![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
129 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Limbic system |
Controls emotional aspects of behaviour Role is memory storage/recall - related to dementia |
|
|
|
Dementia |
Cognitive decline Not a normal part of aging Short term memory loss, emotional stability, confusion Due to loss/destruction of neurons - usually caused by Alzheimer's |
|
|
|
What can cause dementia? |
Alzheimer's Cerebro-vascular disease CJD Drugs |
|
|
|
Alzheimer's |
Form of dementia If you can't find any cause Generalized atrophy and degeneration of neurons Age is greatest risk |
|
|
|
Proteins wound up together in neurons |
Neurofibrillary tangles Pathological cause for Alzheimer's |
|
|
|
Large proteins that can't be broken down Different from neurofibrillary tangles Outside of cells Accumulates and forms plaques |
Neuritic plaques Pathological cause of Alzheimer's |
|
|
|
Pathology for Alzheimer's |
Cortex shrinks Ventricles dilate Progresses over 5-20 yrs |
|
|
|
3 stages of dementia |
Early Middle End |
|
|
|
Early dementia |
Hardest to diagnose Forgetfulness Communication difficulties Mood changes Requires minimal assistance |
|
|
|
Middle dementia |
Memory declines Progressive cognitive impairments Assistance with daily living Behaviour change Starting to lose ability to recognize people |
|
|
|
End stage dementia |
Unable to communicate Requires total care Chronic debilitation |
|
|
|
What is usually the official cause of death for dementia sufferers? |
Bronchopneumonia due to chronic debilitation |
|
|
|
Pancreas |
Produces "juice" that aids digestion Soft gland, posterior to stomach Tail reaches spleen Made of aoini and pancreatic islets Instrumental in diabetes |
|
|
|
Glucose |
Cells require this to make ATP Nerve cells can't make or store glucose Therefore needs it from the blood Skeletal, fat, and liver cells can store glucose but need insulin to help facilitate |
|
|
|
Which tissues do not require insulin for glucose delivery? |
Brain, peripheral nerves, cardiac muscles and smooth muscles of the arteries |
|
|
|
Hypoglycemia |
Lack of glucose from the blood |
|
|
|
Hyperglycemia |
Too much glucose which can cause dysfunction and death |
|
|
|
Insulin |
Produced by beta cells in pancreatic islets See a spike in insulin after eating |
|
|
|
When does diabetes develop (3)? |
1. No insulin is produced 2. Not enough insulin is produced 3. Insulin resistance |
|
|
|
Diabetes Mellitus |
"going through" & "honey sweet" Sweet tasting urine Group of disorders |
|
|
|
Type 1 diabetes |
Genetic Complete lack of insulin because beta cells are destroyed by immune system Hyperglycemia |
|
|
|
Type 2 diabetes |
Cast majority of cases 60-80% insulin resistance High body glucose -} release more insulin -} decreased call response -} more insulin -} body cells respond Will cause death of insulin-producing cells and fatigue |
|
|
|
Functions of the digestive system (2) |
1. Digestion 2. Absorption |
|
|
|
Peristalsis |
Motion of indegistive food in alimentary canal |
|
|
|
Organs involved in diesgestion (3) |
Liver Gull bladder Pancreas |
|
|
|
Liver |
Triangular, reddish-brown In the right upper quadrant 4 lobes (usually all doing the same thing) |
|
|
|
Functions of the liver (5) |
Protection Synthesis Storage Billiruben metabolism Bile production |
|
|
|
Liver failure: protection (4 characteristics) |
-Hepatic portal vein drains nutrient rich venous blood from GI tract through liver -Hepatocytes detoxify drugs, alcohol, pollutants, poisons -Hepatocytes arranged into lobules -Hepatic macrophages remove bacteria and debris from blood |
|
|
|
Liver failure: storage |
Stores vitamins Amino acids (the ones we can't produce) Iron Lipids Glycerin |
|
|
|
Liver failure: Bilirubin metabolism |
- damaged RBCs broken down by liver and spleen - hemoglobin breaks down - liver transfers bilirubin to bile, excretes bile to small intestines - bilirubin eventually turns brown, which makes poop brown |
|
|
|
Liver failure: synthesis |
Hepatocytes produce variety of essential substances and waste - plasma, proteins - amino acids, cholesterol, fats - bile - urea (protein metabolism) |
|
|
|
Hepatitis A (transmission) |
Viral hep Fecal-oral transmission Contaminated water, food, milk, shellfish Incubation period, 1 month |
|
|
|
Hep B and C |
