![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
58 Cards in this Set
- Front
- Back
|
A "sleep" dose of thiopentone in a healthy adult is likely to
result in A. a fall in peripheral resistance followed by a rise in cardiac output B. a fall in cardiac output followed by a rise in peripheral resistance C. a fall in peripheral vascular resistance followed by a fall in cardiac output D. a rise in peripheral peripheral resistance followed by a rise in vascular resistance followed by a fall in cardiac output E. a fall in cardiac output followed by a fall in peripheral vascular resistance |
C
Miller p. 785: “The hemodynamic changes produced by barbiturates have been studied in healthy subjects and patients with heart disease. The primary cardiovascular effect of barbiturate induction is peripheral vasodilation resulting in pooling of blood in the venous system.A decrease in contractility is another effect and is related to reduced availability of calcium to myofibrils. In addition, the heart rate is increased. Mechanisms for the decrease in cardiac output include (1) direct negative inotropic action, (2) decreased ventricular filling because of increased capacitance, and (3) transiently decreased sympathetic outflow from the CNS. The increase in heart rate (10% to 36%) that accompanies thiopental administration probably results from baroreceptor-mediated sympathetic reflex stimulation of the heart in response to the drop in output and pressure. Thiopental produces dose-related negative inotropic effects that appear to result from a decrease in calcium influx into the cells with a resultant diminished amount of calcium at sarcolemma sites. The cardiac index is unchanged or reduced, and mean arterial pressure is maintained or slightly reduce“ |
|
|
Norpethidine toxicity
A. is only seen if renal function is abnormal B. develops because the half-life of norpethidine is twice that of pethidine C. is not seen unless treatment is prolonged D. requires doses of pethidine in excess of 1.2 g per day E. may manifest early as anxiety and mood changes |
E
A – False – NOT only (ie young / elderly) B – false – norpethidine has twice proconvulsive properties of pethidine Half life of Pethidine is 5 hrs, vs norpethidine of 15hrs (up to 30hrs in renal failure) C – False – use recommended for less than 24 – 36rhs D – False – 800mg/24hrs http://www.medsafe.govt.nz/profs/Datasheet/p/Pethidineinj.htm “Clinical experience suggests that patients with normal renal function receiving more than 1000 mg/24hrs pethidine are at particular risk of developing pethidine associated neurotoxicity (PAN). Patients receiving over 800 mg/24hrs pethidine should usually be monitored for early signs of norpethidine toxicity (see Warnings).” E - True - norpethidine has analgesic properties (half as potent as analgesic) and is proconvulsant, thus can get seizures in renal failure - Normeperidine elimination t½ = 15hrs (<35hrs in renal failure). It is half as potent as an analgesic & produces CNS stimulation. Toxicity can occur with prolonged PCA’s & renal failure myoclonus, seizures, & delirium (confusion, hallucinations). |
|
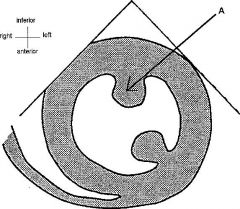
The diagram below represents a transgastric short axis view
of the heart obtained using transoesphageal echocardiography. The structure labelled A is the A. anterolateral papillary muscle B. non-coronary leaflet of the aortic valve C. posterior mitral valve commissure D. posterolateral papillary muscle E. posteromedial papillary muscle |
E
|
|
|
Plasma clearance of non-depolarising muscle relaxants in
pregnant patients (when compared with matched non-pregnant patients) is A. reduced because the distribution half-life is prolonged due to the increased circulating blood volume in late pregnancy B. reduced because the elimination half-life is prolonged due to delayed hepatic and renal clearance brought about by hormonal changes in pregnancy C. increased because the distribution half-life is shortened due to changes in cardiac output in pregnancy D. increased because the elimination half-life is shortened due to increased hepatic and renal clearance brought about by hormonal changes in pregnancy E. increased because the distribution half-life is shortened due to the placental transfer of the relaxant to fetal and placental tissue |
D
Clinical Pharmacokinetics of Neuromuscular Relaxants in Pregnancy Clinical Pharmacokinetics, Volume 34, Number 6, June 1998 , pp. 483-496(14) “Despite an increased in bodyweight, plasma volume by 45% and blood volume by 35% that might influence the volume of distribution of polar drugs, the apparent volume of distribution at steady state (V), volume of distribution (Vd) and the apparent volume of the central compartment (Vc) of atracurium, vecuronium and pancuronium are unchanged during pregnancy. With an elimination that is independent of renal, hepatic and enzymatic functions, the clearance of atracurium is also unchanged. This is corroborated by an unchanged clinical duration of atracurium during pregnancy. The clearance of pancuronium is increased by 27% during caesarean section. This may be explained by the increased glomerular filtration rate reported in pregnant women. The clinical duration of vecuronium in term and postpartum women is twice that reported in nonpregnant women. On the other hand, an increase in the clearance clearance of vecuronium during cesarean sections has been reported.” |
|
|
The best predictor of poor outcome for a peri-operative
ulnar nerve injury is A. a delay in symptom onset to more than 48 hours post-operatively B. association with anaesthesia lasting more than 2 hours C. association with a brachial plexus block D. presence of bilateral injury E. presence of mixed sensory and motor deficit |
E
• A=False Miler 6th ed.pg. 1155 - this occurs in about 9% of cases • B=False • C=False. - mainly associated with GA rather than regional anaesthesia • D=False • E=True - Miller 6th ed. Pg. 1155 - Only 35% of patients with a mixed sensory and motor deficit recovered completely in 1 year |
|
|
Brain stem anaesthesia following retrobulbar block
