![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
111 Cards in this Set
- Front
- Back
|
What is the most frequently injured joint in athletics?
|
Ankle
|
|
|
What percent of all injuries involve running and jumping?
|
25%
|
|
|
Which ligaments provide varus stability?
|
Lateral ligaments
|
|
|
Which is the weakest and most commonly injured ligament?
|
ATFL
|
|
|
Which ligament prevents excessive anterior displacement of the talus?
|
ATFL
|
|
|
Which ligament is 2.5 times stronger than the ATFL?
|
Calcaneofibular
|
|
|
Which ligament is the strongest and least frequently injured?
|
PTFL
|
|
|
What is the most common mechanism of injury?
|
Plantar flexion and inversion
|
|
|
What percentage of all ankle sprains involve the ATFL?
|
2/3
|
|
|
More than ___% of patients with repeated ankle sprains exhibit weakness of peroneal muscles rather than ligamentous laxity.
|
50
|
|
|
Loss of ___________ from ankle mechanoreceptors may be responsible for increasing risk of re-injury.
|
sensory input
|
|
|
What are the objectives of orthotic management of the ankle?
|
1. prevention or correction of deformity
2. support or immobilization of a body segment 3. assistance or restoration of mobility and function. |
|
|
What are advantages of orthotics over adhesive taping?
|
1. orthotics more cost effective
2. taping requires assistance of another person 3. tape causes skin irritation and breakdown 4. tape loosens significantly shortly after use. |
|
|
What are the two types of orthoses?
|
1. Softshell – made of canvas or neoprene rubber.
2. Semi-rigid – made of orthoplast or other semi-rigid material |
|
|
What are the effects of pneumatic compression on stress fracture healing?
|
• Pneumatic leg brace causes increased hydrostatic and venous pressures resulting in shifting of fluids and electrolytes from the capillary space to the interstitial fluid space.
• Increases bone rate of repair • Unloads the tibia and fibula by stabilizing surrounding musculature permitting the bone to heal. |
|
|
How can orthotic help achilles tendinitis?
|
Orthotics can change the pull on the achilles tendon thereby reducing stress.
|
|
|
How does the achilles tendon affect plantar fasciitis?
|
Decreased flexibility of Achilles tendon results in excessive pronation & overstretch to the plantar fascia.
|
|
|
How do pronation and pes cavus affect plantar fasciitis?
|
Over pronation during stance phase - normal supination not allowed which results in the foot not becoming a “rigid lever” during push off causing excessive stresses to the plantar fascia.
Pes Cavus - may result in plantar fasciitis due to inability to provide shock absorption and dissipate forces. |
|
|
Which joint is judged to be the least congruent in the body?
|
Patellofemoral
|
|
|
What are functions of the patella?
|
1. Anatomic pulley – increases lever arm of quadriceps; improves mechanical advantage of quadriceps
Patellectomy – decreases quad strength by about 20% 2. Absorbs compressive forces imparted to femur 3. Prevents excessive friction on quadriceps tendon. |
|
|
Which muscle controls the dynamic tracking of the patella?
|
Quadriceps femoris
|
|
|
What must occur for there to be proper patellar tracking?
|
There must be a balance between the activity of the vastus medialis oblique and the vastus lateralis.
|
|
|
What is the normal range for Q angle in men and women?
|
Range for males: 10-12°
Range for females: 15-18° |
|
|
What are associated with larger Q angles?
|
1. Increased femoral ante-version
2. Excessive external tibial torsion 3. Genu valgus 4. Excessive lateral forces on patella |
|
|
Maximum contact force occurs at ___ degrees of flexion and approximates 6.5 times body weight.
|
90
|
|
|
Why does the medial aspect of the patella receive more contact?
|
Increased degenerative changes in the cartilage on the medial side.
|
|
|
What are the PFJ reaction forces during dynamic motions such as gait, stair climing, cycling, and deep knee bends?
|
1. During gait – one half of body weight
2. Stair climbing or running – 3.3 times body weight 3. Cycling – 1.5 times body weight 4. Deep knee bends – 7.8 times body weight |
|
|
What percent of military recruits suffer from patellofemoral pain syndrome?
|
20%
|
|
|
What is the etiology of PFPS?
|
1. abnormal stress imposed on the articular surface of the patella as a result of mal-alignment and mal-tracking.
