![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
105 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Pleural pressure & alveolar pressure
a. Pleural pressure b. Value of pleural pressure c. Alveolar pressure d. Value of alveolar pressure |
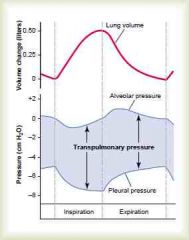
a. The pressure of the fluid in the thin space between the visceral and parietal pleura
(Slightly negative due to elasticity of lung and suction of excess fluid into lymphatic channels) b. -5 (expiration) to -7.5 cm H2O (inspiration) (Guyton) c. Alveolar pressure is the pressure of the air inside the lung alveoli d. 1+ (expiration) to -1 (inspiration) (0 is set to equal atmospheric pressure) (Transpulmonary pressure is the pressure difference between the two. It reflects the elastic forces of the lungs. Called recoil pressure) (Guyton) |
|
|
|
Compliance of the lungs
a. What b. Value c. Depend on |
a. The extent to which the lungs will expand in mL for each cm H2O increse in transpulmonary pressure
b. For both lungs its about 200 mL\cm H2O (For both lungs with thorax its 110 mL\cm H2O) (Takes 10-20 seconds) c. The elastic forces of the lungs <- 1. Elastic forces of the lung tissue itself (elastin, collagen) 2. Elastic forces caused by surface tension of the fluid that lines the inside walls of the alveoli and other lung air spaces (2\3 of elastic strength) (Guyton) |
|
|
|
Surfactant
a. Produced by b. Surfactant is a complex mixture of phospholipids, proteins and ions. What is the most important components (3)? |
a. Type II alveolar epithelial cells
(10% of surface area of alveoli, granular & have lipid inclusions) b. Dipalmitoylphosphatidylcholine, surfactant apoproteins, Ca ions c. (Reduce surface tension up to 10 fold) |
|
|
|
Formula for pressure of alveoli caused by surface tension
|
Pressure = (2 x surface tension)\(radius of alveolus)
(Surfactant: 4 cm H2O, water: 18 cm H2O) (Small premature babies can have alveoli with radii less than one quarter that of an adult, on top of that, surfactant don't begin to develop before 6th-7th month of pregnancy -> cause respiratory distress syndrome of the newborn) (Guyton) |
|
|
|
Work of breathing
a. Can be divided into 3 fractions b. Energy required for respiration during rest c. Energy required for respiration during heavy exercise |
a. The work of inspiration can be divided into three fractions
1. Compliance work 2. Resistance work (That required to overcome the viscosity of the lung and chest wall structures) 3. Airway resistance work b. Up to 5% c. Up to 50% (Guyton) |
|
|
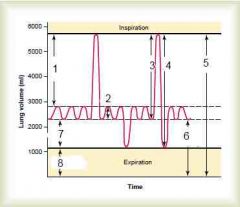
Average for a young adult male
|
(IRV: the extra volume of air that can be inspired over the normal tidal volume - 300mL)
(ERV: The maximum extra volume of air that can be expired by forceful expiration after the end of normal tidal expiration, 1100 mL) (Residual volume: volume remaining after maximal expiration, 1200 mL) (Pulmonary capacity = combinations of two or more pulmonary volumes) (Inspiratory capacity = TV + IRV = 3500 mL) (Functional residual capacity = ERV + RV = 2300 mL) (Vital capacity = IRV + TV + ERV = 4600 mL) (Total lung capacity = IRV + TV + ERV + RV = 5800 mL) (Guyton) |
|
|
|
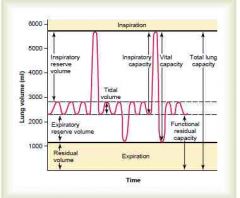
Pulmonary volumes and capacities - in average adult. Definition and value
a. Tidal volume b. Inspiratory reserve volume c. Expiratory reserve volume d. Residual volume e. Pulmonary capacities f. Inspiratory capacity g. Functional residual capacity h. Vital capacity i. Total capacity j. Value in women relative to males |
a. Tidal volume = the volume of air inspired or expired with each normal breath = 500 mL
b. Inspiratory reserve volume = the extra volume of air that can be inspired over and above the normal tidal volume = 3000 mL c. Expiratory reserve volume = The maximum extra volume that can be expired after the end of a normal tidal expiration = 1100 mL d. Residual volume = The volume of air remaining in the lungs after the most forceful expiration = 1200 mL e. Pulmonary capacity is a combination of several lung volumes f. Inspiratory capacity = TV + IRV = 3500 mL g. Functional residual capacity = RV + IRV = 2300 mL h. Vital capacity = IRV + TV + ERV = 4600 mL i. Total lung capacity = IRV + TV + ERV + RV = 5600 mL j. 20-25% less (Also greater in larger & more athletic people) (Guyton) |
|
|
|
Pulmonary volumes and capacities
a. Which cannot be determined by spirometry? b. How are these determined? |
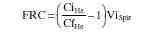
a. All that depend on residual volume
b. Residual volume can be found by helium dilution method (Helium is inspired at the end of a tidal expiration. (FRC = functional residual capacity CiHe = initial concentration of helium in the spirometer CfHe = final concentration of helium in the spirometer Vispir = initial volume of the spirometer) |
|
|
|
Minute respiratory volume
a. How much can the tidal volume increase to? b. How much can the rate increase to? |
a. 4600 mL = vital capacity
b. 40-50\min (-> > 200L\min, 2\3 of this is not sustainable for more than a minute) (Guyton) |
|
|
|
Dead space
a. Anatomical dead space b. Physiologic dead space |
a. The volume of all the space of the respiratory system other than the alveoli
b. Anatomical dead space + alveolar dead space (non-perfused\poorly perfused, non-functional) (In a person with partially funcitonal or nonfunctional alveoli the physiologic dead space may be as high as 10 x the anatomical. In healthy people its about equal) (Guyton) |
|
|
|
Alveolar ventilation formula
|
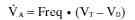
Guyton
|
|
|
|
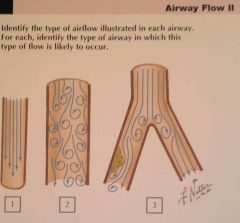
Resistance to airflow in the bronchial tree
a. The greatest amount of resistance to airflow occurs in |
a. Some of the larger bronchioles and bronchi
(Due to their low total cross-sectional area) (Yet in disease states the smaller bronchioles play a greater role. <- Spasm, edema, mucus) (Guyton) |
|
|
|
Parasympathetic nervous reflexes constricting the bronchioles can be elicited by (2)?