A. is NOT associated with contralateral amaurosis B. has an incidence of approximately 1 in 2000 blocks C. becomes clinically apparent within 2 to 15 minutes D. usually takes 4 to 6 hours to resolve E. is associated with increased auditory acuity |
C
Symptoms and signs of brain stem anaesthesia Symptoms and signs range from drowsiness, lightheadness, confusion, loss of verbal contact, to cranial nerve palsies, convulsions, respiratory depression or respiratory arrest, and even cardiac arrest. The onset of symptoms is within 10 minutes of the LA injection and the respiratory depression and cardiovascular events may require assisted ventilation and cardiopulmonary resuscitation. Symptoms and signs may last for up to two to three hours incidence approximately 1 in 200 blocks |
|
|
In HIV infected patients
A. a CD4 count of 200 - 400 ce11s.m1-1 is typical B. toxoplasmosis is often a presenting feature C. cardiomyopathy is a recognised complication D. regional anaesthesia in obstetrics is contraindicated E. an epidural blood patch should NOT be used to treat a post-dural puncture headache |
C
From CEACCP article: Anaesthesia and critical care for patients with HIV infection • A – False. CD4 counts in uninfected adults - A normal CD4 count in a man without HIV infection will be approximately 400 to 1200 cells per cubic millimetre of blood, and 500 to 1600 in women. CD4 count in HIV infection - CD4 count is a marker of likely disease progression. Initially in HIV infection there is a sharp drop in the CD4 count and then the count levels off to around 500-600 cells • B – False. This is an opportunistic infection - AIDS defining illnesss. • C – True. ‘Myocarditis, progressing to dilated cardiomyopathy, is common and may be caused by infection with Cryptococcus, coxsackie B virus, CMV, Aspergillus species as well as lymphoma and HIV itself.’ • D – False - 'regional anaesthesia is not contraindicated' • E – False. ' Epidural blood patch for PDPH appears to be safe but other analgesic techniques should be tried first.' and “Despite early concerns that central nervous system involvement would be accelerated in human immunodeficiency virus (HIV)–infected patients receiving a blood patch, there is no evidence that this is the case, and EBP is not contraindicated in these patients” Fleisher: Evidence Based Practice of Anesthesiology, 2nd ed. “If required to treat a post–dural puncture headache, an epidural blood patch may also be performed in an HIV-infected patient” Stoelting: Basics of Anesthesia, 5th ed. “Blood patches have been safely performed in HIV-positive patients. HIV crosses the blood–brain barrier and infects the CNS early in the clinical course. EBP is unlikely to introduce HIV into the CNS” Longneckers Anaethesiology Chpt 45 Tom DJ, Gulevich SJ, et al: Epidural blood patch in the HIV-positive patient. Review of clinical experience. Anesthesiology 1992; 76:943-947. – 6 patients with HIV who received EBP without sequelae |
|
|
Block of the maxillary nerve in the pterygo-palatine fossa
provides ipsilateral analgesia of the A. hard palate B. nasal septum C. posterior part of the lateral wall of the nose D. upper incisor teeth E. upper molar teeth |
E
From Miller: “The mandibular and maxillary nerves, two divisions of the trigeminal nerve, can be blocked through the same needle entry site. The maxillary nerve (i.e., second division) is blocked as it exits the skull through the foramen rotundum and crosses the pterygopalatine or infratemporal fossa between the skull and the upper jaw. The nerve terminates as the infraorbital nerve as it exits through the infraorbital foramen, where it can also be anesthetized. The coronoid notch of the mandible is located, and with the patient's mouth closed, a 22-gauge, 8-cm needle is inserted at the inferior edge of the coronoid notch perpendicular to the skin entry site. The needle contacts the lateral pterygoid plate at a depth of about 5 cm. It is then withdrawn and redirected anteriorly and superiorly to walk off the plate and is subsequently advanced approximately 0.5 cm into the pterygopalatine fossa. Between 3 and 5 mL of local anesthetic solution produces anesthesia of the upper jaw and skin of the lower eyelid, cheek, and upper lip.” |
|
The following is a view obtained at direct larngoscopy.
According to the classification of Cormack-Lehane, this view would be classed as grade A. 1 B. 2 C. 3 D. 4 E. 5 |

B
|
|
|
In a patient in the sitting position during posterior fossa
craniotomy, the following findings would support a diagnosis of venous air embolism (PAP = pulmonary artery pressure, EtCO2 = end-tidal CO2, PaCO2 = arterial partial pressure CO2, CVP = central venous pressure) A. ↓PAP, ↓ETCO2, ↑PaCO2, ↓CVP B. ↓PAP, ↑ETCO2, ↓PaCO2, ↓CVP C. ↑PAP, ↓ETCO2, ↑PaCO2, ↑CVP D. ↑PAP, ↑ETCO2, ↓PaCO2, ↑CVP E. ↑PAP, ↓ETCO2, ↓PaCO2, ↑CVP |
C
From CEACCP “Gas embolism in anaesthesia”: “End-tidal CO2 falls as a consequence of an increase in physiological deadspace and intrapulmonary shunting… In 25% of patients, the CVP is elevated and the pulmonary artery pressure rises in 50%. Arterial blood gases may reveal hypoxaemia and, less commonly, hypercarbia |
|
|
In a rotameter the
A. bobbin spins inside a tube that has parallel sides B. flow is laminar at high flow rates C. height of the bobbin is proportional to the pressure drop across the bobbin D. pressure drop across the bobbin is constant at varying flows E. resistance increases with increasing gas flow |
D
• A – False. Tapered. • B – False. Turbulent at high flow rates. • C – False. • D – True. • E – False. Resistance decreases |
|
|
The maximum disturbance of prothrombin time following
liver resection usually occurs postoperatively A. on days 1 and 2 B. on days 3 and 4 C. on days 4 and 5 D. on days 6 and 7 E. at an unpredictable time |
A
Postoperative Changes in Prothrombin Time following Hepatic Resection: Implications for Perioperative Analgesia. Anaesth Intensive Care. 2006 Aug;34(4):438-43 "This study demonstrates that maximal disturbances in the PT occur on the first and second postoperative days." |