2. High correlation between PFPS and foot alignment – excessive & premature subtalar pronation during gait results in excessive tibial internal rotation; increasing pressure between lateral articular surfaces and PF joint; results in cartilage irritation & degeneration. |
|
|
Subluxation and dislocation of the patella is caused by excessive instability of the ______ pull of the patella.
|
lateral
|
|
|
What is the most common site of patellar tendinitis?
|
Attachment to the inferior patellar pole
|
|
|
What is softening of the articular cartilage that results in irregular surface on the cartilage with fractures and fissures in the articular surface?
|
Chondromalacia Patellae
|
|
|
What is the purpose of a patellar orthotic?
|
The purpose of orthotics is to achieve and maintain optimal patellar tracking so as to prevent abnormal compressive forces and subsequent degenerative changes.
|
|
|
What corrects patellar orientation & controls tracking; reduces pain so as to permit retraining of the VMO?
|
Patellar Taping
|
|
|
What should treatment of patellar tendinitis focus on?
|
Choose knee supports which dissipate stress on the patellar tendon.
|
|
|
What is a velcro strap which pushes against the patellar tendon and facilitates tracking; raises patella from its articular surface?
|
Cho-Pat Strap
|
|
|
What is the use of tape around the patella to reduce forces allowing tendon to heal?
|
McConnell Taping
|
|
|
The ACL provides ____% of passive restraint of anterior movement of tibia on femur
|
95%
|
|
|
The PCL provides ____% of the passive restraint of posterior movement of tibia on femur.
|
86%
|
|
|
The MCL provides ____% restraint of valgus load on the knee.
|
80%
|
|
|
What is the mechanism of injury for the ACL?
|
• Knee slightly flexed
• Foot fixed on ground • Internal rotation of femur combined with valgus stress at knee. |
|
|
What is the objective of function bracing of the ACL?
|
Decrease knee hyperextension tibial rotation and anterior tibial translation.
|
|
|
What are the characteristics of prophylactic knee braces?
|
1. Supplement the stiffness of the knee against injury producing loads.
2. Not interfere with normal function. 3. Not increase risk of injury else-where in lower extremity. 4. Adaptable to various anatomical shapes and sizes. 5. Not harming other players. 6. Cost effective and durable. 7. Documented to prevent injuries. |
|
|
What are characteristics of rehabilitative knee braces?
|
1. Provides accurate control of knee motions avoiding excessive loads on healing tissues.
2. Remains in position without slippage. 3. Adapts to various leg sizes and shapes 4. Adapts for edema and atrophy 5. Comfortable for user. 6. Easily applied and removed 7. Allows brace to be locked at a given joint angle. 8. Durable and economical. |
|
|
Function ACL braces show a ____% decrease in isokinetic knee strength at high speeds.
|
30%
|
|
|
What percent of patients felt the brace helped improve athletic performance?
|
70%
|
|
|
What is the success rate for unloader knee brace for OA?
|
80% success rate
|
|
|
Adults will always go with _______ at the expense of ______.
|
stability
mobility |
|
|
What are indications, advantages, and disadvantages to rigid polypropylene AFOs?
|
Indications:
– Prevent excessive plantarflexion or dorsiflexion during stance. – Controls mediolateral instability at subtalar joint during stance phase. – Facilitates limb clearance in mid-swing. – Positions the foot for appropriate heel initial contact. Advantages: • Lighweight in design • Cosmetically appealing • Can be worn with different footwear. Disadvantages: • Difficulty with sitting to standing due to lack of ankle dorsiflexion • Bending over • Climbing stairs. |
|
|
What are indications, advantages, and disadvantages to bichannel adjustable ankle locking AFOs?
|
Indications:
Advantages: • Adjustments to brace can be easily made to accommodate changes in patient’s walking abilities. • Accommodates to normal plantar flexion which occurs at heelstrike. Disadvantages: • Lacks cosmetic appeal • Wearer un |
|
|
Which type of patient would use a KNFO?
|
• Designed mainly for patients with spinal cord injury, polio, or progressive neurological conditions.
• Patients who have deficits due to CVA or closed head injuries typically do better with an AFO. |
|
|
What are indications for KAFO prescription?
|
1. Inability to stabilize the knee at weight acceptance and through single-limb support phase of gait. This instability is a result of weakness to the quadriceps (mainly) and also weakness of the hip extensors and ankle plantarflexors Patient compensates for this weakness by hyperextending the knee during weight bearing. In this situation, a KAFO can prevent excessive ligamentous strain and minimize joint pain. 2. Impaired or absent proprioception at the knee.
|
|
|
Patient with bilateral KAFO and a swing through crutch assisted gait pattern demonstrate a ____% greater energy cost.
|
500%
|
|
|
What is defines as an appreciable lateral deviation in the normally straight vertical line of the spine; a rotational deformity of the spine and ribs?
