![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
20 Cards in this Set
- Front
- Back
|
- How many people have limb loss - What is the ratio of arm to leg amputations - What is the primary reason for upper limb amputations (75%) / lower limb amputations? |
- 2 mill Americans (2008) - 1:3 - Trauma/ Disease (ex: diabetes, peripheral vascular disease) |
|
|
- What does amputation surgery involve? - What are the primary goals? |
- severing blood vessels and nerves, beveling bones (to prevent bone spurs), suture muscles to bones distally (process called myodesis) - Goals: maintain maximal function of remaining tissue, allow maximal use of prosthesis, fit of prosthesis will be snug and comfortable (for this reason most amputations are on the shaft- easier to fit prosthesis) |
|
|
Surgical Terminology - Trans - AE (also called) - BE (also called) |
- Amputation across the axis of a long bone - Above the elbow (now called Transhumeral) - Below the elbow (now called Transradial) |
|

What are the types of amputations in the arm (9)
|

|
|
|
- Is it easier to use a prosthesis with higher or lower amputations
|
- Lower - more joints and muscles are available for control of residual limb and prostetic. Also Lower requires smaller/lighter/less complex prosthesis
|
|
|
- What are post-surgical complications of amputation (6)
|
- Bone Spurs - shown on x-ray, require surgery - Sensation - Hyperesthesia (super sensitive to touch in area), Neuroma (ball of nerve tissue forms on end of residual limb, adheres to scar tissue), phantom limb sensation, insensate limb (no sensation at point of amputation), high pain levels - Persistent Edema - Skin Complications (require daily massage) |
|
|
- What is a sock and socket with regards to a prosthesis. What are their function?
|
- sock: Worn on residual limb, absorbs perspiration and protects limb from irritation, helps with fit and comfort - Socket - mold of residual limb, component prosthesis attaches too. - Optimizes comfort and fit. |
|
|
- Why is the OT's relationship with the prosthetist important? - What is the process for patients receiving prosthesis |
- Because adjustments may be important during fitting and training - receive preparatory prosthesis first (OT begins training with this), then final one months later |
|
|
Prosthesis Components (UE): - Purpose of Harness |

- Control system - Worn across back and shoulders, or around chest - also secures prosthesis and steel cable attachment |
|
|
Prosthesis Components (UE) - Purpose of Control System |
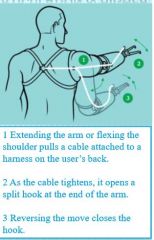
- Operates prosthesis - upper body movements create tension on cable, operating prosthesis - Functions by interacting w/ harness and stainless steel cable |
|
|
Prosthesis Components (UE) - Wrist Unit |

- Connects Terminal Device (TD) to forearm - Unit that pronates and supinates TD |
|
|
Prosthesis Components (UE) - Terminal Device (TD) - Types - What most popular |

- Functions: Grasp, hold and stabilize objects (can be interchangeable) - Cosmetic, activity specific, mechanical (body powered), myo-electric (battery powered), combo of myo-electric and mechanical - Body powered most popular (90%) |
|
|
Myoelectric Prosthesis: - Powered by - Pros (5)/Cons (8) - Method of operations |
- Battery -(Pros) Cosmetically pleasing, no harnessing, can use overhead, minimal effort to control, control similar to normal human control/ (Cons)Less powerful, expensive, cost of maintenance, longer training, fragile, lack of sensory feedback, slow response, heavy - Muscle generates electric potential when contracted, signal is amplified and processed to activate TD |
|
|
Mechanical Prosthesis - Examples - Pros/cons |
- Hook, Hand - Allows better performance of fine motor, gives proprioceptive feedback, lighter, more durable / less cosmetically pleasing |
|
|
- How does a OT with amputee before and after prosthesis is introduced
|
- Before - preparing limb - After - Wearing tolerance, functional use, programming unit, Strengthening (ex: theraband), ADL/IADL training (after prosthesis training is complete) |
|
|
- What can a OT do to help amputee experiencing edema and pain?
|
- Elevation, Massage, circumference measurments, skin hygine (wash daily w/ mild soap, rise thoroughly, pat dry), MD consult regarding skin graft - Teach client to inspect limb (look for ulcers, skin breakdown, ischemia and pressure) - Teach to track limb |
|
|
- How does a OT begin working on ADL/IADL training w/ a client who is using a prosthesis
|
- Start with those they care about most (usually self-care), than dressing, feeding, home management etc. - Train on using adaptive equipment |
|
|
- How can a OT help amputee return to work
|
- Perform work site visit - Assess/evaluate tasks ->can they be modified?? ->do restrictions have to be placed (ex: lifting, climbing, etc) -> does patient need to do a different job/help train for new jobs -> initially patient works part time, to improve endurance. |
|
|
- Hwo can OT help amputee return to driving
|
- Assistive tech - Modify car (ex: ignition, turn signal) - Increase independence |
|
|
- Duration of training -1 Unilateral transradial amputation -2 Unilateral transhumeral amputation -3 Bilateral transradial amputation -4 Bilaterl transhumeral amputation - How should training progress - What is success heavily dependent on? |
1) 8 hrs 2) 12 hrs 3) 15 hrs 4) 20 hrs - Initially training should be 1 hr long, than subsequent sessions may be briefer, than increasing in time as patients strength improves/and prosthesis tolerance improves - Accurate grading of training to patients skill |

