![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
39 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Function of respiratory |
Gas exchange |
|
|
|
Pulmonary ventilation |
Exchange between the atmosphere and your lungs |
|
|
|
Pulmonary respiration |
Exchange between lungs and blood |
|
|
|
Tissue respiration |
Exchange between Blood and Tissue |
|
|
|
Inhalation exhalation |
Contraction of respiratory muscles |
|
|
|
How do gases exert pressure |
Pressure= force/area, ⬆ volume/⬇ pressure, gases exert pressure thru Collison |
|
|
|
Boyle's Law |
Inverse relationship between volume and pressure of a gas |
|
|
|
Compliance |
Ability of lungs to expand, determined mostly by surface tension of fluid in alveoli ( High compliance= easy to expand) |
|
|
|
Elastic recoil |
Ability to return to shape after being stretched, determined mostly by surface of fluid in alveoli |
|
|
|
Minute ventilation |
Ventilation rate × tidal volume |
|
|
|
Alveolor ventilation |
Ventilation rate × title volume - Dead space (150ml) |
|
|
|
Hyperventilation |
Ventilation above metabolism requirements |
|
|
|
Hypoventilation |
Ventilation below metabolism requirements |
|
|
|
Pulmonary and tissue respiration |
Passive happens by diffusion which requires concentration gradient |
|
|
|
Dalton's law |
Pressure of a gas in a mixture of gases is exerted independently of the other gases total pressure is the sum of the partial pressures. |
|
|
|
Nitrogen, 02, CO2 |
78% 21% .033% ( for gas to diffuse through liquid it has to dissolve in the liquid) |
|
|
|
Henry's law |
Amount of gas that will dissolve in some liquid depends on the partial pressure of the gas. For a gas to dissolve in a liquid it has to collide with liquid. |
|
|
|
Factors that influence rate of diffusion |
1 steepness in concentration gradient 2 surface area 3 coefficient gas liquid temp 4 distance |
|
|
|
Transport of o2 in blood |
1.5% dissolved in plasma 98.5% bound to hemoglobin o2 (g)↔ o2 (aq) O2 (aq)+Hb-h ↔Hb-o2+h^+ |
|
|
|
Factors that influence the affinity(attraction) of Hb for o2 |
Po2, pH, Pco2,BPG [CO2(aq)+Hb↔Hb-CO2] [CO2 (aq)+H2o↔H2CO3↔HCO-3+H^+] ⬆during exercise ⬆high altitude ⬆BPG ⬇Hb affinity for o2 altitude ⬆BPG ⬇Hb affinity for o2 |
|
|
|
Transport of CO2 in blood |
7% dissolved into plasma 23% as carbo Amino compounds 70% as hco3 (bicarbonate) |
|
|
|
Regulation of ventilation: basic rhythm |
Respiratory Center 1. Medullary respiratory Center- dorsal respiratory group➡ communicate with respiratory muscles Ventral respiratory group➡ communicate with abdominal muscles plus internal intercostals for forced exhale Pre botzinger neurons➡ communicate to the drg/ adapt the transition between inhale and exhale |
|
|
|
Modifications to basic rhythm |
Chemoreceptors • Central chemoreceptors➡ located in medulla➡ monitor pH pco2 in CSF Peripheral chemoreceptors➡ located in arotic Arch and carotid sinus➡ monitor pH pco2 po2 (normal stimulus to breathe High pco2 not low po2) |
|
|
|
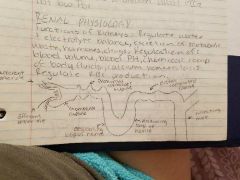
Function of kidneys |
Regulate water and electrolyte balance ,excretion of metabolic wastes, hormones, drugs |
|
|
|
Kidneys regulation |
Blood volume, blood pH, chemical composition of body fluids, calcium homeostasis, regulate red blood cell production |
|
|
|
Kidneys |
|
|
|
|
Glomerular filtration |
Glomerular filtration rate(GFR)= volume of filtrate you farm per minute |
|
|
|
What determines what gets filtered |
The filtration membrane- selection based on size and charge |
|
|
|
What determines how much gets filtered |
BP in glomerulus |
|
|
|
How do kidneys keep GFR constant despite fluctuations in systemic BP |

|
|
|
|
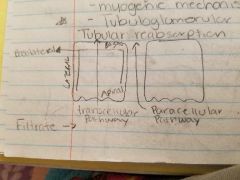
How is resistance of afferent and efferent arteriole regulated( how do we regulate GFR) |
Neural regulation( sympathetic stimulation) Hormonal regulation( epinephrine, Angiotensin II,ANP) Autoregulation- myogenic mechanism - tubuloglomerular feedback (tubular reabsorption) |
|
|
|
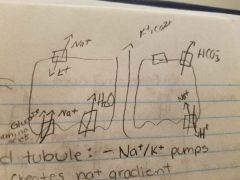
Proximal convoluted tubule |
Na+/K+ pumps in basolateral membrane creates na+ gradient Use gradient to reabsorb glucose and amino acids Water follows by osmosis Paracellular reabsorption of K+, Ca2+ by diffusion Primary active transport is sodium potassium pumps Secondary active transport is using the gradient Reabsorb hco3 by feedback loop |
|
|
|
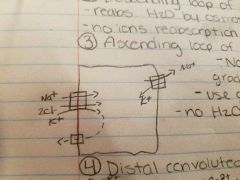
Descending Loop of henle |
Reabsorb H2O by osmosis No ions reabsorbed |
|
|
|
Ascending Loop of henle |
Na+/K+ pumps create Na+ gradient Use gradient to reabsorb Na+/2Cl-/K+ No H2O reabsorbs because no channels |
|
|
|
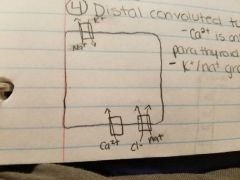
Distal convoluted tubule (hormonal) |
Ca2+ is only in the presence of parathyroid hormone K+/Na+ gradient |
|
|
|
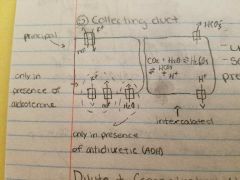
Collecting duct |
Adding new HCO-3 Urinate out the H+ Secrete more H+in presence of aldosteron |
|
|
|
Dilute and concentrated urine production |
Blood➡300mosm/l New filtrate➡300 mosm/l Urine:dilute➡50-100mosm/l Urine:concentrate➡1200mosm/l Dilute urine has no ADH ( deeper into medulla the more concentrated the I.F. will be) |
|
|
|
Why is the concentration of I.F. in medulla so high |
Counter-current multiplication by Loop of henle create high concentration Counter-current exchange by Visa recta allows High concentration to persist |
|
|
|
Acid/base |

|

|