|
1. Irritation of the epithelial membrane of the respiratory passageways themselves, initiated by noxious gases, dust (sulfor dioxide, acidic elements), cigarette smoke, or bronchial infection
(Can also cause local non-nervous reactions via mast cells) 2. Microemboli of small pulmonary arteries (Guyton) |
|
|
|
Cough & sneeze reflex
a. Cough reflex - initiated by? which nerve? b. Sneeze reflex - initiated by? which nerve? c. Mechanism? difference between the two reflexes |
a. Light touch (foreign particles) -> carina, larynx (especially), chemical corrosives (sulfur dioxide gas, chlorine gas) -> terminal bronchioles (and even alveoli), vagus nerve
b. Chemical & touch in nasal passageways, trigeminal nerve c. 1. Maximum of air is inspired 2. Epiglottis & vocal folds close (-> cause the pressure to elevate to 100 mmHg) 3. Open suddenly (airflow up to 160 km\t) In the sneeze reflex the uvula depresses, thus forcing the air through the nasal passageways (Guyton) |
|
|
|
Filtration function of the airways
a. Where are most particles > 5 um stopped? b. Where are particles between 1-5 um mostly stopped? c. Fate of particles < 1um |
a. In the nasal passageways by the process of turbulent precipitation (the air passing through the nasal passageways hit many obstructions causing it to change direction & lose momentum), hair, and mucus
(-> cilia -> pharynx -> esophagus) b. Settle in the smaller bronchioles due to gravitational precipitation (Terminal bronchiolar disease in coal miners) c. Diffuse against the walls of the alveoli and adhere to the alveolar fluid or are suspended in the air and expelled by expiration (Ie particles of cigarette smoke) (Adherence to alveoli -> removed by alveolar macrophages, lymphatics. excess can cause growth of fibrous tissue in alveolar septa) (Guyton) |
|
|
|
Bronchial vessels
a. % of cardiac output b. Empty into |
a. 1-2%
b. Pulmonary veins -> left atrium (Thus this deoxygenated air mix with oxygenated air from pulmonary vein and cause the saturation to be less than 100%) (Guyton) |
|
|
|
Pressure in the pulmonary artery
a. Systolic b. Diastolic c. MAP d. Mean pulmonary capillary pressure |
a. 25 mmHg
b. 8 mmHg c. 15 mmHg d. 7 mmHg (Guyton) |
|
|
|
Compliance of pulmonary vascular tree
|
7 mL\mmHg
(= very high, <- large diameter vessels, that are also thin and easily distensible. The consequence of this is that the pulmonary circulation is capable of accommodating the large amount of blood flow (4-7x) that happens during exercise without increasing the blood pressure (and causing edema) excessively) (Guyton) |
|
|
|
Pulmonary vedge pressure
a. What b. Use |
a. Insert a catheter into one of the small branches of the pulmonary artery to measure the pressure
b. Indicative of pressure and changes of pressure in pulmonary capillaries and left atrial (Congestive heart failure) (about 5 mmHg here, left atrial average 2 mmHg (1-5 mmHg), and pulmonary capillary pressure about 7 mmHg.) (In left heart failure the left atrial pressure can rise up to 40-50 mmHg. Above 7-8 mmHg, further increase cause almost equally great increases in pulmonary arterial pressure -> right heart failure. Above 30 mmHg pulmonary edema is likely to develop) (Guyton) |
|
|
|
Blood volume of the lungs
a. How much b. How much can it increase? when? c. How much can it decrease? when? |
a. 450 mL (9%)
b. 2x, ie congestive heart failure, mitral regurgitation, aortic stenosis c. To half, ie forced expiration, compensation to systemic volume contraction (Guyton) |
|
|
|
a. The capillaries in the alveolar walls are distended by the blood pressure inside them, but simultaneously, they are compressed by the alveolar air pressure on their outsides. What happens then when the lung alveolar air pressure become greater than the capillary blood pressure?
b. How big is the difference in hydrostatic pressure in the highest part of the lung and the lowest? |
The capillaries close and there is no blood flow.
b. 23 mmHg (15 mmHg above heart, 8 mmHg below heart) (Ie the apical systolic pressure is only 10 mmHg (25 mmHg at heart level - 15 mmHg hydrostatic pressure difference) (Guyton) |
|
|
|
Zones 1,2,3 of pulmonary blood flow
a. Different zones b. Which zones exist in a healthy upright person? c. Which zones exist in a healthy recumbent person? d. When does zone 1 blood flow occur (2)? e. What happens to the blood flow during exercise? |
a.
1. Zone 1: no blood flow during all portions of the cardiac cycle (alveolar pressure is higher than alveolar capillary pressure during the whole cardiac cycle) 2. Zone 2: Intermittent blood flow (only in systole) 3. Zone 3: Continuous blood flow b. Zone 2 in apices and zone 3 in all the lower areas c. Zone 3 in all of the lung (No part of the lung is more than a couple of centimeters above the heart) d. Breathing against positive air pressure (> 10 mmHg greater than normal), low pulmonary systolic pressure as in hypovolemia e. Apices change to zone 3 (increasing flow 700-800%, only incrase 200-300% in the lower lung since they're not normally blocked during parts of the cardiac cycle) (Guyton) |
|
|
|
Capillary exchange of fluid in the lungs - 4 differences compared to peripheral circulation
|
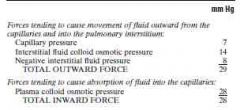
1. The pulmonary capillary pressure is lower (7 vs 17 mmHg)
2. The interstitial fluid pressure is more negative (-8 vs -5 mmHg) 3. Higher interstitial oncotic pressure (The pulmonary capillaries are leakier to plasma proteins) (14 vs < 7 mmHg) 4. The alveolar walls are very thin, and the alveolar epithelium covering the alveolar surfaces is so weak that it can rupture by any positive pressure in the interstitial pressure greater than alveolar air pressure (0 mmHg) (Guyton) |
|
|
|
Pulmonary edema
a. Groups of causes (2) b. Normal pulmonary capillary hydrostatic and oncotic pressure (similar as peripheral) b. Pulmonary edema safety factor |
a.