Aka serum hep Transmission through body fluids Avg. 2-6 month incubation period More severe Liver becomes larger and edematous Cell injury and necrosis |
|
|
|
Cirrhosis |
Permanent change to the structure of the liver - chronic, irreversible, inflammatory |
|
|
|
Manifestations of hepatitis |
Mild, flu-like symptoms Joint aches, low fever, nausea, fatigue, abdominal discomfort Tender liver, skin rash, jaundice |
|
|
|
Hepatitis - prognosis |
Hep A - recovery in 6 wks with little long term side effects Hep B + C - recovery in 8-10 wks - more likely to be a carrier - be chronic, or progress to cirrhosis or cancer |
|
|
|
Cirrhosis - pathogenesis (4 stages) |
1. Fat accumulates in cells 2. Bands of fibrous tissue from around lobules 3. Disorganized regenerative nodules form 4. Obstructed blood and bile flow |
|
|
|
Manifestations of cirrhosis |
Is due to portal hypertension or liver failure |
|
|
|
Function of urinary system |
Excretes water Controls water, electrolyte, and acid balance Regulates blood pressure by secreting remin (?) Secrets erythropoietin (stimulates RBC) |
|
|
|
Organs in urinary system |
Kidney Ureter - passage between kidneys and bladder Bladder Urethra |
|
|
|
Kidney - cortex |
Superficially outside |
|
|
|
Kidney - medulla |
Deeper layer, darker, made of renal pyramid |
|
|
|
Kidney - nephron |
In cortex, long tail extends down renal pyramid sending urine inwards - the basic functional unit of the kidney - 1 mill per person per kidney |
|
|
|
Afferent arteriole |
Blood supply for the kidneys |
|
|
|
Kidneys - Glomerulus |
Capillary bed in ball shape No gas exchange happens here |
|
|
|
Kidney - peritubular capillary |
Drains away to renal vein and back to heart |
|
|
|
Kidney - Tubules |
Capsules that surround the glomerulus and captures any fluid that escapes - Bowman's capsule/glomerular capsule |
|
|
|
Urine formation (3) |
3 processes: 1. Filtration 2. Reabsorption 3. Secretion |
|
|
|
Urine - filtration |
- Bowman's capsule surrounds glomerulus - Blood comes in afferent arteriole - Fluids and dissolved substances move through glomerular - membrane to Bowman's capsule - driven by blood pressure - throwing stuff out based on size - energy efficient |
|
|
|
Potocytes |
Attach to outside of capillary |
|
|
|
Glomerular filtration rate (GRR) |
Fluid is filtered every 125ml/min 180L/day |
|
|
|
Urine - reabsorption |
Between peritube capillaries and internal structure Return of useful substances to the blood Water, glucose, amino acids, sodium, potassium 99% is reabsorbed |
|
|
|
Urine - secretion |
Movements of substances from blood to peritubular capillaries to the nephron tubules - hydrogen, kreotene, hormones, drugs, etc. - throw out more junk |
|
|
|
Minor calyx |
Urine secretion Collect urine from nephron ducts Point of triangle shape Drains into renal pelvis Into ureter Stretch receptors are sensitive to filling in bladder Sends signals to brain |
|
|
|
2 types of nephron-related disease |
Glomerular disorders Eg. Glometonephritis
Tubular disorders Eg. Pyleonophritis |
|
|
|
Acute pyelonephritis |
Infections of renal pelvis, calyces, medulla Fecal-based like e. Coli Usually through ureters but can enter from blood Affects one or both kidneys |
|
|
|
Manifestations of Acute pyelonephritis |
Renal inflammation, edema Infiltration of WBCs Purulent urine May lead to abscess and necrosis Healing - scarring of tubules |
|
|
|
Chronic Pyelonephritis |
Even more scarring, recurrent auto-immune response to infection Progresses to kidney failure |
|
|
|
Glomerular disorders |
From infections, toxins, immune responses Proteinuria, decreased GFR Low urine output Edema, hypertension, higher blood volume, increasing blood pressure |
|
|
|
Acute glomerulonephritis |
Inflammation of glomeruli Usually after fighting strep infection |
|
|
|
Acute post-strep |
- Abrupt onset 7-10 days after - Bits of strep get stuck in the infiltration system membrane - Attracts neutrophils and macrophages - Will damage membrane - Bowman's capsule leaks when it's not supposed to -Fibrin (a clothing factor) doesn't clot properly and reduces urine - blood and protein in pee Lowered GFR Hypertension Edema in eyes, ascites Usually resolvable without serious issue |
|
|
|
Chronic post-strep |
Just add scar tissue Means reduced function and potential failure |
|
|