|
|
Intra-ocular pressure is increased by
A. head-up (reverse Trendelenburg) position B. hypothermia C. metabolic acidosis D. miosis E. respiratory acidosis |
E
A. False. Reverse Trendelenburg will decrease IOP. B. False. Reduces IOP by reduction in production of aqueous. C. False. Changes of pH due to metabolic acidosis and alkalosis have opposite effects on IOP compared to corresponding respiratory pH changes. D. False. Miosis decreases IOP. E. True. Increases CO2. |
|
|
When a circle absorption system is in use with an
intubated 70 kg adult patient, rebreathing of expired gas becomes practically negligible if A. a fresh gas flow rate of greater than 9 litres per minute is used B. intermittent positive pressure ventilation (IPPV) is used, rather than spontaneous ventilation C. the carbon dioxide absorbent is fresh and has an intergranular space of at least one litre D. the minute volume is greater than 9 litres E. the fresh gas flow enters the circle circuit on the absorber side of the inspiratory valve |
A
From The Anesthesia Gas Machine: "A fresh gas flow of 8-10 L/min creates a semi-open system, with essentially no rebreathing, since the amount of fresh gas is sufficient to dilute any exhaled carbon dioxide to very low levels (and send it to the scavenging system)." |
|
|
Reversed splitting of the 2nd heart sound is caused by
A. acute pulmonary embolism B. atrial septal defect (ASD) C. complete left bundle branch block (LBBB) D. severe mitral regurgitation E. pulmonary hypertension |
C
Wiki: Split during expiration: Reverse splitting indicates pathology. Aortic stenosis, hypertrophic cardiomyopathy, left bundle branch block (LBBB), and a ventricular pacemaker could all cause a reverse splitting of the second heart sound |
|
|
A six-week-old baby is booked for elective right inguinal
hernia repair. An appropriate fasting time is A. 2 hours for breast milk B. 4 hours for formula milk C. 5 hours for breast and formula milk D. 6 hours for solids E. 8 hours for solids and 4 hours for all fluids |
B
RCH Fasting guidelines • Children less than 6 months of age: Please plan for the last breast feed to finish no later than 3 Hours before anaesthesia. Please plan for a formula or cow's milk feed to finish no later than 4 Hours before anaesthesia. • All other patients: Please do not give milk drinks, food, lollies or chewing gum for 6 Hours before anaesthesia. Please offer clear fluids up to 2 Hours before anaesthesia NOTE: this is different to the ANZCA day surgery guidelines: • limited solid food may be taken up to six hours prior to anaesthesia and clear fluids totalling not more than 200 mls per hour may be taken up to two hours prior to anaesthesia. • Children over six weeks of age, limited solid food and formula milk may be given up to six hours, breast milk may be given up to four hours and clear fluids up to two hours prior to anaesthesia. • For infants under six weeks, formula or breast milk may be given up to four hours and clear fluids up to two hours prior to anaesthesia. |
|
|
Following a left sided pneumonectomy, a left intercostal
drain is placed and connected to an underwater drainage system. In the postoperative period A. a leakage of air is expected from the drain B. the patient should be nursed in the right lateral decubitus position C. the underwater seal drain should be left on continuous free drainage D. the underwater seal drain should be left on continuous free drainage, and connected to wall suction for 5 minutes every hour E. the underwater seal drain should remain clamped and be released for a short period every hour |
E
• A - false - not always • B – true - Events that increase intrapleural pressure in the nonsurgical (ventilated) hemithorax or that decrease intrapleural pressure in the surgical (empty) hemithorax may predispose the patient to cardiac herniation. Positioning the patient so that the empty hemithorax is in a dependent position allows the heart to be pulled by gravity into the empty hemithorax • C – False – Thoracic anaesthesia, Dr Paul Forrest, Uni of Sydney: “Following pneumonectomy, a single drain is placed which should be clamped and intermittently unclamped, this drain must not be on suction as cardiac herniation may occur” • D – maybe – only for first 24 hrs • E – As above |
|
|
Relative contra-indications to mediastinoscopy include
A. cervical spondylosis B. emphysema C. mediastinal lymphadenopathy D. poor left ventricular function E. superior vena cava syndrome |
E
CEACCP 2007: “Contraindications to Mediastinoscopy: Previous mediastinoscopy is a relatively strong contraindication to a repeat procedure because scar tissue eliminates the plane of dissection. Superior vena cava (SVC) syndrome increases the risk of bleeding from distended veins and is a relative contraindication. Other relative contraindications include severe tracheal deviation, cerebrovascular disease, severe cervical spine disease with limited neck extension, previous chest radiotherapy, and thoracic aortic aneurysm.” |
|
|
Consider the following blood gases. Normal ranges are in
brackets. ph PaCO2 7.28 36 Bicarbonate 18 mmo1.1-1 (18 - 25) Base excess -7 mmo1.1-1 (-4 - +3) Na + 142 mmo1.1-1 (135 - 145) Cl- 112 mmo1.1-1 (98- 110) These blood gases are consistent with A. acute renal failure B. diabetic ketoacidosis C. ethylene glycol overdose D. intraoperative infusion of 6 litres of normal saline E. salicylate overdose |
D
Normal Anion Gap Metabolic Acidosis with slight respiratory compensation Anion gap = Na+K-Cl-HCO3 = 142-112-18 = 12 (normal gap 8-16) All the rest are high AG causes |
|
|
A 70-year-old diabetic requires forefoot amputation. You
wish to block the most peripheral nerves possible to provide complete anaesthesia for this procedure. Nerves which you would need to block include the A. medial and lateral plantar B. sciatic and saphenous C. sural and deep peroneal D. superficial and deep peroneal E. tibial and common peroneal |
B
Everything sensory below the knee is supplied by the sciatic nerve, EXCEPT medial foot which is supplied by saphenous nerve (branch of femoral nerve). |