1. Increased pulmonary capillary pressure <- left-sided heart failure, mitral valve disease 2. Increased leakage <- damage to the pulmonary capillaries <- infections (pneumonia), breathing noxious gases (chlorine gas, sulfur dioxide gas) b. Pulmonary capillary hydrostatic pressure: 7 mmHg Pulmonary capillary oncotic pressure: 28 mmHg c. Pulmonary edema safety factor The pulmonary capillary hydrostatic pressure can rise to pulmonary capillary oncotic pressure (determined experimentally) before significant edema formation begins. This gives a safety factor of 21 mmHg (Compensatory changes in lymphatic drainage in chronic (> 2 weeks) conditions such as mitral valve disease can increase up to 10 fold so the patient can have a pulmonary capillary hydrostatic pressure of up to 45 mmHg without the development of lethal pulmonary edema) (Guyton) |
|
|
|
Henry's law
a. Formula b. Explain |

a. Partial pressure = concentration of dissolved gas\solubility coefficient
b. The solubility coefficient depend on the molecules attraction to water molecules. When molecules are attracted, far more of them can be dissolved without building up excess partial pressure within the solution. (Carbon dioxide is 20x as soluble as oxygen -> the partial pressure of carbon dioxide for a given concentration is less than 1\20 that exerted by oxygen) (Guyton) |
|
|
|
Vapor pressure
a. What? b. Value at 37C? |
a. The partial pressure that the water molecules exert to escape through the surface.
b. 47 mmHg at 37C (Due to random movement of water molecules making them continually escape from the water surface into the gas phase.) (The vapor pressure of 57 mmHg at 37C means that once the gas mixture has become fully humidified (ie via respiratory airways) - that is, once it is in "equilibrium" with the water - the partial pressure of the water vapor in the gas mixture (P H2O) is 47 mmHg) (Guyton) |
|
|
|
Diffusion pressure
a. Formula with explanations of factors b. Two factors depend solely on the gas, which are these, and what are they collectively called? |
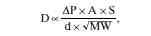
a. Image
D = Diffusion rate deltaP = partial pressure difference between the two ends of the diffusion pathway A = cross-sectional area of the pathway S = Solubility of the gas d = Distance of diffusion MW = Molecular weight of the gas (The velocity of kinetic movement of the molecules is inversely proportional to the square root of MW) b. Molecular weight and solubility of the gas = diffusion coefficient of the gas (Proportional to S\square root of MW) (Guyton) |
|
|
|
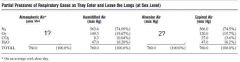
(Guyton)
|
|
|
|
Rate at which alveolar air is renewed by atmospheric air
a. The volume of alveolar air that is replaced by new atmospheric air with each breath is ... of the total? b. Importance? |
a. 1\7 (350 mL\2300 mL: tidal volume-anatomical dead space\functional residual capacity)
b. Prevent sudden changes in gas concentrations in the blood. (Guyton) |
|
|
|
Respiratory unit\lobule
a. Components b. Special characteristic |
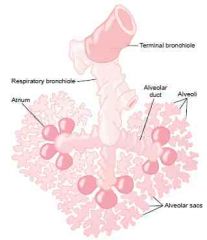
a. Components
1. Respiratory bronchiole 2. Alveolar ducts 3. Alveolar atria 4. Alveoli b. Gas exchange can occur between them. They are collectively called the respiratory or pulmonary membrane. (Guyton) |
|
|
|
Alveoli
a. Number in the two lungs combined? b. Average diameter? |
a. 300 million
b. 0.2 mm (Guyton) |
|
|
|
Respiratory membrane
a. Components (6) |
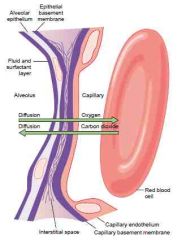
a. Components
1. A layer of fluid lining the alveolus - contains surfactant 2. Alveolar epithelium 3. Alveolar epithelial basement membrane 4. A thin interstitial space 5. Capillary basement membrane (Is in many places fused with the alveolar epithelial basement membrane) 6. Capillary endothelial membrane b. 0.6 um (can be as low as 0.2 um) c. 70 m2 (The average diameter of pulmonary capillaries is 5 um -> the RBC membrane usually touch the capillary wall, so that the gases don't need to diffuse through significant amounts of plasma) (Guyton) |
|
|
|
Factors that affect the rate of gas diffusion through the respiratory membrane (4)
|
1. The thickness of the respiratory membrane
(Normally 0.6 um in average) (Can increase with edema off interstitial space of fibrosis with some pulmonary diseases) 2. The surface area of the respiratory membrane (Emphysema: many of the alveoli coalesce, with dissolution of many alveolar walls. -> The new alveolar chambers are larger, but the total surface area of the respiratory membrane has decreased, can be up to fivefold.) (Affect respiration during rest one when only third remains) 3. The diffusion coefficient (CO2 twice as fast as O2, O2 twice as fast as N2. About) 4. The pressure difference 3. |
|
|
|
Diffusing capacity of the respiratory membrane
a. Definition b. Value for oxygen c. How many times greater can it be under exercise? why? |
a. Diffusing capacity of the respiratory membrane is defined as the volume of a gas that will diffuse through the membrane each minute for a partial pressure difference of 1 mmHg
b. 21 mL\min\mmHg (The mean deltaP for oxygen is 11 mmhg -> 230 mL O2\min) c. > 3 times greater (65 mL\min\mmHg. <- 1. More zone 1 perfusion 2. Increased ventilation-perfusion ratio (Guyton) |
|
|
|
Measurement of diffusing capacity - the carbon monoxide method - principle
|
1. A small amount of CO is inspired and the Pco in the alveoli is measured
2. deltaP = alveolar Pco because hemoglobin binds so fast and avidly with it that its concentration in the circulation can be roughly said to be zero 3. Measure the CO absorbed in a certain period (Can multiply by 1.23 to get the diffusing capacity of oxygen) (Unpractical to measure directly due to the difficulty of measuring the Po2 in the pulmonary capillary blood) |
|
|
|
Ventilation-Perfusion ratio
a. Formula b. Effect of no ventilation on formula c. Effect of no perfusion on formula d. What is a physiologic shunt, and how will it affect the formula? e. what is a physiologic dead space, and how will it affect the formula? |
a. VA(small A)\Q
b. 0 c. Infinity d. The total quantity of shunted blood (bronchial (2% of left atrial input) and via non-ventilated respiratory units) per minute is called the physiologic shunt. Decrease it. (Some degree of shunting in the base of the lung. V\Q is 0.6) e The sum of anatomical dead space (-> terminal bronchiole) and non-perfused alveoli. Cause increased V\Q ratio. (When the physiologic space is great, much of the work of ventilation is wasted because so much of the ventilating air never reaches the blood) (In the top of the lung the V\Q is 2.5 due to decrease of both, both a relatively larger decrease of perfusion. This is improved during exercise) (Guyton) |
|
|
|
Abnormal V\Q in COPD . which two changes occur
|
1. In the areas of the lung where the small bronchioles are obstructed, the distal alveoli is unventilated -> V\Q = close to 0. Serious physiologic dead space.
