![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
60 Cards in this Set
- Front
- Back
|
150. During adulthood, ageing results in
A. a decline in resting cardiac output B. a decrease in functional residual capacity (FRC) C. an increase in hypoxic ventilatory drive D. an increase in serum creatinine E. an increase in ventricular wall stiffness |
E
From Miller, M&M: • Elderly have decreased GFR, but not necessarily increased Cr due to loss of muscle mass. • FRC does not change with age. • Resting cardiac output is unchanged, but maximal CO is decreased. • Decreased LV compliance means atrial kick is important. • Stroke volume increases with age, but HR decreases. • There is decreased responsiveness to hypoxia. • There is no change in Total Lung Capacity |
|
|
149. In providing general anaesthesia for patients with
congenital long QT syndromes, which of the following statements is correct? A. a priming dose of a non-depolarising muscle relaxant protects against succinylcholine induced arrhythmias B. beta-blocking drugs are relatively contra-indicated C. low dose droperidol is safe D. pre-induction infusion of magnesium sulphate should NOT be used E. thiopentone leaves the QT interval unchanged |
A
Anesthesia for patients with congenital long QT syndrome. Anesthesiology. 2005 Jan;102(1):204-10 • A - true? The ideal muscle relaxant should avoid bradycardia, vagal stimulation, and potassium shifts. It should have little or no histamine release and be short acting to avoid the use of reversal agents. Accordingly, succinylcholine, because of its autonomic effects and potassium release, is far from ideal. It prolongs the QT interval in patients with c-LQTS unless pretreatment with a priming dose of tubocurarine is used." • B. false - indicated • C. false - can prolong QT • D. false - Mg and K should be replaced if low • E. false - propofol thought to be better than thiopentone; STP known to prolong QT |
|
|
148. In clinically used doses levosimendan, a novel inotrope
used in heart failure, A. acts by increasing levels of intracellular cyclic AMP B. increases myocardial intracellular calcium C. increases myocardial oxygen consumption D. increases the rate of fatal ventricular arrhythmias E. increases the sensitivity of intracellular contractile proteins to calcium |
E
Curr Opin Crit Care 2003, 9:337–344: “Calcium sensitizers are a new class of inotropic drugs. They improve myocardial performance by directly acting on contractile proteins without increasing intracellular calcium load. Thus, they avoid the undesired effects of an increased intracellular calcium load. Calcium sensitizers may enhance myocardial performance without increasing myocardial oxygen consumption and without provoking fatal arrhythmias” |
|
|
147. All of the following have anti-emetic properties EXCEPT
A. cannabinoid-1 agonists B. dopamine-2 agonists C. 5-hydroxytryptamine-1A agonists D. 5-hydroxytryptamine-3 antagonists E. neurokinin-1 antagonists |
B
• A – False. o DOES have anti-emetic properties. "Cannabinoids inhibit emesis through CB1 receptors in the brainstem of the ferret." Gastroenterology. 2001 Oct;121(4):767-74. • B – True. o I.e. dopamine-2 agonists are not antiemetic. "Antiemetic drugs: Most act on the vomiting centre directly, e.g. antihistamine and anticholinergic drugs, or on the chemoreceptor trigger zone (CTZ), e.g. phenothiazines, butyrophenones and metoclopramide. The latter group are dopamine receptor antagonists." Yentis, 3rd. ed., p.35. • C – False. o I.e DOES have anti-emetic properties. "5-HT1A receptor agonists may be a useful new class of antiemetic drugs against PONV." Prevention of Nausea and Vomiting with Tandospirone in Adults After Tympanoplasty. Anesth Analg 2002;95:1442-1445. • D – False. o I.e DOES have anti-emetic properties. "Metoclopramide in very high dosage is thought to act via central 5-HT receptors;" Yentis, 3rd. ed., p.35. • E – False. o I.e DOES have anti-emetic properties. "The addition of aprepitant to standard antiemetic therapy in cisplatin-based chemotherapy significantly improves emesis protection in general and, in particular, in the delayed phase by approximately 20%." Neurokinin-1-Receptor Antagonists: A New Approach in Antiemetic Therapy, Onkologie 2006;29:39-43. |
