![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
63 Cards in this Set
- Front
- Back
|
What is an acute wound? |
wound induced by surgery or trauma in an otherwise healthy individual -progresses through normal phases of wound healing in predictable time and manner (inflammation, proliferation, maturation & remodeling) |
|
|
What is the inflammation phase? |
Begins at the time of injury Prepares for wound for healing Two activities: Hemostasis (vascular phase)-vasoconstriction, platelet activation & clustering Exudate-leakage of plasma and blood components Scab formation-if wound is small Cellular phase- WBCs movement, phagocytosis of debris Sx: fever, leukocytosis, gen. malaise |
|
|
What is the proliferative phase? |
Begins 2-3 days of injury, lasting, up to 2-3 wks Fibroblasts helps build new tissue to fill the wound space Granulation tissue forms which is the foundation for scar tissue development Collagen synthesis and accumulation continues Adequate nutrition and proper oxygenation are important in this phase |
|
|
What is the remodeling and maturation phase? |
Final stage of healing: begins approx. 3 wks after injury and may last for as long as 6 months (if wound is large) and up to two years for full maturation New collagen tissue continues to be deposited which compresses the blood vessels. (so the scar is usually avascular.) Wounds that heal by second intention take longer to remodel and form a scar smaller than the original wound. |
|
|
What is a chronic wound? |
wound whose progression through the phases of wound healing is prolonged or arrested due to underlying conditions |
|
|
What are the factors affect wound healing? |
-Developmental stage -State of health -Wound characteristics -Local factors -Systemic factors -Inappropriate wound management |
|
|
What are all the factors that need to be approached for wounds? |
Wound characteristics Local factors Systemic factors |
|
|
What are the characteristics that affect rate of wound healing? |
-mechanism of onset -time since onset -wound location -temeprature -wound hydration -necrotic tissue or foreign bodies -infection |
|
|
What are examples of mechanism of onset? |
- surgical wounds -traumatic wounds -wounds with an insidious onset-underlyinig pathology |
|
|
Why do we need to know the time since onset of the wound? |
can assist with predicting healing time in acute wounds |
|
|
What are the types of wounds? |
Incision Contusion Abrasion Laceratioin Puncture Penetrating Avulsion Microbial Chemical Thermal Irradiation |
|
|
What is the cause of an incision? |
cutting or sharp instrucment; wound edges are close approximation and aligned |
|
|
What is the cause of a contusion? |
blunt instrument; usually disrupting skin surface; possible bruising |
|
|
*What is the temperature the wound should be? |
temperature of body 98.6 |
|
|
What is the cause of an abrasion? |
rubbing or scraping epidermal layers |
|
|
What is the cause of a laceration? |
tearing of skin & tissue w/ blunt or irregular instrument |
|
|
What is the cause of a puncture? |
pointed instrument punctureing the skin |
|
|
What is the cause of a penetration? |
FB entering skin at high velocity; fragments possibly scattered throughout tissues |
|
|
What is the cause of an avulsion? |
Tearing a structure from normal anatomic position; possible damage to blood vessels, nerves & other structures |
|
|
What is the cause of microbial wounds? |
secretion of exotoxins or endotoxins |
|
|
What is the cause of chemical wounds? |
toxic agents and substances released from cellular necrosis |
|
|
What is the cause of thermal wounds? |
High or low temperature; cellular necrosis as possible result |
|
|
What is the cause of irradiation wounds? |
UV light or radiation exposure |
|
|
Picture of abrasion wound: |

|
|
|
Picture of thermal wound: |

|
|
|
Picture of thermal wound: |
|
|
|
Picture of contusion wound: |

|
|
|
Picture of laceration wound: |

|
|
|
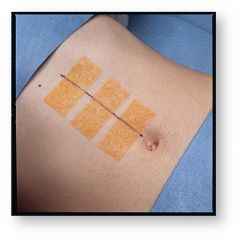
Picture of penetration x 2 wound: |

|
|
|
Picture of puncture wound: |

|
|
|
Picture of avulsion wound: |

|
|
|
Why is the wound location important to know? |
-vascularity of area -wounds over bony prominences-less vascular -presence of epidermal appendages -skin thickness |
|
|
How does the wound shape affect wound healing? |
linear takes less time to close square comes second in time circular longest time to heal *size and depth also affect it |
|
|
What is the importance of wound hydration? |
-Dry wounds open to the air -moist wounds heal better |
|
|
What does necrotic tissue do to a wound? |
promotes infection |
|
|
What does foreign body do for a wound? |
prolongs inflammation |
|
|
Picture of necrotic tissue: |