2. In the areas where the alveolar walls have been mainly destroyed but there is still ventilation there is an increased V\Q. Serious physiologic shunt. (Obstruction -> air trapping -> emphysema (destruction & fusion of alveoli) -> destroy much of the alveoli) (Can combine to reduce the effectiveness of the lung to as little as 1\10) (Guyton) |
|
|
|
Blood values
a. Venous and interstitial pO2 and oxygen saturation b. Arterial pO2 and oxygen saturation c. Intracellular pO2 d. Venous and interstitial pCO2 e. Arterial and alvelar pCO2 f. Intracellular pCO2 |
a. 40 mmHg = 75% O2 saturation
b. 95 mmHg = 97% O2 saturation (not alveolar due to physiologic shunting by bronchial vessels) c. 23 mmHg (5-40 mmHg) (1-3 mmHg is required for full support of the chemical processes that use oxygen) d. 45 mmHg e. 40 mmHg f. 46 mmHg (The big difference in intracellular vs interstitial in CO2 and O2 is due to its solubility coefficient and the potentially long diffusion distance) (Guyton) |
|
|
|
The blood PO2 rises almost to that of the alveolar air by the time the blood has moved a .... of the distance through the capillary, becoming almost 104 mmHg
|
1\3
(Under strenuous exercise the required oxygen can increase 20 fold combined with a increased cardiac output which can reduce the time that the blood remains in the capillary to one half of normal. Yet, because of the great safety factor for diffusion of oxygen through the pulmonary membrane, the blood still becomes almost saturated with oxygen by the time it leaves the pulmonary capillaries.) (Guyton) |
|
|
|
Role of hemoglobin in oxygen transport
a. How many % is carried bound to oxygen? b. What happens to the last percent? |
a. 97%
b. The remaining 3% is transported in the dissolved state in the water of plasma and blood cells (Guyton) |
|
|
|
Draw oxygen-hemoglobin dissociation curve (x?, y?, shape?)
|
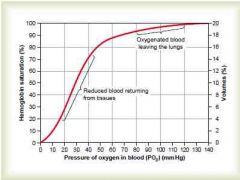
(Guyton)
|
|
|
|
Maximum amount of oxygen that can combine with the hemoglobin of the blood
a. How many mL of oxygen can one gram of hemoglobin bind? b. How many mL of oxygen are transported from the lungs to the tissues by each 100 mL of blood flow during normal conditions= |
a. 1.34 mL
(Actually 1.39 mL, but its reduced due to the presence of ie. methemoglobin) (-> 15g hemoglobin\100 mL -> 20mL O2\100 mL blood = 20 volume percent) (19.4 mL O2\100 mL blood at 97% oxygen saturation, 14.4 mL O2\100 mL blood at 75% oxygen saturation) b. 5 mL O2 (19.4-14.4) (Can be increased to 15 mL O2 during strenuous exercise = 3 fold increase. This plus 6-7x increase in CO gives a 20-fold increase in oxygen transport) (Guyton) |
|
|
|
Utilization coefficient
a. Definition b. Normal value |
a. The percentage of the blood that gives up its oxygen as it passes through the tissue capillaries
b. 25% (Up to 85% in the entire body during strenuous exercise) (Guyton) |
|
|
|
Effect of hemoglobin to buffer the tissue Po2
a. Why is the pO2 of interstitial tissue not higher than 40 mmHg considering the high saturation of hemoglobin as it leaves the capillary bed? b. In which values can hemoglobin buffer the blood? |
a. The hemoglobin normally sets 40 mmHg as an upper limit due to its affinity to oxygen
b. 60-1000 mmHg with only a few mmHg changes in the peripheral tissues (Guyton) |
|
|
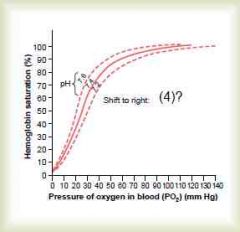
Oxygen-hemooglobin dissociation curve
a. Image b. Bohr effect |
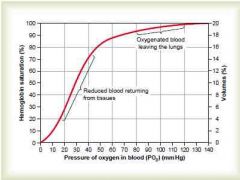
b. The right-shift of the curve due to increased H and pCO2
(The normal BPG in the blood keeps the oxygen-hemoglobin dissociation curve shifted slightly to the right all the time. In hypoxic conditions lasting longer than a few hours, it can increase considerably, releasing O2 at 10 mmHg higher) (Guyton) |
|
|
|
Effect of intracellular PO2 on rate of oxygen usage
a. When the cellular PO2 is more than ..., oxygen availability is no longer a limiting factor in the rats of the chemical reactions. b. What is the rate-limiting factor? |
a. 1 mmHg
b. ADP concentration (Thus the rate of energy expenditure (ATP->ADP) is the rate-limiting factor) (Guyton) |
|
|
|
Transport of oxygen in the dissolved state
a. How much is normally transported in the dissolved state to the tissues by each 100 mL of arterial blood flow? |
a. 0.17 mL O2\100 mL blood flow
(Compared to 5 mL O2\100 mL blood in hemoglobin) (0.29 in arterial, 0.12 in venous) (If a person breathes oxygen at very high alveolar PO2 levels, the amount transported in a dissolved state can become high enough to cause oxygen poisoning) (Guyton) |
|
|
|
What is the hemoglobin affinity to carbon monoxide compared to oxygen?