|
|
146. The risk of latex allergy is increased in all of the following
patients EXCEPT those A. who work in hospitals B. with chronic urological conditions C. with food allergy D. with sarcoidosis E. with spina bifida |
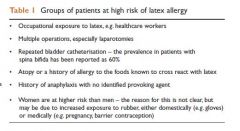
D
BJA CEPD Reviews Vol 2 (1) 2002 |
|
|
145. The normal range of the QRS axis in the ECG is
A. 0 to +180 degrees B. 0 to +90 degrees C. -30 to +90 degrees D. -90 to +90 degrees E. -90 to +30 degrees |
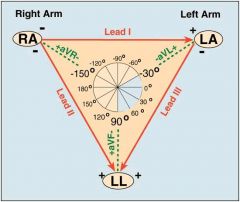
C
|
|
|
144. Modified haemoglobins have been advocated as blood
substitutes. They A. cause nephrotoxicity B. cause systemic hypertension C. have a linear oxygen dissociation curve D. reduce mortality in trauma victims E. require cross-matching |
B
Types of Blood substitutes • Modified haemoglobin – older ones cause renal failure • Perflurocarbons (these have a linear O2 dissociation) http://emedicine.medscape.com/article/207801-overview • Adverse effects associated with hemoglobin-based oxygen carriers include hypertension, abdominal pain, skin rash, diarrhea, jaundice, hemoglobinuria, oliguria, fever, stroke, and laboratory anomalies such as an elevation in lipase levels. Although most of these side effects were transient and clinically asymptomatic, many clinical trials involving these agents have been discontinued or held due to the associated adverse effects • “HemAssist from Baxter Healthcare has been extensively studied by many scientists. Despite its initial success, however, its Phase III trauma trial in the U.S. was stopped after 46.2% of the patients using the product died, compared to the 17.4% death rate in the control group” |
|
|
143. Cephalothin has NO significant activity against
A. escherichia coli B. proteus mirabilis C. pseudomonas aeruginosa D. staphylococcus aureus E. streptococcus pneumoniae |
C
MIMS Online: Cephalothin is usually active against the following organisms in vitro: beta-haemolytic and other Streptococci (most strains of Enterococci, e.g. Enterococcus faecalis, are resistant); Staphylococci (including coagulase positive, coagulase negative, and penicillinase producing strains; methicillin resistant Staphylococci are resistant); Streptococcus pneumoniae; Haemophilus influenzae; Escherichia coli; Klebsiella; Proteus mirabilis. Note. Pseudomonas organisms, most indole producing Proteus sp. and motile Enterobacter sp. are resistant to cephalothin |
|
|
142. Post-operative delirium in the elderly is associated with all
of the following factors EXCEPT A. pre-existing cognitive deficit B. pre-existing hearing impairment C. pre-existing visual impairment D. post-operative urinary tract infection E. use of general anaesthesia rather than regional anaesthesia |
E
Miller edition 6 p2442: 'The type of anaesthesia (regional vs GA) and intraoperative haemodynamic complications have not been associated with delirium.' |
|
|
141. The cardiac valvular lesion identified as the MOST
significant risk factor for non-cardiac surgery is severe A. aortic incompetence B. aortic stenosis C. mitral incompetence D. mitral stenosis E. tricuspid incompetence |
B
From ACC/AHA Guideline Update on Perioperative Cardiovascular Evaluation for Noncardiac Surgery: "Severe aortic stenosis poses the greatest risk for noncardiac surgery. If the aortic stenosis is severe and symptomatic, elective noncardiac surgery should generally be postponed or canceled. Such patients require aortic valve replacement before elective but necessary noncardiac surgery. On the other hand, in patients with severe aortic stenosis who refuse cardiac surgery or are otherwise not candidates for aortic valve replacement, noncardiac surgery can be performed with a mortality risk of approximately 10%. In rare instances, percutaneous balloon aortic valvuloplasty may be justified when the patient is not a candidate for valve replacement." |
|
|
140. The muscles of the upper eyelid receive a somatic nerve