|
Scoliosis
|
|
|
During scoliosis the entire thoracic cage takes on an ovoid shape, causing the ribs on the concave side to protrude _______ while the ribs on the opposite side are recessed.
|
anteriorly
|
|
|
What is usually noted in later years of first decade? Curves are always slight and disappear on lying down.
|
Postural Scoliosis
|
|
|
What is usually the result of a leg length discrepancy? Pelvis dips down on the short side
|
Compensatory Scoliosis
|
|
|
What is not true scoliosis; an irritative form caused by pressure on the nerve roots from a herniated disc?
|
Sciatic Scoliosis
|
|
|
Which scoliosis is rare that usually requires psychiatric treatment?
|
Hysterical Scoliosis
|
|
|
What is the most common form of scoliosis (70%)?
|
Idiopathic
|
|
|
How is idiopathic scoliosis classified?
|
Classified by age of onset.
1. Infantile – before 3 years of age 2. Juvenile – age 3 to onset of puberty; usually the age of 10 years 3. Adolescent – from age 10 until maturity |
|
|
What type of brace is used for scoliosis?
|
Milwaukee Brace
|
|
|
What are key characteristic of the Milwaukee Brace?
|
• Can successfully halt progression of curve in 70% of cases.
• Incidence of success rises with addition of exercise program. |
|
|
What are factors for bracing treatment for scoliosis?
|
1. an orthotist who can supply and service the brace.
2. an orthopedic surgeon who will follow the brace treatment 3. a skeletally immature willing patient 4. fully cooperative parents. |
|
|
What are indications for bracing scoliosis?
|
1. any child with progressive spinal curvature.
2. children with paralytic scoliosis supported with brace until they have regain muscle power to maintain straight spine. 3. to maintain spinal alignment until skeletal maturity with subsequent fusion. 4. all structural curves 20 to 40 degrees of skeletally immature adolescents |
|
|
What are goals for exercise programs for those who suffer from scoliosis?
|
1. Develop or enhance the patient’s awareness of his or her posture
2. Augment the function of the orthosis through active exercise while in the brace. 3. Enhance respiratory function and chest mobility. 4. Improve or prevent further loss of ROM of the upper and lower extremities. 5. Enhance proper body mechanics and activities of daily living while wearing the orthosis. |
|
|
What are specific exercises for scoliosis?
|
1. Exercises for muscle function & flexibility of the trunk and pelvis
2. Posterior pelvic tilts in multiple functional positions. 3. Abdominal exercises for upper, lower, and oblique muscle groups. 4. Anterior chest wall stretches 5. Spinal stabilization and stretching into the curve convexity. 6. Hip flexor stretches and strengthening 7. Hamstring stretches and strengthening 8. Iliotibial/tensor fascia latae stretches and strengthening 9. Erector spinae stretches and strengthening. |
|
|
What are functions of orthoses with spinal dysfunction?
|
1. reduce gross spinal motion (limiting bending & twisting of torso)
2. stabilize individual motion segments 3. apply closed chain force systems designed to correct or prevent progression of vertebral column deformities & to stabilize instabilities. 4. protect post surgical interventions. |
|
|
What is the most frequent corset prescribed?
|
Lumbosacral Corset
|
|
|
When are thermoplastic spinal orthoses used?
|
Used when the goal is immobilization of the spine in all 3 planes.
|
|
|
When are thermoplastic spinal orthosies effective?
|
1. instability of spine
2. post-operative care for traumatic thoracic or lumbar fractures. 3. spinal cord injuries 4. spinal fusion |
|
|
For patients with an osteoporotic spinal fracture, what is the main objective of orthoses?
|
Improve quality of life
Reduce pain |
|
|
Cervical soft collars are comfortable and minimally restrict cervical motion, but what is the main purpose?
|
Used primarily as a kinesthetic reminder for patients with mild whiplash injury or neck pain to restrict cervical motions.
|
|
|
Which cervical collar provides more stability than a soft collar and is the most used and best prescribed?
|
Philadelphia
|
|
|
What is used for complete control of cervical and upper thoracic spine in all three planes?
|
Cervical Halo
|
|
|
What are the two main classifications of splints?
|
Articular
Non-articular |
|
|
What is the terminology used when naming splints?
|
Location
Direction |
|
|
What are the purposes of splints?
|
1. Immobilize a structure
2. Mobilize a tissue 3. Restrict an aspect of joint motion |
|
|
The purpose of immobilization is to place a structure in its anatomical or most comfortable ________ position.
|
resting
|
|
|
What is defined as moving or stretching specific soft tissues or joints to create change?
|
Mobilization
|
|
|
How will tissues lengthen during mobilization?