|
250 times higher
(CO compete equally with oxygen when PCO is 0.4 mmHg. 0.6 mmHg PCO can be lethal.) (the PO2 which measures the dissolved oxygen can still be normal) (Guyton) |
|
|
|
Transport of carbon dioxide in the blood
a. mL transported\100 mL blood flow during normal conditions b. Chemical forms in which carbon dioxide is transported, and its percentage |
a. 4 mL CO2\100 mL blood flow
b. 1. Dissolved state - 7% CO2\100mL blood flow) 2. Bicarbonate - 70% 3. Carbaminohemoglobin - 23% (Guyton) |
|
|
|
Carbonic anhydrase in red blood cells
a. Function b. Pathway for products |
a. CO2 + H2O -> H2CO3 (-> H + HCO3)
b. 1. Most of the H combine with the hemoglobin due to its strong buffering ability. 2. Many of the HCO3 diffuse out through the membrane in exchange for Cl by band 3 (HCO3-Cl exchanger) called Hamburger or chloride shift (increased Cl in RBCs compared to other cells) (= 70% of carbon dioxide transport. Inhibition with azetazolamide can increase interstitial PCO2 to 80 mmHg <- altitude sickness treatment by causing hyperventilation?) (Guyton) |
|
|
|
Haldane effect
a. What b. Mechanism |
a. Binding of oxygen with hemoglobin tends to displace carbon dioxide from the blood
(Quantitatively more important in promoting CO2 transport than is the reverse effect - the Bohr effect in promoting oxygen transport) b. Oxyhemoglobin is a stronger acid -> 1. Acidic hemoglobin has less tendency to form carbaminohemoglobin 2. The increased acidity cause it to release an excess of H -> bind with HCO3 -> H2CO3 -> CO2 + H2O (Almost doubles the amount of carbon dioxide released from the blood in the lungs and approximately doubles the pickup of carbon dioxide in the tissues) (Guyton) |
|
|
|
Respiratory exchange ratio\Respiratory quotient
a. Formula b. For diet exclusive in carbohydrates c. For diet exclusive in fat d. For diet exclusive in protein e. For mixed diet f. How can one determine the proportion of fat and carbohydrates metabolized |
a. R = rate of carbon dioxide output (4 mL CO2\100 mL blood flow)\rate of oxygen uptake (5 mL O2\100 mL blood flow)
b. 1 (When oxygen is metabolized with carbohydrates, one molecule of carbon dioxide is formed for each molecule of oxygen consumed) c. 0.7 d. 0.80 (When oxygen reacts with fats and protein, a significant share of the oxygen metabolized with these foods is required to combine with the excess hydrogen atoms present in their molecules) e. 0.825 f. Use nitrogen excretion to assess protein metabolism and then use a mathematical formula to find the proportion of fat and carbohydrates metabolized. (Almost 1 after a meal, almost 0.7 8-10 hours after a meal, almost 0.7 in untreated diabetes mellitus) (Guyton) |
|
|
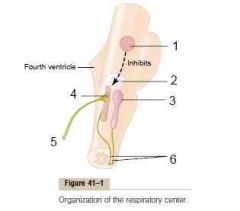
Respiratory center
|
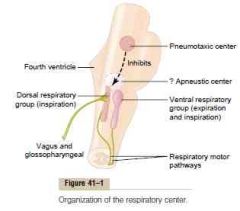
(The respiratory center is composed of several groups of neurons located bilaterally in the medulla oblongata and pons of the brain stem)
(Dorsal respiratory group is located in the dorsal portion of the medulla, and mainly cause inspiration) (Ventral respiratory group is located in the ventrolateral part of the medulla, and mainly cause expiration) (The pneumotaxic center is located dorsally in the the superior portion of the pons, and mainly control rate and depth of breathing) (Guyton) |
|
|
|
Dorsal respiratory group
a. Location b. Function |
a. Extend most of the length of the medulla, most of it is located in the tractus solitarius (afferent nucleus of CN IX, X) and reticular substance of the medulla
(Input to tractus solitarius include: peripheral chemoreceptors, baroreceptors, several types of receptors in the lungs) b. The basic rhythm of respiration (Even if the medulla have been sectioned and the brain stem is transected both above and below) (Emits inspiratory neuronal action potentials -> inspiratory ramp signal) (Guyton) |
|
|
|
Inspiratory ramp signal
a. What b. What qualities regarding it can be regulated |
a. The nervous signal for inspiration begins weakly and increases steadily in a ramp manner for a few seconds and then ceases abruptly
(Produce steady increase in the volume of the lungs instead of inspiratory gasps) b. Controllable qualities 1. Rate of increase of the ramp signal - faster during heavy inspiration (-> fills lungs faster) 2. Limiting point at which the ramp suddenly ceases -> to control the rate (The earlier the ramp ceases, the shorter the duration of inspiration) (Guyton) |
|
|
|
Pneumotaxic center
a. Location b. Function |
a. Dorsally in the nucleus parabrachialis of the upper pons
b. Control the "switch-off" point of the inspiratory ramp -> duration of the filling phase -> rate of respiration It works by limiting inspiration and thus increasing the rate of breathing (Guyton) |
|
|
|
Ventral respiratory group of neurons
a. Location b. Function |
a. Bilaterally anterior and lateral to the dorsal respiratory group in the nucleus ambiguus rostrally and nucleus retroambiguus caudally
b. Functions mainly as an overdrive mechanism when high levels of pulmonary ventilation are required, inactive during normal breathing (Stimulate both inspiration and expiration, especially important in providing the powerful expiratory signals to the abdominal muscles) (Guyton) |
|
|
|
Hering-Breuer inflamation reflex - components
|
Stretch receptors located in the muscular portions of the walls of the bronchi and bronchioles -> vagi -> dorsal respiratory group -> pneumotaxic effect: "switch off" inspiratory ramp (inhibit filling and secondarily incrase respiratory rate)
(Activated when tidal volume is increased three-fold in humans <- probably mechanism to inhibit overinflation not regulate normal breathing) (Guyton) |
|
|
|
Direct chemical control of respiratory center activity by carbon dioxide and hydrogen ions
a. Where is the receptors? b. What is the most important direct stimulus? c. Excitation of carbon dioxide on the respiratory center is great the first hours and declines to 1\5 after 1-2 days. What is the mechanism of this? |
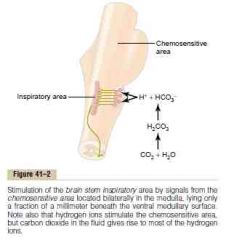
a. In a bilateral chemosensitive area located beneath the ventral medullary surface
b. Hydrogen ions (But hydrogen ions don't easily cross the BBB. CO2 is believed to stimulate this sensors secondarily through hydrogen via reacting with water) c. 1. Renal acid-base regulation 2. Slowly-diffusing HCO3 through the BBB into the CSF which combine and "remove" H (= Effective acute effect, weak chronic effect after a few days adaptation) (Guyton) |
|
|
|
Peripheral chemoreceptor system for control of respiratory activity - role of oxygen in respiratory control
a. How low must PO2 fall before this mechanism become active? b. Location, where is the signal transmitted to c. Role of H and CO2 d. How does hypoxia stimulate these chemoreceptors? |
a. < 70 mmHg
(Most active between 60-30 mmHg) b. Most as carotid bodies -> Hering's nerve->CN IX -> dorsal respiratory area of medulla some aortic bodies in aortic arch -> CN X -> dorsal respiratory area of medulla (Receive its own artery with very high blood flow -> % of oxygen removed is almost zero -> constantly exposed to arterial blood values) c. The central receptors is much more powerful, but the peripheral can respond a lot faster (up to 5x) than the central route (Important during rapid increase in CO2 during exercise?) c. Controversy if it is by the glomus cells which have contact with nerve endings, or by the nerve endings themselves (The glomus cells are highly characteristic glandular-like cells that synapse directly on indirectly with nerve endings) (Guyton) |
|
|
|
Acclimatization - increased tolerability to low atmospheric rpessure of oxygen if it happens gradually, as with mountain climbers
a. Mechanism |
a. After 2-3 days the respiratory center in loses much of its sensitivity to changes in PCO2 and H -> hypoxic stimuli from peripheral chemoreceptors can stimulate a larger increase in ventilation due to loss of inhibitory effect of low PCO2 and H
(Increase in ventilation can be 400-500% compared to 70% without acclimatization) (Guyton) |
|
|
|
J (juxtaposition) receptors
a. Where b. <- c. -> |
a. Sensory nerve endings in the alveolar walls in juxtaposition to the pulmonary capillaries
b. Especially when the pulmonary capillaries become engorged with blood or when pulmonary edema occurs (Like in congestive heart failure) c. Thought to elicit a feeling of dyspnea (Guyton) |
|
|
|
Cheyne-Stokes breathing
a. What b. Mechanism c. Seen in (2) |
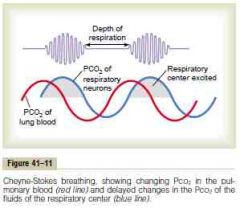
a. Crescendo-descendo periodic breathing, every 40-60 seconds
(Periodic breathing: breathes deeply, breathes slight\don't breathe -> new cycle) b. The basic mechanism is due to lag from pulmonary values of carbon dioxide in reaching the chemosensitive neurons of the respiratory center. (This exist in everyone, but normally its highly "damped" by the large amounts of dissolved and chemically bound carbon dioxide and oxygen in the blood and respiratory center) c. 1. Long delay for transport of blood from the lungs to the brain <- Severe cardiac failure 2. Excessive negative feedback <- brain damage (This type is frequently a prelude to death from brain malfunction) (Guyton) |
|
|
|
Maximum expiratory flow
a. What b. Why? c. Value |
a. The maximum expiratory flow beyond which the flow cannot be increased any more even with greatly increased additional forces.