supply from the A. oculomotor nerve and a parasympathetic supply from the superior vagus nerve B. oculomotor nerve and a sympathetic supply from the superior cervical ganglion C. ophthalmic division of the trigeminal nerve and a parasympathetic supply from the superior vagus nerve D. ophthalmic division of the trigeminal nerve and a sympathetic supply from the superior cervical ganglion E. ophthalmic division of the facial nerve only |
B
Anatomy for Anaesthetists: The sensory innervation of the upper lid originates from the supra-orbital, supratrochlear and lacrimal nervesaall three are branches of the ophthalmic nerve (V′). The sensory innervation of the lower lid originates from the infra- orbital branch of the maxillary nerve (V′′) and infratrochlear (V′) nerves. These nerves lie outside the rectus cone and are therefore ineffectively blocked by retrobulbar injections. Oculomotor Nerve : The superior branch passes lateral to the optic nerve to supply the superior rectus muscle and levator palpebrae superioris; the inferior branch supplies three musclesathe medial rectus, the inferior rectus and the inferior oblique (the nerve to the last conveying the parasympathetic fibres to the ciliary ganglion) (see p. 252). |
|
|
139. A patient with known ischaemic heart disease undergoes
percutaneous coronary artery stenting (with a non drug¬eluting stent) prior to major elective surgery. Ideally the surgery should be postponed for A. 1 - 4 weeks B. 4 - 8 weeks C. 8 -12 weeks D. 12 - 24 weeks E. over 24 weeks |
B
ACC/AHA 2007 guidelines If a coronary stent is used in the revascularization procedure, as in the majority of percutaneous revascularization procedures, further delay of noncardiac surgery may be beneficial. Bare-metalstent thrombosis is most common in the first 2 weeks after stent placement and is exceedingly rare (less than 0.1% of most case series) more than 4 weeks after stent placement. Given that stent thrombosis will result in Q-wave MI or death in the majority of patients in whom it occurs, and given that the risk of bare-metal stent thrombosis diminishes after endothelialization of the stent has occurred (which generally takes 4 to 6 weeks), it appears reasonable to delay elective noncardiac surgery for 4 to 6 weeks to allow for at least partial endothelialization of the stent, but not for more than 12 weeks, when restenosis may begin to occur. |
|
|
138. When comparing propofol (induction and infusion for
maintenance) with desflurane (propofol induction only) anaesthesia for ambulatory surgery, which statement is INCORRECT? A. anti-emetic use is higher with desflurane B. incidence of postoperative nausea is higher with desflurane C. time to eye opening in recovery is shorter with desflurane D. time to home readiness is shorter with desflurane E. time to obeying commands in recovery is shorter with desflurane |
D
Waking is faster with Des compared to Propofol, BUT time to discharge is the same. PONV is higher with Des. Comparison of Recovery Profile After Ambulatory Anesthesia with Propofol, Isoflurane, Sevofluran and Desflurane: A Systematic Review - Anil Gupta et al Anaesthesia and Analgesia, March 2004, vol 98 • In this systematic review we focused on postoperative recovery and complications using four different anesthetic techniques. No differences were found between propofol and isoflurane in early recovery. However, early recovery was faster with desflurane compared with propofol and isoflurane and with sevoflurane compared with isoflurane. A minor difference was found in home readiness between sevoflurane and isoflurane (5 min) but not among the other anesthetics. Nausea, vomiting, headache, and postdischarge nausea and vomiting incidence were in favor of propofol compared with isoflurane (P < 0.05). A larger number of patients in the inhaled anesthesia groups required antiemetics compared with the propofol group. We conclude that the differences in early recovery times among the different anesthetics were small and in favor of the inhaled anesthetics. The incidence of side effects, specifically postoperative nausea and vomiting, was less frequent with propofol. |
|
|
137. An eight-year-old boy presents with bleeding one week after