|
|
Analgesic requirements during labour are reduced by each
of the following EXCEPT A. acupressure B. acupuncture C. hypnosis D. one-to-one support by a midwife E. transcutaneous electrical nerve stimulation (TENS) |
Both A and E seem true
From ANZCA Pain book: • A – “The efficacy of acupressure, aromatherapy, audio analgesia, relaxation or massage has not been established” • B and C – “Acupuncture decreased the need for pain relief (RR 0.7; CI 0.49 to 1.0) and women taught self-hypnosis had reduced pharmacological requirements, a slight decrease in need for epidural analgesia (RR 0.30, CI 0.22 to 0.40), and increased satisfaction compared with controls” • D – “Continuous or one-to-one support by a midwife or trained layperson during labour reduced analgesic use, operative delivery and dissatisfaction, especially if the support person was not a member of the hospital staff, was present from early labour, or if an epidural analgesia service was not available” • E – “TENS reduced reports of severe pain during labour, but a consistent reduction in pain scores or in requirements for other analgesia could not be confirmed” |
|
|
A six-year-old boy requires return to theatre for arrest of
post-tonsillectomy haemorrhage. When anaesthetising for this procedure it is important to A. avoid sedative premedication prior to induction B. avoid volatile anaesthetic agents C. have duplicate suction apparatus and endotracheal tubes available D. use an uncuffed endotracheal tube in this age group E. use a rapid sequence induction |
C
CCEAP article "Before induction, in addition to the standard equipment, a selection of laryngoscope blades, smaller than expected tracheal tubes, and two suction catheters should be immediately available" |
|
|
In preparation for a posterior-lateral incision for a
thoracotomy, a patient is placed in the left lateral decubitus position. In this position the A. axillary roll is placed under the chest to aid surgical exposure B. dependant leg should be extended and the superior leg flexed C. neck should be extended to allow access to the airway D. radial nerve is the most commonly injured nerve E. right brachial plexus is at risk of injury if the right arm is flexed at the shoulder to more than 90° |
E
• A. False. "An axillary roll is placed to minimize the risk of brachial plexus injury” - Congress of neurosurgeons • B. False. Other way around • C. False. • D. false, Frequently damaged nerves include the branches of the brachial plexus and the ulnar and common peroneal nerves. The radial nerve is damaged infrequently" From Radial nerve injury after general anaesthesia in the lateral decubitus position* Anaesthesia 2005 60 (6), 602–604. • E. True – mainly correct - > 90 degrees abduction leads to increased risk |
|
|
A 21-year-old female is admitted following a motor vehicle
accident, while returning from a nightclub. She is known to have been taking moderate doses of 3,4 methylenedioxymethamphetamine (MDMA or ecstasy). The clinical feature LEAST likely to be secondary to the MDMA use is A. hyponatraemia B. hypotension C. pneumothorax D. sweating E. tachycardia |
B
BJA Article: http://bja.oxfordjournals.org/cgi/content/full/96/6/678?ck=nck#TBL5 Table 2 Minor clinical symptoms and signs seen with MDMA Tachycardia Elevated mood Hypertension Confusion Mydriasis Ataxia Dry mouth Nystagmus Sweating Bruxism (jaw clenching) |
|
|
The following investigation results are consistent with a
diagnosis of acute Addisonian crisis EXCEPT A. calcium 2.5 mmo1.1-1 B. glucose 12 mmo1.1-1 C. potassium 6.1 mmo1.1-1 D. sodium 125 mmo1.1-1 E. urea 15 mmo1.1-1 |
B
Should be hypo, not hyperglycaemia eMedicine: • The most prominent findings are hyponatremia, hyperkalemia, and a mild non–anion-gap metabolic acidosis due to the loss of the sodium-retaining and potassium and hydrogen ion-secreting action of aldosterone. • Urinary and sweat sodium also may be elevated. • The most consistent finding is elevated blood urea nitrogen (BUN) and creatinine due to the hypovolemia, a decreased glomerular filtration rate, and a decreased renal plasma flow. • Hypercalcemia, the cause of which is not well understood, may be present in a small percentage of patients. However, hypocalcemia could occur in patients with Addison disease accompanied by idiopathic hypoparathyroidism. • Hypoglycemia may be present in fasted patients, or it may occur spontaneously. It is caused by the increased peripheral utilization of glucose and increased insulin sensitivity. It is more prominent in children and in patients with secondary adrenocortical insufficiency. • Liver function tests may reveal a glucocorticoid-responsive liver dysfunction. |
|
|
A 30-year-old man presents to the emergency department
following a high speed motor vehicle accident. His blood pressure is 70/50 mmHg with a strongly positive FAST (focussed abdominal sonography for trauma). His chest X¬ray shows a widened mediastinum. The most appropriate method to assess the widened mediastinum in this patient is A. aortogram B. CT angiogram of the chest C. repeat chest X-ray D. intraoperative TOE (transoesophageal echocardiography) E. transthoracic echocardiography |
D
A-C certainly wrong in this unstable patient. Needs to go to OT anyway and TOE probably better than TTE |
|
|
A 40-year-old man with Marfan's syndrome is to undergo
thoraco-abdominal aortic reconstruction for chronic aortic dissection. An intrathecal catheter is inserted. The purpose for this is to A. allow drainage of cerebrospinal fluid (CSF) B. allow intrathecal administration of metabolic substrates C. allow intrathecal administration of neuroprotective drugs D. cool the spinal cord E. facilitate spinal cord function monitoring |
A
|
|
|
An otherwise well 65-year-old male is having a total hip
replacement under a general anaesthetic consisting of sevoflurane, nitrous oxide and fentanyl. His blood pressure has been stable at 130/70. Prior to the surgeon commencing femoral reaming and cementing, you should A. administer 5000 units of unfractionated heparin B. administer corticosteroids C. discontinue nitrous oxide D. induce moderate hypotension E. use vasopressors to elevate the blood pressure |