|
Acute Renal Failure (ARF) |
- Sudden drop in kidney function - Often tubular necrosis - Change to tubes themselves - Ischemia - nephrotoxic agents |
|
|
|
Nephrotoxia |
Kidney poisoning Heavy metals Organic solvents Antifreeze Antibiotics and pesticides |
|
|
|
What causes ischemia in acute renal failure? |
Hypovolemia (not enough blood) |
|
|
|
Chronic renal failure (CRF) |
Progressive and irreversible from loss of nephrons Chronic glomerulonephritis Chronic ischemia (leads to atrophy) |
|
|
|
3 types ages of renal failure |
- Based on percent of remaining kidney function - must lose 75% to show symptoms - will filter 15ml/min in end-stage - may require dialysis - fluid in brain |
|
|
|
Normal flora |
Usually in large intestines More bacteria cells than human cells Produce vitamins Maintain water balance Help fight pathogens |
|
|
|
Pathogens |
Organisms that cause disease Normal flora are opportunistic pathogens Could cause disease if they end up where they are not supposed to be E. Coli Strep |
|
|
|
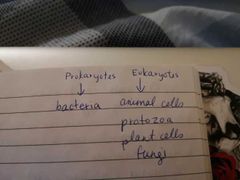
Types of microorganisms |

|
|
|
|
Bacteria |
Cellular - unicellular Prokaryotes Free-living (don't need a host) Have a cell wall Some have a slime wall Some contain toxins Reproduce very rapidly |
|
|
|
3 main shapes of bacteria |
Bacilli - pill Cocci - circular (ie. Strep) Spiral - syphillis |
|
|
|
Viruses |
Acellular Simple structure Capsid DNA Requires living cell host - won't replicate but may remain viable for hours or days Usually tissue specific |
|
|
|
Prions |
Protein particle Altered form of a normal host protein Not broken down by enzymes Progressively greater damage to neuron Transmissible neurodegenerative disease HCHO doesn't work Aerosolization is major transmission |
|
|
|
Example of prion |
CJD Slow progression Non-inflammatory Neuronal degeneration Loss of coordination, dementia, death |
|
|
|
Infection |
When a microbe produces in body tissue Step 1: transmission |
|
|
|
Types of transmission (4) |
Direct - touching a lesion Indirect - involves intermediary eg. food Droplet Vector - insect or animal transmission |
|
|
|
Fomite |
Inanimate object that carries organisms |
|
|
|
Pneumonia |
Inflammation of lung tissue Usually caused by bacteria 8th leading cause of death |
|
|
|
How to classify pneumonia (3) |
Infectious agent Distribution (lobar, broncho-) Source (community v. Hospital) |
|
|
|
Bacterial pneumonia |
Alveolar inflammation - fluid in alveoli from response Most common in strep pneumonia Onset depends on person's health 2 types of distribution: bronchial and lobar |
|
|
|
Bronchopneumonia |
Bronchial infected first Spreads to adjacent alveoli Patches of inflammation throughout lungs Commonly in the chronic or terminally ill |
|
|
|
Lobar pneumonia |
Single lobe fills with exudate Consolidation Little residual damage Healthy people fight it off with antibiotics In compromised, exudate builds up Breathing affected Sepsis or death |
|
|
|
Consolidation |
Large areas fill with exudate Accumulation of fluid, cells, tissue, or other material in alveoli Attracts neutrophils into airways Displaces air |
|
|
|
Viral pneumonia |
Atypical but happens in 50% of cases No fluid buildup or neutrophils Virus invades alveolar epithelium Diffuse and bilateral |
|
|
|
TB |
Chronic bacterial infection caused by mycrobacterium TB (one specific type) Affects those with decreased resistance from malnutrition and decreased immune response Droplet |
|
|
|
Aerobic bacteria - TB |
Needs oxygen in order to grow efficiently Has an extra thick slime layer and therefore more resistant Constant ongoing response to try to isolate bacteria Cause lesions can tubercles (granules) |
|
|
|
TB - what happens to tubercles? |
Centres grow and become Cassius necrosis s Scar tissue forms around and calcifiesisolated bacilliLesion is now a ghon focus isolated bacilli Lesion is now a ghon focus |
|
|
|
What is a ghon complex - TB |
If TB affects lymphnodes as well ghon focus |
|
|
|
When can TB become reactive? (2) |
1. Immune system impaired 2. Live bacilli escape to bronchi |
|
|
|
What is different about secondary TB? |
Lymphocytes jump in for secondary immune response Faster with more necrosis Widespread destruction of lungs Cavitation Localized in lung apex Bleeding may happen |
|
|
|
Flu |