|
The tissues will lengthen due to cell growth and not stretching of the tissues.
|
|
|
When a splint restricts, it also ______ an aspect of joint motion
|
blocks
|
|
|
What are characteristics of static splints?
|
Have a rigid base
Immobilize the joints they traverse |
|
|
Serial static splints are applied to joints, soft tissue, or musculotendinous units they cross and hold them in a _________ position.
|
lengthened
|
|
|
What uses an elastic type force to mobilize specific tissues to achieve increases in ROM?
|
Dynamic Splint
|
|
|
What achieves tissue mobilization by applying low load force to the tissue’s end range in one direction; the force applied is non-elastic?
|
Static Progressive Splint
|
|
|
What are objectives to immobilizing splints?
|
- provide symptom relief
- protect and position edematous structures - aid in maximizing functional use - maintain tissue length - protect healing structures and surgical procedures - provide support and protection for soft tissue healing - maintain and protect reduction of fracture - improve and preserve joint alignment - block and transfer muscle and tendon forces - influence a spastic muscle - prevent possible contracture development |
|
|
What are objectives to mobilizing splints?
|
- remodel long standing, dense, mature scar
- elongate soft tissue contractures, adhesions, and musculotendinous tightness - increase passive joint ROM - realign or maintain joint and ligament profile - substitute for weak or absent motion - maintain reduction of an intraarticular fracture with preservation of joint mobility |
|
|
What are objectives to restriction splinting?
|
- limit motion after nerve injury or repair
- limit motion after tendon injury or repair - limit motion after bone or ligament injury or repair - provide and improve joint stability and alignment - assist in functional use of the hand |
|
|
The arch system of the hand is vital for positioning the hand to allow for normal function related to _______ and _________.
|
grasp
prehension |
|
|
What are characteristics of the proximal transverse arch of the hand?
|
• Carpal tunnel
• Long flexors and median nerve pass en route to the hand. |
|
|
What are characteristics of the distal transverse arch of the hand?
|
Increases the mobility of the peripheral digits allowing for optimal grasping abilities.
|
|
|
What are characteristics of the longitudinal arch of the hand?
|
A disruption of this arch occurs with an ulnar nerve injury resulting in loss of intrinsic muscle function.
|
|
|
Is the position of function (rest) of the hand a long term or short term position?
|
Short term
|
|
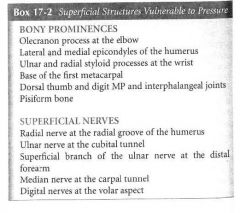
What are superficial structures of the arm that are vulnerable to pressure?
|
|
|
|
What are characteristics of the antideformity position of the hand?
|
• Prevents MP joint contractures
• MP contractures would impair grasping abilities. |
|
|
What may older adults experience with hand orthoses?
|
• May report pain, redness, & irritation over the bony areas
• Use padding or gel • Flare away during the molding process. |
|
|
What should you consider with regard to peripheral nerves when bracing or splinting the hand?
|
• Avoid compression
• Patients may report pain, redness, paresthesias, and numbness in that nerve’s distribution. |
|
|
What should you consider with regard to vascular supply when bracing or splinting the hand?
|
• Avoid compression
• Patients may report throbbing, color changes, temperature changes, and pain. |
|
|
What purposes do splints serve when treating for burns?
|
1. protect fragile wounds or newly grafted burn wounds
2. position joints to maintain achieved ROM 3. as dynamic devices to apply gentle prolonged stretch to increase ROM 4. enhance pressure applied to a scar. |
|
|
When treating burns, should splints replace active exercise?
|
No
|
|
|
What will form is patients are constantly splinted in a particular position?
|
Contracture
|
|
|
Splints should be fabricated with a good fit to reduce _______ and skin breakdown
|
friction
|
|
|
When are splints often donned?
|
Rest
Sleep |
|
|
What can be remolded to adjust the fit to retain gains made after exercise?
|
Thermoplastics
|
|
|
____% of splints contain micro-organisms that may cause infections.
|
50%
|
|
|
When cleaning splints, 1 oz of quaternary ammonia per gallon of water is ____% effective
|
100%
|
|
|
What is a previous name for developmental dysplasia of the hip?
|
Congenital dislocation of the hip
|
|
|
What is the purpose of orthotic management of DDH in the first 6 months of life?
|
Limit extension and adduction
Allow flexion and abduction Initially worn 24/7 |
|
|
What is the hallmark sign of legg-calve-perthes disease?
|
Flattening of the femoral head, often accompanied by avascular necrosis
|
|
|
Legg-Calve-Perthes disease is ____ times more common in boys than girls ages 4-8
|
4
|