C
Bone cement implantation syndrome (BCIS): • is characterized by a number of clinical features that may include hypoxia, hypotension, cardiac arrhythmias, increased pulmonary vascular resistance (PVR), and cardiac arrest. • It is most commonly associated with, but is not restricted to, hip arthroplasty • Pathophysiology: Not fully understood – though to be release into the circulation of MMA cement monomer during cementation. More recent research has investigated the role of emboli formed during cementing and prosthesis insertion BJA – Bone cement implantation syndrome. 2009 • A – “Heparin is known to clear lipaemic serum by stimulating lipase activity and has been advocated for treatment of FES. However, the evidence for heparin treatment in FES is contradictory [85, 86]. If increases in FFAs are an important part of the pathogenesis of FES, then activation of lipase is a potentially dangerous therapeutic intervention. Furthermore, the risk of bleeding, even with low-dose heparin, cannot be ignored in patients with multiple injuries." (Mellor and Soni, Fat Embolism Review Article, Anaesthesia, 2001, 56, pages 145-154) • B – Some evidence that steroids reduce complement activation with BCIS: Inhibition of complement activation by high-dose corticosteriods in total hip arthroplasty. Clin Orthop Relat Res 1998; 236: 205 – 9 • C - “The avoidance of nitrous oxide should be considered in high risk patients to avoid exacerbating air embolism” • D – probably not, especially if BCIS occurs • E – The blood pressure is fine, no need for this |
|
|
Transfusion related acute lung injury (TRALI) occurs
A. almost immediately B. within 4 hours C. within 8 hours D. within 24 hours E. within 48 hours |
C
None quite fit http://ceaccp.oxfordjournals.org/cgi/reprint/6/6/225 article states onset is from tranfusion within 6 hours. Most sites suggest with 6 hours but can occur up to 24hrs |
|
|
The action of which drug is UNCHANGED in the recipient
following cardiac transplantation? A. adenosine B. adrenaline C. atropine D. digoxin E. isoprenaline |
E
Adenosine has an exaggerated effect in denervated heart Denervated heart does not respond to indirectly acting drugs, e.g Atropine Digoxin action via vagal effects – no good in denervated heart Slow response to catecholamines Direct acting drugs, e.g isoprenaline are used instead |
|
|
A 55-year-old man presents for hemi-colectomy. The
LEAST useful intervention to prevent a surgical site infection is A. aggressive peri-operative fluid therapy B. avoidance of blood transfusion C. maintenance of hyperoxia perioperatively D. maintainence of normothermia perioperatively E. timely administration of prophylactic antibiotics |
A
|
|
|
Regarding atrial fibrillation
A. aspirin is as effective as warfarin for the prevention of embolic stroke in elderly patients B. patients should not receive warfarin therapy unless they have other risk factors for embolic stroke C. patients who are converted to sinus rhythm should be placed on rhythm maintenance therapy D. rhythm control has NOT been shown to be superior to rate control E. the best drug for rate control during exercise is digoxin |
D
Perhaps B also 2006 ACC/AHA guidelines for management AF |
|
|
The Neonatal Facial Coding Scale (NFCS), used to assess
pain in neonates, includes all of the following EXCEPT A. brow bulge B. chin quiver C. closed mouth D. deep nasolabial fold E. eyes squeezed shut |
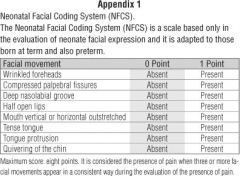
C
|
|
|
A 25-year-old man, involved in a motor vehicle crash,
presented with a GCS (Glasgow Coma Score) of 5. He was intubated and ventilated, and CT scan of his head was consistent with diffuse axonal injury. An ICP (intra-cranial pressure) monitor has been placed. The patient's ICP has ranged between 15 and 25 mmHg over the last 2 hours, despite intravenous mannitol and moderate hypocapnia. He has stable haemodynamics with a mean arterial pressure of 95-100 mmHg. He now requires general anaesthesia to manage his orthopaedic injuries. The most appropriate agents for maintenance of anaesthesia would be A. isoflurane / remifentanil B. propofol / fentanyl C. propofol / nitrous oxide D. sevoflurane / nitrous oxide E. sevoflurane / remifentanil |
B
Propofol for raised ICP is best. Choice between fentanyl and remifentanil: unlikely to be extubated, less risk of hypotension & bradycardia with fentanyl. Want to avoid nitrous oxide |
|
|
Movement(s) produced by the motor components of the C6-
7 nerve roots is/are A. elbow flexion B. elbow pronation and supination C. finger flexion and extension D. shoulder abduction and lateral rotation E. wrist flexion and extension |
E
• A=False (C5,6) • B=False (C6,7,8). • C=False (C7,8 for both). • D=False (Adduction/medial rotation – C6,7,8 and Abduction/lateral rotation – C5). • E=True (C6,7 mediate both movements). |
|
|
In modern anaesthetic practice, mortality from myocardial
infarction after non-cardiac surgery is A. 2.5 - 5% B. 5 - 10% C. 10 - 15% D. 20 - 30% E. approximately 50% |
C
Lots of discussion on wiki "Mortality after PMI is < 10% to 15%, similar to the in-hospital mortality after nonsurgical non-Q infarction. This is in contrast to older data showing a higher (> 50%) mortality after PMI." The Pathophysiology of Perioperative Myocardial Infarction:Facts and Perspectives. Journal of Cardiothoracic and Vascular Anesthesia 2003; 17(1):90-100. |
|
|
An indication for NON-operative management of blunt liver
trauma in adults is A. absence of peritoneal signs B. a haemodynamically stable patient C. a haemopertitoneum of LESS than 500 ml D. a LOW grade injury on CT scan E. severe chronic obstructive airway disease |
B