a tonsillectomy. When you see him in the emergency room, he is conscious but restless, tachypnoeic, pale and cool peripherally, with a pulse rate of 135 and blood pressure of 80/60. What percentage of his blood volume is he most likely to have lost? A. 10 -15% B. 15 - 25% C. 25 - 45% D. 45 - 55% E. more than 55% |
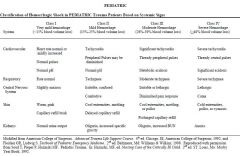
C
|
|
|
135. Compared to propofol, the use of thiopentone for rapid
sequence induction A. causes greater depression of cardiac output and more hypotension B. causes less pain and tissue reaction if injected extravascularly C. is less likely to release histamine D. results in a less rapid and predictable onset of action E. results in a greater incidence of nausea and vomiting |
E
Propofol has intrinsic antiemetic effect |
|
|
134. The leading cause of perioperative death in hip arthroplasty
surgery is A. blood loss B. bone cement implantation syndrome C. myocardial infarction D. pneumonia E. pulmonary embolus |
C
Mantilla "Frequency of myocardial infarction, pulmonary embolism, deep venous thrombosis, and death following primary hip or knee arthroplasty." Anesthesiology 2002 96(5) 1140 • Surveyed 10 years worth of patients (10000 or so) having major orthopedic surgery. He found that pulmonary embolis was more common (0.7%) than MI (0.4%) but that MI was more fatal (28%) than PE (14%). In numbers, 10 out of 10000 died of PE, 13 out of 10000 died of MI within 30 days. • Strictly speaking this means that MI is the commonest form of mortality, although a PE is a much more common event |
|
|
133. The best indication of the adequacy of spinal anaesthesia
for caesarian section is a block to T4 to A. cold B. cold and paralysis of legs C. pin prick D. pin prick and paralysis of legs E. touch |
E
From Oxford Specialist Handbook Obstetric Anaesthesia Pg 286 “Traditional teaching was that an unspecified block to T4 was necessary for CS. However, more recent evidence suggests that loss of sensation to light touch up to and including T5 is the best indicator of a pain free operation.” “The sensation of ice-cold is normally blocked 1-2 dermatomes higher than pain, which in turn is blocked 1-2 dermatomes higher than light touch.” |
|
|
132. The equivalent shock energy with a biphasic defibrillator, to
that of a 360 joule monophasic defibrillator shock is A. 90 joules B. 180 joules C. 360 joules D. 450 joules E. 720 joules |
B
|
|
|
131. Ischaemic preconditioning limits myocardial damage during
a subsequent ischaemic insult. This process is inhibited by A. alpha-2 agonists B. insulin C. isoflurane D. opioids E. sulfonylureas |
E
'Anaesthetics and cardiac preconditioning. Part II. Clinical implications' British Journal of Anaesthesia 91 (4): 566-76 (2003 “Sulfonylurea hypoglycaemic agents prevent ischaemic preconditioning and are thought to be responsible, in part, for the reported increase in cardiovascular mortality in patients treated with these agents” |
|
|
130. Which of the following statements about "bias" in scientific
studies is FALSE? A. bias is a systematic deviation from the truth B. observer bias can be eliminated by blinding C. randomisation is one of the most important ways to reduce bias D. the Hawthorne effect may be reduced by masking the actual intent of a study E. triple-blinding refers to the blinding of patient, observer and investigator |
B
Which of the following statements about "bias" in scientific studies is FALSE? A. bias is a systematic deviation from the truth – true, definition out of Miles & Gin B. observer bias can be eliminated by blinding – false Reduces but doesn’t eliminate bias C. randomisation is one of the most important ways to reduce bias - true "The two most important features of trial design that reduce bias are randomization and blinding" Miles & Gin D. the Hawthorne effect may be reduced by masking the actual intent of a study - true "...the Hawthorne effect, a type of bias. It can be reduced by masking the actual intent of the study..." E. triple-blinding refers to the blinding of patient, observer and investigator - 'true "Blinding of the patient (single blind), observer (double blind) and investigator or person responsible for the analysis of the results (sometimes referred to as triple blind)..." |
