![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
When does injury to a cell/tissue/organ occur?
|
Cellular injury occurs when a stress exceeds the cells' ability to adapt (basic principle). Rather than adapting it will become injured.
|
|
|
The likelihood of injury depends on what? Elaborate a bit.
|
• Type of stress
• Severity (1) If you slowly cut the blood supply (renal artery atherosclerosis) results in atrophy, whereas embolus results in injury. • Type of cell affected (1) Neurons are highly susceptible to ischemic injury whereas skeletal muscle is relatively more resistant. |
|
|
Neurons have the ability to withstand hypoxia for ______ to _______ minutes.
|
3 to 5 minutes
|
|
|
What is hypoxia?
|
Low/inadequate oxygen delivery to tissue.
|
|
|
Hypoxia is a common cause of cellular injury. What are causes of hypoxia?
|
(1) Ischemia
• Decreased blood flow through an organ. • Can occur with block in arterial flow (e.g. atherosclerosis), or a block in a vein (blocking the flow of fresh blood across the vascular bed in the organ) • Shock (2) Hypoxemia (3) Decreased O2-carrying capacity of blood. • Anemia. • CO-poisoning • Methemoglobinemia |
|
|
Provide an example where a block in a vein would cause ischemia in an organ.
|
Budd-Chiari syndrome. Thrombosis of hepatic vein. The most common cause is polycythemia vera. Another cause of BC syndrome would be a patient with lupus that has lupus-anticoagulant (which creates a hypercoagulable state in that patient).
|
|
|
What is shock?
|
Shock is a generalized reduced perfusion of tissue, which results in impaired oxygenation of tissue.
|
|
|
What is hypoxemia? Provide examples.
|
Low partial pressure of O2 in the blood (PaO2 < 60 mm Hg, which would translate roughly to a SaO2 < 90%).
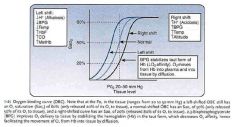
FiO2 (% O2 in the atmosphere) → PAO2 (“squeezes” oxygen into capillaries) → PaO2 (“squeezes” oxygen across RBCs) → SaO2 (O2 “squeezed” into Hb) Examples: • High altitude: FiO2 is decreased. This decreases PaO2 which decreases PaO2 which result in hypoxemia. • Anything that increases PACO2 would decrease PAO2. (1) Hypoventilation is an example. (2) COPD is another. (3) Interstitial fibrosis of the lung. |
|
|
You wanted to measure the saturation of oxygen in Hb in RBCs. How would you do this?
|

Pulse oximetry. Identifiex oxy- and deoxyhemoglobin only. It does not idenfity dyshemoglobins.
|
|
|
O2 content of blood is calculated how?
|
O2 content = (Hb g/dL x 1.34) x SaO2 + PaO2 x 0.003
|
|
|
Provide examples of hypoventilation.
|
Depression of the respiratory center with barbiturates.
|
|
|
An SaO2 of ________ produces cyanosis of skin and mucous membranes.
|
< 80%
|
|
|
In anemia the PaO2 is ____ (normal/abnormally low) and SaO2 would be (normal/abnormally low).
|
normal; normal
None of these variables are affected: FiO2 → PAO2 → PaO2 → SaO2 |
|
|
Give causes of anemia with examples.
|
(a) Decreased production of Mb (e.g.. iron deficiency)
(b) Increased destruction of RBCs (e.g.. hereditary spherocytosis) (c) Decreased production of RBCs (e.g.. aplastic anemia) (d) Increased sequestration of RBCs (e.g., splenomegaly) |
|
|
This is the leading cause of death due to poisoning.
|
CO-poisoning
|
|
|
How would the partial pressure of O2 and saturation of hemoglobin be in the case of carbon monoxide poisoning?
|
CO competes with O2 for binding sites on Hb. Decreases SaO2 without affecting PaO2.
|
|
|
CO and CN inhibits ___________ in the electron transport chain. Poisoning with these poisons are seen in ____.
|
Cytochrome oxidase; house fires
|
|
|
Causes of carbon monoxide poisoning include?
|
(1) Automobile exhaust
(2) Smoke inhalation in house fires (3) Wood stove (vedkomfyr/vedovn) (4) Methylene chloride (paint thinner) (5) Gas heaters |
|
|
From what is cyanide produced in house fires?
|
Combustion of polyurethane products.
|
|
|
What are clinical findings in a person with CO poisoning?