Non-operative management of blunt hepatic injury in multiply injured adult patients. Al-Mulhim A S. Mohammad H A H. Surg J R Coll Surg Edinb Irel 2003; 1: 81-85: "Until recently, operative management was the standard of care in treating liver injuries. Non-operative management of blunt liver trauma, however, has now evolved into a common practice, especially since abdominal CT has enabled more precise evaluation of these patients. The strategy for this arose from the observation that many liver injuries had stopped bleeding at the time of laparotomy and needed little or no intervention. Guidelines for the non-operative management of blunt liver injuries have been produced... It was concluded that non-operative management should be the initial approach to all patients with blunt liver injury if haemodynamic stability can be ensured. When continued bleeding can be safely ruled out, a period of intensive monitoring is warranted." |
|
|
A 55-year-old, 70 kg woman has had endovascular
treatment of a cerebral aneurysm discovered after presenting with a Hunt and Hess Grade 2 subarachnoid haemorrhage. Postoperative treatment should include A. at least 3 litres per day of normal saline intravenously B. enteral or intravenous magnesium supplementation C. intravenous dexamethasone D. maintenance of a systolic blood pressure greater than 160 mmHg E. sedation and ventilation for 24 hours following procedure |
A
A best (Up-to-date) – previously thought to be D perhaps |
|
|
A 60-year-old man with a 45-pack year history of smoking
and heavy drinking presents with stridor. He has had a hoarse voice for about 4 months. He has been waking at night for a week with difficulty breathing relieved by sitting up. He is sitting upright in bed with moderate inspiratory stridor. His Sa02 on air is 95%. The next step in his management should be A. awake fibreoptic intubation B. CT scan of neck C. examination under anaesthesia following gaseous induction D. nasendoscopy under topical anaesthesia E. tracheostomy under local anaesthesia |
D
Mx of stridor due to malignancy (CCEAP): - awake CT and awake ENT nasoendoscopy to delineate structures involved - then GA is planned: inhalational induction or awake tracheostomy. - NB. AFOI is not a recommended option because: - hard to topicalise well, patient co-operation not assured (already hypoxic), scope may plug remaining airway, may make a tumour bleed into airway |
|

You are anaesthetizing a patient for a laparoscopic
fundoplication. During the case you suspect a tension capnothorax is developing. Which of the capnograph traces below is consistent with this diagnosis? |
?B or E
Tension pneumothorax can result in increased duration of phase II and slope of phase III, i.e. an obstructive pattern due to closure of small airways. This finally results in drop in ETCO2 when pressure is enough to cause circulatory collapse. Capnothorax can result in increase in ETCO2 despite increases in ventilation (i.e. E) |
|
|
During a laparotomy for resection of a liver tumour, a 25 kg
8-year-old has received a rapid transfusion of one unit of packed cells. Her central venous pressure (CVP) is now 8 mmHg. The most likely cause of haemodynamic instability related to this transfusion is A. ABO incompatibility B. coagulopathy C. hyperkalaemia D. hypocalcaemia E. hypothermia |
D
Sandy thought C however "If a patient becomes hemodynamically unstable during rapid blood transfusion, and the circulating blood volume has been maintained, then ionized hypocalcaemia is the most likely cause of hypotension." Pediatric anaesthesia 2005 15:716-726 " Intraoperative pediatric blood transfusion therapy:a review of common issue |
|
|
Oxygen concentration can be measured with each of the
following EXCEPT A. a fuel cell B. a mass spectrometer C. an infra-red absorption analyser D. a paramagnetic analyser E. a Raman scattering analyser |
C
"Infra-red spectroscopy: depends on the ability of gases containing different atoms to absorb infra-red light (thus O2 and nitrogen cannot be analysed)" Yentis, 3rd ed., p. 479 |
|
|
You are performing a level 2 check of your anaesthesia
machine prior to commencing your list. This includes a suction bulb test at the common gas outlet. The bulb does NOT stay collapsed for >10 seconds. Assuming you are performing this test correctly, this may be due to a A. leak at the piped oxygen supply connection B. leaking CO2 absorber C. loosely connected oxygen cylinder D. poorly seated machine outlet check valve E. loosely seated vaporizer |
E
• A - False. Part of the high pressure system. • B - False. Not proximal to the CGO - part of the circle. See below. • C - False. Part of the high pressure system. • D - False. Part of the circle. • E - True. See below. From Anaesthesia Secrets: "These tests, however, do not replace the negative pressure test recommended by Datex-Ohmeda and Dräger for leaks in the machine proximal to the common gas outlet. To perform this test, a no-flow state is first achieved by turning off the machine. The hose connected to the fresh gas outlet is then removed, and the leak detector device (essentially a suction bulb) is attached. After all of the gas is removed from the machine, a flowmeter is opened, and the suction bulb is compressed until it stays flat. If the bulb does not reinflate in 30 seconds, the flowmeter is considered safe. The remaining flowmeters and vaporizers are tested individually in the same way. If all pass, the machine is safe for use. If the machine does not pass, it should be removed for servicing." |
|
|
An anaesthetised patient is ventilated and has standard
monitoring plus a central venous line. As the surgeon is commencing the case, the line isolation monitor (LIM) alarms indicating a potential leakage current of greater than 5 milliamps from one of the power circuits in use. The most appropriate action is to A. check the diathermy return plate B. disconnect the central line to electrically isolate the patient till the fault is identified C. make sure the patient is properly "earthed" or "grounded" D. sequentially unplug non-vital equipment from the circuit until the fault is identified E. suspend the operation and move the patient to a safe environment |
D
Line isolation alarm means a piece of equipment has caused loss of isolation in power supply - any connection from patient to earth will have potential to cause more than 5mA current flow. Therefore: DO NOT touch patient (may inadvertently complete the patient circuit to earth), then sequentially remove equipment to detect culprit. Most commonly due to diathermy equipment. |