|
|
|
What are some wound complications? |
-Infextion -Hemmorrhage -Dehiscence and Evisceration (Dehiscence: partial or total disruption of wound layers) (Evisceration: protrusion of viscera through the incisional area) -Fistula formation: abnormal passage from an internal organ to the skin or from one internal organ to another |
|
|
Explain an infected wound: |
-invasion and multiplication of microorganisms in body tissues (colinization is okay) -Culture with >10^5 microbes per g/tissue = infection -signs and sx similar to inflammation but disproportionate to wound |
|
|
What is colinization: |
presence of microbes normal skin microflora, up to 10^3 per g/tissue |
|
|
What things occur and cause an acute wound to become a chronic one? |
-senescent cells -increased number of inflammatory mediators -reduced number of tissue inhibitors of MMPs -reduced or arrested epithelialization -greater bioburden |
|
|
*What is a *Dehiscence? |
partial or total disruption of wound layers |
|
|
*What is a evisceration? |
protrusion of viscera through the incisional area |
|
|
How does circulation affect wound healing? |
Inadequate macrocirculaiton Inadequate microcirculation Sympathetic response: vasoconstriction (methods to improve can be as simple as temp) |
|
|
What are the interventions for impaired macro or microcirculaiton? |
-vascular consult -medical management |
|
|
What are the interventions for cold impaired circulation? |
blankets heat lamps |
|
|
What are the interventions for fear impaired circulation |
explain intervention provide rationale, if pt. can comprehend distraction provide a nonthreatening environment antianxiety medications |
|
|
What are the interventions for pain impaired cirulation? |
explain intervention provide rationale, if pt can comprehend distraction pn. meds accept steady improvements when pt. tolerance precludes complete resolution during a particular session |
|
|
what are the mechanical stresses that can occur in the are of the wound? |
pressure shear frictioin periwound edema tension on wound edges-improper suturing, edema |
|
|
How does age affect wound healing(systemic factors)? |
-Decrease macrophage function, impaired fibroblast function -decrease collagen synthesis and lower cellular turnover occurs, epidermal & dermal atrophy (? decrease vascularity) -slowed immune response, decrease sweat glands, decrease inflammatory response, increased susceptibility to infection, increase comorbidities, decrease pain perception |
|
|
How does inadequate nutrition affect wound healing (systemic factors)? |
Carbs for preferred fuel, but .also need proteins and vitamins (albumen 3.4-5.4 grams per deciliter and prealbumin levels: 16 to 35 mg/dl) |
|
|
How does the person's developmental stage of their skin affect wound healing? |
-infants skin and mucous membranes are easily injured -childs skin becomes increasingly resistant to injury and infection -adolescents skin has enlarged sebaceous glands and increased glandular secretions and continues to about age 50 -older adults: brown spots or liver spots, dry |
|
|
How does a persons stage of health affect wound healing? |
-very thin or obese: susceptible to irritation -fluid loss- loose and flabby -jaundice -eczema and psoriasis |
|
|
What are the comorbitities that affect wound healing? |
DM, COPD, PVD, anemia, immunocompromised (HIV) or transplant pt |
|
|
What are the medications that affect wound healing? |
steroids >30-40 mg/day (impair), chemotherapy?, NSAIDS, all can decrease wound tensile strenght, and non selective COX and delay or cause abnormal bone healing |
|
|
How does the behavior of the person affect wound healing? |
lifestyle alcohol smoking -greater risk for injury -less likely to seek or obtain medical attention |
|
|
How does smoking affect wound healing? |
-decreases tissue perfusion -reduces tissue oxygenation -therefore reducing oxygen tension -delays normal cellular response to wounding -3x increased graft/flap necrosis -3-5 x increased infection rate -possible interventions |
|
|
What are the other factors that affect wound healing? |
age circulation & oxygen Nutritional status Wound condition Health status |
|
|
What are some of the innappropriate wound management (pt. related issues)? |
-home remedies -not following recommended treatment -lack of understanding of information provided -limited financial resources -insufficent caregiver support |
|
|
What are the factors that may affect personal hygiene? |
-culture -socioeconomics class -spiritual practices -developmental level -health state -personal preferences |
|
|
What are the clinician related issued for innappropriate wound mangagment? |
-failure to follow established guidelines-refer when appropriate -failure to properly educate pt -exposure to air or inappropriate dressing -inappropriate use of antiseptics (iodine, hydrogen peroxide, and dakin's-bleach) -overuse of whirl pool |
|
|
*What happens when Suture line repaired how much do we get back? |
80% Not 100% even if it does not dehisence |
|
|
What are the psychological effects of wounds? |
-pain -fear and anxiety -changes in body image (dysmorphia) |