Acute upper respiratory tract infection from virus Indirectly or droplet |
|
|
|
Influenza type A |
Affects proteins type H & N Can insect multiple species |
|
|
|
Influenza types B & C |
Only infects humans Milder, like a cold |
|
|
|
Flu pathogenesis |
Virus targets cells lining respiratory tract Replicates until cell destroyed Cellular injury and immune response Very fast reaction |
|
|
|
Sepsis |
Life-threatening complication of infection From any infection Incidents is rising |
|
|
|
4 stages of sepsis |
SIRS Sepsis Severe sepsis Septic shock |
|
|
|
SIRS |
Systemic inflammatory response syndrome |
|
|
|
Sepsis |
SIRS + infection |
|
|
|
Severe sepsis |
Sepsis + organ damage |
|
|
|
Shock |
Sepsis + hypertension Not enough blood 50% mortality rate |
|
|
|
Opioid |
Painkillers Body build up a tolerance |
|
|
|
Fentanyl |
Potent version of morphine (10x) Used to bump potency of other drugs like heroin Difficult to detect So little is needed Acts directly on brain stem Inhibits respiratory centers in brain stem |
|
|
|
2 types of head injury |
Penetrating Blunt |
|
|
|
Cerebral concussion |
No obvious evidence of brain damage Temporary loss of consciousness Vomiting Headaches Amnesia Increased risk of chronic traumatic encephalopathy |
|
|
|
Contusions |
Bruising of brain Rupture of small vessels near surface Limb paralysis and decreased level of consciousness |
|
|
|
Coup |
On side where impact happened |
|
|
|
Contrecoup |
Rebound - head trauma |
|
|
|
3 types of intercranial hemmorhage |
1. Epidural hematoma 2. Subdural hematoma 3. Subarachnoid hematoma Where hematoma= blood pocket |
|
|
|
3 types of intercranial hemmorhage |
1. Epidural hematoma 2. Subdural hematoma 3. Subarachnoid hematoma Where hematoma= blood pocket |
|
|
|
Layers of brain covering |
Scalp Meninges Brain |
|
|
|
Dura Mater |
Thick mother Superficial most layer |
|
|
|
Arachnoid Mater |
Spidey A gap between this layer and the brain Gap= subarachnoid space |
|
|
|
Pia mater |
Most inner most layer Follows contour of the brain |
|
|
|
Epidural hematoma |
Between skull and Dura Mater Collection of blood that won't even be touching the brain Lack of consciousness sure to increased pressure on the brain |
|
|
|
Subdural hematoma |
Between Dura Mater and arachnoid Mater Tearing of bridging veins These drain to sinus Bleeding is slower and limited in volume Chronic or acute symptoms - if chronic, symptoms are non-specific, dementia in elderly Common in very young and very old |
|
|
|
Subarachnoid hematoma |
Between arachnoid and pia mater Blood vessels on surface of brain Or ruptured aneurysm |
|
|
|
Flail chest |
A type of thoracic trauma Rib fractures Paradoxical motion of the chest |
|
|
|
Accumulations in pleural space |
In membrane lining Thoracic cavity wall sticks to the lungs and fixes them to the wall Can be: Blood Air Exudate Water Pus |
|
|
|
Pneumothroax |
Any Gas in pleural space Very painful because of lung recoil Can be from penetrating chest wound or spontaneous |
|
|
|
Types of pneumothorax (2) |
Open - rupture of lung lining itself During sleep, rest, or exercise Tension - mediastinal shift putting pressure on heart |
|
|
|
Cirrhosis manifestations (4) |
1. Portal hypertension - pressure causes hemmorhoids and esophageal varices 2. Liver failure - 80-90% of liver is destroyed |
|
|
|
What happens during portal hypertension? (5) |
Esophageal varices Hemmorhoids Caput medusae - varicose veins around intestine Ascites Splenomegaly - enlarges spleen |
|
|
|
Portal circuit |
Connects two capillary beds Like from intestines/stomach to liver |
|
|
|
What happens during liver failure? (6) |
80-90% of liver is destroyed Decreased albumin Decreased clotting factors - bruising Decreased hormone metabolism Spider veins Jaundice Toxicity in brain |
|
|
|
Pancreatic change in type 2 diabetes |
Non-specific Fat deposits Enlargement Progressive decrease in weight |
|
|
|
Complications of diabetes (2) |
Ketoacidosis - insulin deficiency - increased fat metabolism Hypoglycemia- insulin shock 90% of type 1 cases |
|
|
|
Diabetes - chronic complications (2) |
Microvascular disease - retinopathy, damage to capillaries, neuropathy , kidney damage Macro vascular disease like atherosclerosis Peripheral vascular disease - gangrene Neuropathies - nerve damage |
|
|
|
Synergism |
Lethal drugs become more potent with combo |
|