|
|
A 60-year-old diabetic has had a below knee amputation for
an ischaemic leg. He has neuropathic pain being managed with oxycodone 40 mg bd and paracetamol 1 g qid. He is also on omeprazole 20 mg daily for reflux. You decide to commence gabapentin. Before deciding on a dosage regimen and commencing therapy it is most important that you A. cease his omeprazole B. check his hepatic transaminase level C. check his renal function D. check his QT interval on a resting ECG E. reduce his oxycodone dose |
C
Renal excretion - must dose reduce. |
|
|
The most frequently reported cause of mortality associated
with transfusion of blood and blood products is A. anaphylaxis B. bacterial sepsis C. haemolytic reaction D. transfusion associated graft versus host disease E. Transfusion Related Acute Lung Injury (TRALI) |
E
Complications of blood transfusion – CEACCP Vol 6 Number 6 2006 TRALI is the most common cause of major morbidity and death after transfusion. It presents as an acute respiratory distresssyndrome (ARDS) either during or within 6 h of transfusion |
|
|
You have anaesthetised a patient with a partially
obstructing right main bronchus tumour. You are using Heliox (28% 02/72% He) and sevoflurane. You secure the airway with an endotracheal tube and continue with the same gas mixture. After 20 minutes the end-tidal CO2 is 28 mmHg. The capnogram waveform is normal. This probably means the patient is A. appropriately ventilated with a low cardiac output B. appropriately ventilated with a normal cardiac output C. hypothermic (34° C) D. hyperventilated E. hypoventilated |
B
Anesthesia 2003. 58:156-160 “Capnography is considered essential in the management of mechanically-ventilated patients. Helium, as an adjunct to mechanical ventilation, is the subject of renewed interest and used increasingly. However, helium affects the performance of infrared capnometry. We constructed a simple device to generate variable mixtures of helium, oxygen and carbon dioxide within the normal physiological range, and tested the performance of two side-stream and one in-line capnographs. We found that addition of helium to the gas mixture caused all three capnographs to underestimate the concentration of carbon dioxide. The underestimation increased as the proportion of helium increased. The maximum underestimation (30%) occurred in a 79:21 helium ⁄ oxygen mixture.” |
|
|
In a patient requiring fresh frozen plasma (FFP), where the
patient's blood group is unknown, it is ideal to give FFP of group A. A B. B C. AB D. 0 E. blood group of FFP in this situation doesn't matter |
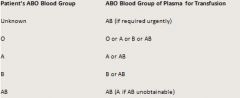
C
|
|
|
In relation to obstetric haemorrhage
A. amniotic fluid embolism is unlikely to present as unexplained haemorrhage B. cell salvage is too dangerous to be recommended because of potential contaminants C. coagulopathy after severe maternal abruption is ONLY likely if foetal death in-utero occurs D. intravenous magnesium may facilitate replacement of an inverted uterus E. placenta percreta can be excluded by ultrasound examination |
D
Similar to previous Miller: "Uterine relaxation may be necessary to replace the uterus; â-sympathomimetic agents, magnesium, and nitroglycerin all have been used to achieve this goal." |
|
|
An elderly patient with chronic lung disease on home
oxygen therapy is to have a submandibular lymph node biopsy under local anaesthesia. An appropriate measure to reduce the risk of fire occurring during this procedure is A. separating the surgical site from the patient oxygen supplementation with an adhesive drape B. titrating the supplemental oxygen so the patient's Sa02 is greater than 97%, but less than100% C. using aqueous chlorhexidine instead of aqueous iodine as the surgical skin preparation D. using bipolar diathermy instead of monopolar for the procedure E. using nitrous oxide in oxygen to provide sedation and reduce oxygen concentration |
D
|
|
|
A 70 kg adult male, who has taken prednisolone 10 mg per
day orally for over 12 months, undergoes an uncomplicated laparotomy and bowel resection. The best management of his steroid therapy perioperatively, until oral intake resumes, is to administer A. hydrocortisone 100 mg intravenously for approximately 24 hours B. hydrocortisone 200 mg per day intravenously for approximately 72 hours C. hydrocortisone 400 mg per day intravenously for approximately 72 hours D. no steroid therapy E. prednisolone 20 mg per day via naso-gastric tube |
D
Otherwise, conversion of prednisolone to hydrocortisone is 1:4. Therefore 10mg = 40mg prednisolone, plus add a bit more for stress of surgery, which could fit with A? From Anaesthesia (53) 1998 1091-1104, Nicholson, Burrin & Hall. Perioperative steroid replacement: "Patients receiving 10 mg or less of prednisolone daily have been shown to have a normal response to HPA testing and do not require formal HPA testing or peri-operative steroids greater than their usual requirements. For other patients we recommend a physiological substitution regimen based on those described by Kehlet, Symreng and colleagues and Salem and colleagues” |
|
|
Each of the following statements regarding vasospasm
occurring after subarachnoid haemorrhage is true EXCEPT A. cerebral vessel narrowing, demonstrated angiographically, can be reversed 30% to 40% of the time by administering nimodipine B. combination therapy resulting in hypertension, hypervolaemia and haemodilition is a mainstay for prevention and treatment C. other causes of neurological deterioration (such as hydrocephalus) need to be excluded before making the diagnosis D. sequential transcranial Doppler measurements may detect those patients at risk E. the peak incidence is 7 - 10 days after the subarachnoid haemorrhage |
A