(Much higher when the lungs are filled with a large volume of air then when they are almost empty) b. Increased pressure for expiration force both air from the alveoli toward the bronchioles and collapse the bronchioles. After a certain point, the increased bronchiolar constriction exceed the pressure generated by the outflow of the alveoli. (Highest in highest lung volume because the bronchi and bronchioles are held open partially by way of elastic pull on their outsides by lung structural elements) c. 400L\min (Guyton) |
|
|
|
Constricted lung diseases
a. Examples (4) b. Effect on maximal expiratory flow c. Effect on residual volume d. Effect on total lung capacity |
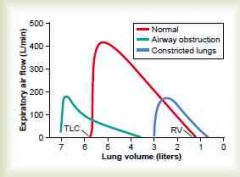
a. Fibrotic disease of the lung itself
1. Tuberculosis 2. Silicosis Diseases that constrict the chest cage 3. Kyphosis 4. Scoliosis b. Decreased (Less TLC and RV -> less maximum expiratory flow) c. Decreased d. Decreased (Guyton) |
|
|
|
Diseases with airway obstruction
a. Examples (2) b. Is inspiration or expiration more difficult? why? c. Effect on maximum expiratory flow d. Effect on residual volume e. Effect on total lung capacity |
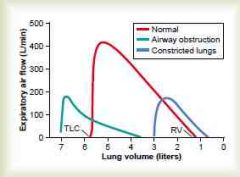
a.
1. Asthma 2. Emphysema (some stages) b. Expire, the closing tendency of the airways is greatly increased by the extra positive pressure required in the chest to cause expiration (The extra negative pleural pressure that occurs during inspiration actually "pulls" the airways open at the same time that it expands the alveoli -> air enter lungs easily and then become trapped) c. Decreased (< obstruction of airway, collapse more easily than normal airways) d. Increased (air trapping) e. Increased (air trapping) (Guyton) |
|
|
|
Forced expiratory vital capacity and forced expiratory volume
a. Forced expiratory vital capacity b. Forced expiratory volume 1 (FEV1) c. FEV1 - normal value d. Used for? |

a. Forced expiratory vital capacity
Vital capacity measured when the patient is exhaling with maximal speed and effort. (IRV+TV+ERV) b. Forced expiratory volume 1(FEV1) Used relative to FVC -> FEV1\FVC c. >80% (Can be <20% in serious airway obstruction) d. Obstructive lung diseases like asthma (Guyton) |
|
|
|
Chronic pulmonary emphysema - pathophysiologic changes (3)
|
1. Chronic infection
(<- inhaling smoke, inactivation of cilia by nicotine, inhibition of alveolar macrophages) 2. Chronic obstruction of the bronchioles (<- infection, excess mucus, inflammatory edema) 3. Air entrapment -> overstretching of alveoli (Combined this can cause destruction of up to 80% of the alveoli) |
|
|
|
Chronic pulmonary emphysema -physiologic effects (4)
|
1. Increased airway resistance
2. Decrease the diffusing capacity 3. Extremely abnormal V\Q ratios - both physiologic shunts (high) and physiologic dead space (low) 4. Pulmonary hypertension -> chronic cor pulmonale (Loss of large portions of the alveolar walls decreases the number of pulmonary capillaries through which blood can pass) (Guyton) |
|
|
|
Pneumonia
a. Definition b. Part of the pathophysiologic changes is consolidation of the affected part - what is this? c. Most common bacterial causative pathogen |
a. Any inflammatory condition of the lung parenchyma in which some or all of the alveoli are filled with exudate and cells
b. Lung segment filled with fluid and cellular debris c. Pneumococci (Guyton) |
|
|
|
Atelectasis (ateles: incomplete, ektasis: extension)
a. Definition b. Causes c. Effect on blood flow |
a. Collapse of the alveoli, which can be localized or affect an entire lung (massive collapse)
b. 1. Airway obstruction caused by mucus or tumor (Entrapped air is absorbed by capillaries within minutes to hours -> collapse or very negative pressure that attract transudate fluid) 2. Lack of surfactant as in hyaline membrane\respiratory distress syndrome of the newborn c. Increased resistance to blood flow <- lung collapse itself, hypoxic vasoconstriction (As a result of this shunting, the overall V\Q is only moderately compromised) (Guyton) |
|
|
|
Hypoxia - causes
a. Inadequate oxygenation of the blood in the lungs due to extrinsic reasons (2) b. Pulmonary disease (4) c. Inadequate oxygen transport to the tissues by the blood (4) d. Inadequate tissue capability of using oxygen (2) e. Other cause? |
a. Inadequate oxygenation of the blood in the lungs due to extrinsic reasons
1. Deficiency of oxygen in the atmosphere 2. Neuromuscular diseases b. Pulmonary disease 1. Hypoventilation <- increased airway resistance 2. Hypoventilation <- decreased pulmonary compliance 3. Diminished respiratory membrane diffusion 4. Abnormal alveolar ventilation-perfusion ratio (physiologic dead space, physiologic shunting) c. Inadequate oxygen transport to the tissues by the blood 1. Anemia 2. Hemoglobinopathies 3. General circulatory deficiency (general, localized (cerebral, coronary) 4. Tissue edema d. Inadequate tissue capability of using oxygen 1. Poisoning of cellular oxidation enzymes (Cyanide inhibit cytochrome oxidase) 2. Diminished cellular metabolic capacity for using oxygen <- vitamin deficiency (beri beri) e. Venous-to-arterial shunts (right-to-left cardiac shunts) (Guyton) |
|
|
|
Cyanosis
a. Cause b. Is cyanosis associated with anemia? c. Is cyanosis associated with polycythemia vera? |
a. Definite cyanosis appears when the arterial blood contains more than 5g of deoxygenated hemoglobin per 100 mL of blood
b. Rarely (Not enough hemoglobin for 5 grams to be deoxygenated in 100 mL of arterial blood) c. Yes (Excess blood cells -> excess Hb) (Guyton) |
|
|
|
