |
-anterior knee -anterior tibia -iliac crest |
|
|
What are the most common locations for pi while sidelying? |
-greater trochanter -malleolus -femoral condyle if emaciated -ear -lateral humeral epicondyle |
|
|
What are the most common locations for pi while sitting? |
-ischial tuberosity -greater trochanter (if sling like seat) -sacrum/coccyx (if in posterior pelvic tilt) |
|
|
Describe presentation as it relates to a characteristic of pressure injuries |
-international NPUAP/EPUAP injury classification system provides detailed descriptions -pt. with full-thickness pi more likely to have multiple injuries |
|
|
Describe periwound and structural changes as it relates to a characteristic of pressure injuries |
-nonblanchable erythema -mottled -ring of inflammation around injury* -dermatitis |
|
|
Describe pulses as it relates to a characteristic of pressure injuries |
-usually not applicable due to proximal injury locaiton -usually normal unless concomitant PVD |
|
|
Describe temperature as it relates to a characteristic of pressure injuries |
-increased in areas of reactive hyperemia -decreased in areas of ischemia |
|
|
What is the sessing scale? |
7 point observational scale describing wound and periwound characteristics -scores range from 0-6 -used in clinic and research settings |
|
|
Sessing Scale: |
0: normal skin, but at risk 1: skin completely closed, may lack pigmentation or may be reddened 2: wound edges and center are filled in, surrounding tissues are intact and not reddened 3: wound bed filling with pink granulating tissue, slough present, free of necrotic tissue, minimum drainage and odor 4: moderate to minimal granulating tissue, slough and minimal necrotic tissu, moderate dranage and odor 5: presence of heavy drainag and odor, eschar, and slough, surrounding skin reddened or discolored 6: breaks in skin around primary ulcer, purulent drainige, fould odor, necrotic tissue, and or eschar, may have septic sy. |
|
|
What is Bates-Jensen Wound Assessment Tool ? |
BWAT Formerly the pressure sore status tool (PSST) -13 items rated 1 to 5 scale -describe wound and periwound characteristics -Total scores range from 13-65 (higher scores indicate increased severity -reliable and valid -used in clinic and research setting |
|
|
What is the Pressur Injury Scale for Healing? |
PUSH -3 subscales wound surface area, exudate amound, appearance Total score 8-34 (higher = less severe) -limited research |
|
|
HATT wound assessment |
History Anatomy Tissue type (worst) Touch/view details |
|
|
DIMES treatment |
Debridement Infection/Inflammation Moisture Balance Edge/Environment Supportive Products |
|
|
What is the prognosis for pi healing? |
Very slowly but with appropriate interventions: Category I within 1-3 wks Category II within days to weeks Category III and IV take an average of 8-13 weeks |
|
|
What are the precautions for PT interventions? |
-pi depth can be deceptive -probe regularly -ensure wound care goals and interventions are consistent with pt. overall plan of care |
|
|
When should you request culturing of wound? |
-if it fails to progress in timely manner -if it shows signs/sx of infection |
|
|
When should we assess for osteomyelitis? |
-wounds with exposed bone -deep wounds with purulent or malodorous drainage |
|
|
When should you not debride a pressure wound? |
If it is stable, hard, dry, eschar-covered in ischemic limb |
|
|
What are the categories of support surface technology? |
1: mattresses and mattress overlays 2: specialty mattresses, pressure-reducing foam, alternative air, low air loss 3: air-fluidized beds |
|
|
What needs to be taken into consideration when considering support surface technology? |
-Pt. needs (pressure redistribution, shear reduction, continence, temp, and moisture control) -Pt. mobility (ability to reposiitoin, transfer) -Pt status (deformities, body weight, tissue status, risk for recurrence) *support surfaces are not substitutes for proper skin care, turning, adn repositioning |
|
|
What should the pt. and caregiver be educated on? |
-wound etiology -intervention strategies -risk factor modification -guidelines for pressure injuries |
|
|
What are the therapeutic exercise interventions for pi's? |
Flexibility (minimize contractures) Strengthening (-assist with mobility, transfers, and weight shifts, pelvic floor and abdominal muscle strengthening to assist management of incontinence) Aerobic Exercise (improves cardiovascular endurance for improving mobility and activity) |
|
|
What functional training interventions for pi's? |
-gait training -transfers and bed mobility (emphasize minimizin friction and shear) (protect intact skin and any existing pi) |