A. False - see below “nimodipine does not decrease the incidence of angiographic vasospasm and its beneficial effects are likely to relate to other neuroprotective effects” B. Trueish - some controversy as to whether HHH is only used for treatment rather than prophylaxis C. True – makes sense – diagnosis of exclusion D. True. Stoelting p 219 ' daily transcranial doppler sonographic exams are performed to detect vasospasm' E. True - depending on source. Stoelting says vasospasm occurs 3-15 days post SAH therefore peak could occur 7-10 |
|
|
The stellate ganglion is located
A. anterior to the anterior scalene muscle (scalenus anterior) B. anterior to the dome of the pleura C. anterior to the thoracic duct D. at the level of the body of C6 (6th cervical spine) E. posterior to the brachial plexus sheath |
A
• A – True. The stellate ganglion lies ANTERIOR to the scalenius anterior muscle ("Anaesthesia UK" website - Stellate Ganglion Block) • B – false - lies posterior / superior to dome of lung • C – False – Thoracic duct is medial • D – False – anterior to the transverse process of C7 • E – False – posterior is the vertebral body and longus Colli |
|
|
When compared with intra-muscular or subcutaneous
opioid regimens, patient controlled analgesia (PCA) with opioids A. is equally preferred by patients B. provides better analgesia C. results in less opioid-related adverse effects D. results in lower opioid consumption E. results in shorter hospital stay |
B
APM Update 2007 (via college website). Intravenous opioid PCA provides better analgesia than conventional parenteral opioid regimens: Patient preference and satisfaction for intravenous PCA are higher when compared with conventional regimens (Level I [Cochrane Review]). Opioid administration by IV PCA leads to slightly higher opioid consumption. There is no difference in the incidence of nausea and vomiting compared with conventional regimens but the incidence of pruritus is increased. There is no difference in length of hospital stay (Level I [Cochrane Review]). |
|
|
Type 1 Von Willebrand's disease results in
A. an effect on bleeding time that is variable B. prolonged prothrombin time C. prolonged activated partial thromboplastin time D. delayed bleeding following trauma E. haemarthoses |
A
Patients with von Willebrand disease will typically display a normal prothrombin time and a variable prolongation of partial thromboplastin time, and prolonged bleeding time. Type 1 vWD (60-80% of all vWD cases) is a quantitative defect (heterozygous for the defective gene) but may not have clearly impaired clotting, most patients usually end up leading a nearly normal life. Trouble may arise in the form of bleeding following surgery (including dental procedures), noticeable easy bruising, or menorrhagia (heavy periods). Decreased levels of vWF are detected (10-45% of normal, i.e. 10-45 IU). |
|
|
Regarding epidural abscess following the insertion of an
epidural catheter, the following are correct EXCEPT A. diagnosis is dependent upon the triad of fever, back pain and neurological deficit B. gram +ve cocci are the most common causative agents C. non-surgical management may be appropriate D. prognosis worsens with increasing age E. the incidence is between 1:1000 and 1:5000 |
A
A. False – Fever, back pain and neurological deficits are the most common signs and symptoms but is diagnosis dependent on the triad?? “the most common signs and symptoms of epidural abscess after epidural catheterization consist of neurologic deficits (78%), elevated body temperature (56%), and back pain (56%), whereas meningitis is uncommon” B. True – “S. aureus was isolated in 67% of patients, which is in accordance with other reports.” C. True – “Seven patients underwent neurosurgery for evacuation of the abscess, and four were discharged with neurologic sequelae in the form of paraparesis of varying degrees. The patients who were treated with antibiotics only were discharged free of symptoms. Two patients were treated with antibiotics only. It has been suggested that this treatment is acceptable in patients with a lumbar epidural abscess without neurologic symptoms in whom the causative bacteria is known.” D. Truish – the elderly are likely to have co-morbidities = “the majority of the patients with epidural abscess were immunocompromised by one or more complicating diseases” E. – True: - “In this series, the incidence of epidural abscess after epidural analgesia was 1:1,930 catheters, which is higher than previously quoted estimates of approximately 1:5,000.” Incidence of Spinal Epidural Abscess after Epidural Analgesia: A National 1-year Survey - Wang, etal. Anesthesiology: December 1999 - Volume 91 - Issue 6 - p 1928 |
|
|
A strategy shown to reduce the incidence of severe phantom
limb pain is the use of A. continuous regional blockade using nerve sheath catheters B. patient controlled analgesia (PCA) with opioids postoperatively C. perioperative ketamine D. perioperative NSAIDs (non-steroidal anti-inflammatory drugs) E. spinal anaesthesia for the amputation |
C
Acute postamputation pain syndromes 1. Continuous regional blockade via nerve sheath catheters provides effective postoperative analgesia after amputation, but has no preventive effect on phantom limb pain 2. Calcitonin, morphine, ketamine, gabapentin, amitriptyline and tramadol reduce phantom limb pain 3. Sensory discrimination training and motor imagery reduce chronic phantom limb pain 4. Ketamine, lignocaine (lidocaine), tramadol and amitriptyline reduce stump pain 5. Perioperative epidural analgesia reduces the incidence of severe phantom limb pain 6. Perioperative ketamine may prevent severe phantom limb pain |
|
|
A 35 kg 5-year-old girl presents for debridement and
suturing of a lower leg laceration. She is otherwise well, with no significant medical history. After induction with 02, N20 and sevoflurane, and no veins visible, an LMA is inserted. Immediately she develops stridor and airway obstruction. 5a.02 = 90%. After increasing to 100% 02, the appropriate immediate management is A. increasing sevoflurane after removal of the LMA B. increasing sevoflurane with the LMA in place C. intralingual suxamethonium D. intramuscular atropine E. intramuscular suxamethonium |
A
Seems appropriate before moving onto C-D |