Presence of hypercapnia and hypoxia
a. Too little oxygen in the atmosphere, too little hemoglobin b. Diffusion difficulty c. Two general conditions associated with both |
a. Hypoxia
b. Hypoxia, hypercapnia only if very severe (CO2 diffuses 20 times as rapidly as oxygen, and stimulate ventilation at a lower deviation) c. Hypoventilation and general circulatory deficiency |
|
|
|
Hypercapnia - at which alveolar PCO2 levels can ... develop
a. Dyspnea b. Lethargic\semicomatose state c. Death |
a. 60 mmHg PCO2
b. 80 mmHg PCO2 c. 120 mmHg PCO2 (Depress respiration) (Guyton) |
|
|
|
Acclimatization to low PO2 - means (5)
|
1. Increase in pulmonary ventilation
(Arterial chemoreceptors can increase alveolar ventilation 1.65x normal immediately, and up to 5x after several days. The inhibition of hypocapnia and alkalosis diminishes due to renal compensation of alkalosis by increasing bicarbonate excretion) 2. Increased RBC count (Hematocrit can rise to 60 and whole blood hemoglobin concentration can rise to 200g\L after a week. In addition, blood volume increase 20-30%. Combined total body hemoglobin increase >50%) 3. Increased diffusing capacity of the lungs (Normally 21 mL\mm Hg\min, can increase more than three-fold) Increase due to 1 increased pulmonary capillary blood volume -> expand capillaries and increase the surface area for diffusion. 2. Increase in lung air volume -> increase surface area for diffusion 3. Increased pulmonary arterial blood pressure -> increased perfusion. Zone 1 -> Zone 2\3) 4. Increased tissue capillarity\angiogenesis of the peripheral tissues 5. Increased ability of the tissue cells to use oxygen despite low PO2 (Increased mitochondrial and cellular oxidative enzymes) |
|
|
|
Oxygen saturation and alveolar pO2
a. 3000m b. 6000m |
a. 90%, 67 mmHg
(92% and 77 mmHg when acclimatized after several days) b. 73%, 40 mmHg (85%, 54 mmHg, when acclimatized after several days) (Guyton) |
|
|
|
The ceiling when breathing air and when breathing oxygen in an unpressurized airplane
a. A person can stay conscious for short exposures at which level of arterial oxygen saturation b. The ceiling for an aviator in an unpressurized airplane when breathing air c. The ceiling for an aviator in an unpressurized airplane when breathing pure oxygen |
a. 50%
b. 7 000m (23 000 feet) c. 14 000m (47 000 feet) (Guyton) |
|
|
|
Acute effects of hypoxia
a. Above 3700m (12 000 feet) b. Above 5500m (18 000 feet) c. Above 7000m (23 000 feet) |
a.
1. Drowsiness, lassitude, mental and muscle fatigue 2. Decreased mental proficiency (ferdighet) (Mental proficiency is a combination of judgment, memory, and performance of discrete motor movements) 3. Headache, nausea 4. Euphoria b. Twitchings and seizures c. Coma and death (Mental proficiency fall to 50% when staying 4000m for 1 hour, and to 20% after 18 hours) (The top of Mount Everest is 8854m) (Guyton) |
|
|
|
Natural acclimatization of native human beings living at high altitudes
a. Highest populated altitude b. Mechanisms of natural acclimatization |
a. Above 5000m (5338m), and work at 5950m
(Miners living in Peruvian Andes) b. 1. Increased chest size and slight decrease in body mass (high ratio of ventilatory capacity to body mass) 2. Larger heart 3. Increase in delivery of oxygen by the blood to the tissues (Guyton) |
|
|
|
Acute mountain sickness
a. When does it begin? b. Components |
a. From a few hours up to 2 days after ascent.
b. 1. Acute cerebral edema (Caused by hypoxic vasodilation) 2. Acute pulmonary edema (Unknown cause, maybe hypoxic vasoconstriction is higher in some areas, thus shunting the blood to less constricted areas. More and more of the pulmonary blood flow is forced through fewer and fewer still unconstricted pulmonary vessels greatly increasing hydrostaic pressure -> edema) (Reversible in a few hours if given oxygen) (Guyton) |
|
|
|
Chronic mountain sickness - pathophysiological changes
|
1. Excessive increase of hematocrit
2. Excessive increase in pulmonary arterial pressure -> hypertrophy of right ventricle (General hypoxic vasoconstriction of pulmonary vessels) (Guyton) 3. The peripheral arterial pressure begins to fail 4. Congestive heart failure |
|
|
|
Pressures in atria
a. Left atrium b. Right atrium |
a. 5 mmHg
b. 2 mmHg (Netter) |
|
|
|
Describe how changes in lung volume affect pulmonary vascular resistance
|
Increased lung volume first decrease pulmonary vascular resistance due to traction on extra-alveolar vessels, as it increase further it increase pulmonary vascular resistance due to compression on alveolar vessels.
(Netter) |
|
|
|
Chemical and humoral control of pulmonary vascular resistance
a. Identify substances that vasoconstrict pulmonary vessels (4) b. Identify substances that vasodilate pulmonary vessels (4) |
a. Vasoconstrictors
1. Alpha-adrenergic agonists (NE) 2. Thromboxane 3. ATII 4. Endothelin b. Vasodilators 1. Beta-adrenergic agonists 2. Bradykinin (Anaphylactic mediator) 3. Prostacyclin 4. Nitric oxide (Netter) |
|
|
|
Pulmonary acinus
|
The part of the airway consisting of a respiratory bronchiole and all of its branches.
(The respiratory bronchioles are the smallest bronchioles that connect terminal bronchioles to the alveolar ducts) (Primary pulmonary lobule and respiratory lobule are synonyms) (Netter) |
|
|
|
Alveolar sac
|
Terminal dilation of alveolar ducts that give rise to alveoli.
(Stedman) |
|
|
|
Which structures constitute the respiratory zone of the lungs (4)?
|
Structures distal to the terminal bronchiole:
1. Respiratory bronchiole 2. Alveolar ducts 3. Alveolar sacs 4. Alveloli (Netter) |
|
|

1-7?