|
(1) Cherry-red discoloration of the skin and blood (can be deceptive)
(2) Early sign of exposure is headache (3) Dyspnea, dizziness (occurs at levels of 20-30%) (4) Hypoxia causes lactic acidosis (5) Seizures and coma ensue. |
|
|
A patient is brought in to the ER after having inhaled smoke from a house fire. You ask the patient if he/she has a headache and they reply "yes". What should you be thinking?
|
Early sign of exposure to carbon monoxide.
|
|
|
What is the main problem in methemoglobinemia?
|
Iron in heme is oxidized to Fe3+.
|
|
|
What happens to the partial pressure of oxygen and saturation of hemoglobin in methemoglobinemia?
|
PaO2 would be normal, SaO2 would be decreased (same as in CO-poisoning)
|
|
|
How is methemoglobin regenerated to normal Hb?
|
NADH is used to transfer electrons to cytochrome B5 and cytochrome b5 reductase transfers (e-) to metHb producing normal Hb.
|
|
|
Methemoglobinemia is classically seen with ______.
|
Oxidant stresses, such as from sulfa and nitrate drugs.
|
|
|
What special group of patients can get a methemoglobinemia?
|
Newborns are particularly at risk for developing methemoglobinemia after oxidant stresses owing to decreased levels of cytochrome b5 reductase until at least 4 months of age.
|
|
|
The classic clinical finding in methemoglobinemia is ______?
|
Chocolate-colored blood (increased concentration of deoxyhemoglobin) and cyanosis.
|
|
|
Clinically evident cyanosis occurs at metHb levels greater than ______.
|
1.5 g/dL
|
|
|
The treatment of methemoglobinemia is ______________.
|
IV Methylene blue. Helps reduce Fe3+ back to Fe2+.
|
|
|
How would CO and metHb poisoning occur on an oxygen binding curve?
|
|
|
|
Describe the consequences of hypoxic cell injury.
|
1° consequence is decreased ATP, everything else is secondary to that.
• Na+-K+ ATPase is affected, causing cellular swelling. • Ca++ pump is affected. Increased Ca++ in the cytosol is the "point of no return" for the cell, causing activation of many enzymes. • Switch to anaerobic glycolysis. Lactic acid production. Denatures structural and enzymatic proteins. |
|
|
If you had to summarize cellular injury in two words, it would be _______________. What would be the consequence on histology for cells in the proximal renal tubule?
|
cellular swelling
Microvilli would be effaced or lost. |
|
|
Cellular swelling would lead to what?
|
(1) Loss of microvilli
(2) Membrane blebbing (membrane "pulls away" from cytoskeleton in certain spots) (3) Swelling of RER. Would cause ribosomes to detach. Decreased protein synthesis. |
|
|
The hallmark of irreversible injury is __________.
|
membrane damage
|
|
|
What membranes are affected in irreversible injury to cells?
|
(1) Plasma membrane
(2) Inner mitochondrial membrane (3) Lysosomal membrane |
|
|
Agent such as ________ and ________ damage the inner mitochondrial membrane.
|
alcohol; salicylates
|
|
|
What is the action of uncouplers?
|
Energy used for synthesizing ATP is used to generate heat. Protons bypass complex 5 in the ETC.
|
|
|
Provide an example of a natural uncoupler.
|
Thermogenin in the brown fat of newborns. Thermogenin is useful for stabilizing body temperature in newborns.
|
|
|
What is a watershed area?
|
An area between the terminal branches of major arterial blood supplies, and these areas do not have overlapping blood supply.
|
|
|
Provide examples of watershed areas.
|
• Area between the distribution of the anterior and middle cerebral arteries.
• Area between the distribution ofthe superior aiul inferior mesenteric arteries (i.e. splenic flexure) |
|
|
Provide some examples of tissues/cells that are susceptible to hypoxic injury.
|
• Subendocardial tissue
• Neurons in cortex, layers 3, 5 and 6. • Purkinje cells in the cerebellum. • Hepatocytes around the central vein • Renal cortex, the straight portion of proximal tubule (highly metabolically active) • Renal medulla, the Na-K-2Cl cotransport in the thick ascending limb is susceptible to hypoxia. |
|
|
Low ATP causes ________ and _________ to accumulate in the cell, causing activation of the enzyme ___________.
|
citrate; AMP; phosphofructokinase
|
|
|
Without ATP, the Na/K-ATPases and sarcoplasmic reticulum __________ fail, leading to increased Na+ and _____ and increased intramitochondrial ________. Failure of sarcoplasmic reticulum to resequester ____ leads to cessation of contraction within ischemic zones of myocardium.
|
Ca+-ATPase; Ca++; Ca++
|