Which cells increase distally through the airways? Which decrease and are absent in the terminal bronchioles? |

1. Ciliated cell
2. Goblet (mucous) cell 3. Basal cell (stem cell) 4. Brush cell\Type 3 pneumocyte (Brush of rigid apical microvilli and absence of lamellar type secretory granule. Uncertain function. Chemosensor or absorptive?) 5. Kulchitsky cell\Enteroendocrine cell\Argentaffin cell 6. Serous cell 7. Clara cell ( nonciliated, secretory bronchiolar epithelial cells; function as stem cells for repair in the bronchioles and can divide into ciliated or nonciliated bronchiolar cells.) (Ciliated cells and goblet cells are predominant in the trachea and large bronchi. Ciliated cells are predominant in the bronchioles. Clara cells increase distally through the airways, whereas goblet cells and serous cells decrease distally and are absent in the terminal bronchioles) |
|
|
|
Internal intercostal - which part are considered expiratory and which part is considered inspiratory?
|
The interchondral part has a inspiratory function, while the rest has a expiratory function.
(Netter) |
|
|
|
Dalton's law
|
According to Dalton's law, the sum of the partial pressures for gases in a mixture equals the total pressure.
(Netter) |
|
|
|
Alveolar gas equation
a. Give the alveolar gas equation for determining partial pressure of oxygen in alveolar air |
a. PA(alveolar)O2 = PI(inspired)O2 - PACO2\R
R is the respiratory quotient, and is normally 0.825. (The alveolar gas equation can be used in a healthy person to predict PAO2 based on Pa(arterial)CO2 measured during arterial blood gas determination.) (Netter) |
|
|
|
Hysteresis
a. What? b. Why? |
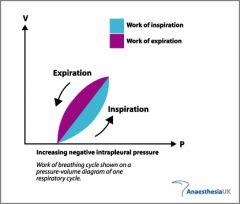
a. Hysteresis is the difference in the pressure-volume curve obtained during inspiration and the curve obtained during expiration.
b. Lung volume associated with any pressure during inspiration is lower than volume at that pressure during expiration, mainly because surface forces must be overcome during inspiration. (Netter) |
|
|
|
What are the factors that account for the initial, rapid adjustment of ventilation with the onset of exercise (2)?
|
1. Activation of motor pathways result in collateral activation of the respiratory center
2. Afferent signals from muscle and joint mechanoceptors result in further activation of respiration (Netter) |
|
|
|
(Netter)
|
|
|

|
(Netter)
|
|
|
|
How many meters of descend into water cause an increase of 1 atmosphere of pressure?
|
10 meters.
(Guyton) |
|
|
|
Boyle's law
|
The inverse relationship of pressure and volume of a gas at constant temperature.
(Guyton) |
|
|
|
Nitrogen narcosis
a. Mechanism b. Symptoms when staying for an hour or more beyond 37 meters c. Symptoms when staying for an hour or more beyond 46 meters d. Symptoms when staying for an hour or more beyond 61 meters e. Symptoms when staying for an hour or more beyond 76 meters |
a. It dissolves in the fatty substances in the neuronal membranes and, because of its physical effect on altering ionic conductance through the membranes, reduces neuronal excitability.
(Same mechanism as gas anesthetics) b. Joviality, carelessness c. Drowsy d. Strength wanes, clumsy movement\loss of coordination e. Almost complete loss of mental proficiency - judgment, coordination, memory (Symptoms resemble alcohol toxicity) (Guyton) |
|
|
|
Acute oxygen poisoning
a. Appear at how many atmospheric pressure units? b. Signs and symptoms when staying at these depths for 30-60 minutes (5) |
a. 4 ATM (30m dive)
b. 1. Seizures followed by coma 2. Nausea and dizziness 3. Muscle twitchings 4. Disorientation 5. Disturbance of vision (Exercise greatly increases the diver's susceptibility to oxygen toxicity) c. Excessive formation of oxygen free radicals (superoxide, hydrogen peroxide) -> exceeds the capability of the cell's enzymes to break them down (catalase, peroxidases, superoxide dismutase) -> free radical damage: polyunsaturated fatty acids (nervous tissue is especially susceptible due to their high lipid content), enzymes ++ (Guyton) |
|
|
|
Chronic oxygen toxicity
a. At how low levels can it develop b. Symptoms (3) c. Mechanism |
a. As low as 1 atm of oxygen for 12 hours
b. 1. Lung passageway congestion 2. Pulmonary edema 3. Atelactasis c. Caused by damage to the lining of the respiratory tract due to the high local PO2 (compared to the hemoglobin buffered PO2 in the rest of the body) -> exceed the cell's capability to break down oxygen free radicals -> free radical damage -> polyunsaturated fatty acids of membrane, enzymes.. (Guyton) |
|
|
|
Decompression sickness\Bends\Compressed air sickness\Caisson disease\Diver's paralysis - mechanism
|
a. The high alveolar PN2 equilibrates with the water of the body in less than an hour and in the fat tissue after several hours (Slow diffusion capacity and slow blood flow to fat tissue)(five times more fat-soluble than water-soluble) -> removal by the reverse process (N2 is not metabolized) takes almost the same time -> nitrogen bubbles develop in fluids (ECF and ICF) after sudden decompression because of the lack of the high pressure outside compressing all the body tissues sufficiently to keep the excess nitrogen gas dissolved -> block progressively larger vessels -> tissue ischemia & infarction
(At 1 atm 1L N2 is dissolved in the body, 2 atm = 2L, 3 atm = 4L..) (Guyton) |
|
|
|
Decompression sickness\Bends\Compressed air sickness\Caisson disease\Diver's paralysis
a. Time for development of symptoms b. Symptoms (3) |
a. can be delayed for minutes to hours
(Sometimes the gases can remain dissolved in the "supersaturated" state for hours before bubbling) b. Nitrogen bubbles develop -> block progressively larger vessels 1. Myalgia and arthralgia of extremities (90%) 2. CNS involvement: dizziness, paralysis, LOC (up to 10%) 3. Pulmonary involvement (the chokes): dyspnea from vessel blockage and consequently edema (Guyton) |
|
|
|
Advantages of using helium instead if nitrogen for deep dives (80-300 meters)(3)
|
1. 1\5 the narcotic effect of nitrogen
2. Low density -> lower airway resistance for breathing 3. Diffuses more rapidly, less dissolve in body tissue (The world record is 318 meters) (Guyton) |
|
|
|
Hyperbaric oxygen treatment - beneficial for (4)
|
1. Decompression sickness\Caisson disease
2. Arterial gas embolism 3. CO poisoning 4. Gas gangrene (Caused by clostridial organisms which grow best under anaerobic conditions and stop growign at PO2 great than 70 mmHg) (Guyton) |
|