|
|
129. Regarding a patient presenting for renal transplantation
due to diabetic nephropathy, which of the following statements is LEAST correct? A. angiotensin-converting enzyme (ACE) inhibitors are probably best discontinued preoperatively B. dialysis is indicated if serum potassium concentration exceeds 6 mmo1.1-1 C. intravenous access should preferably be obtained in a forearm vein of the non-fistulous arm D. suxamethonium causes a rise in serum potassium concentration of up to 0.6 mmo1.1-1 E. temporomandibular joint rigidity may be present |
C
All seem correct. But picking C just as you could still use for IV access if required • A - True. o Could impair graft perfusion o "These drugs have not gained wide acceptance in the treatment of hypertension in renal transplant recipients (RTRs) because of a potential for decreased renal blood flow and glomerular filtration rate associated with a single kidney and concomitant cyclosporine use." ACE inhibitors and angiotensin II antagonists in renal transplantation: an analysis of safety and efficacy. • B – True. o “Although unlikely after immediate preoperative completion of dialysis, potassium levels greater than 6 mEq/L may require a delay in surgery and correction of potassium levels.” Miller online • C – True. o In practice the best answer – “note any sites of AV fistulas and avoid potential sites when placing the IV” p 582 oxford • D – True. o “The increase in serum potassium after an intubating dose of succinylcholine is the same, approximately 0.6 mEq/L, for patients with and without ESRD. This increase can be tolerated without significant cardiac risk even with an initial serum K+ concentration greater than 5 mEq/L.” Miller • E – True o “Limited mobility of the cervical spine or temperomandibular joint may contribute to increased difficulty of laryngoscopy in patients who have severe diabetes mellitus” ANESTH ANALG 1998;86:516-9 |
|
|
128. In relation to gas embolism, which of the following
statements is LEAST correct? A. a patent foramen ovale is present in more than 25% of adults B. hyperbaric oxygen is the treatment of choice for arterial air emboli C. the incidence of air microemboli during caesarean section is up to 40% D. the most sensitive and specific monitor for gas emboli is a praecordial Doppler E. volumes of 100-300 ml of air may be fatal |
D
CEACCP - Gas embolism in anaesthesia 2002 • 27% of adults have a PFO (20-30% quoted elsewhere) • TOE is by far the most sensitive and specific monitor to detect VAE. It can detect up to 0.02ml/kg and is 10x more sensitive than Precordial Doppler • Although Precordial Doppler is highly sensitive at 0.2ml/kg, it is only moderately specific. • Volumes of 100-300mls can be fatal (approx 1ml/kg). 100ml/sec can be entrained through a 14G cannula with only 5cm pressure gradient - i.e. Only takes a few secs to kill someone! |
|
|
127. The usual cardiovascular response to ECT
(electroconvulsive therapy) is A. not predictable as it is very variable B. transient bradycardia followed by tachycardia and hypertension C. transient bradycardia with hypotension D. transient tachycardia and hypertension E. transient tachycardia followed by bradycardia and hypotension |
B
Initial parasympathetic induced bradycardia lasting 10-15 seconds followed immediately by a more prominent sympathetic response that results in tachycardia and hypertension lasting 5 minutes or longer. |
|
|
126. In a haemodynamically stable 20-year-old male presenting
with blunt chest trauma, the best screening test for diagnosis of cardiac injury requiring treatment is A. chest X-Ray B. serum CK-Mb levels C. serum Troponin levels D. standard 12 lead ECG E. transthoracic echocardiography |
D
COA 2008 Feb;21(1):41-6. Anesthetic management of thoracic trauma. In a patient with otherwise minor trauma, a normal ECG at admission can exclude the risk of significant blunt cardiac injury, eliminating the need for cardiac monitoring if not otherwise indicated. If the patient is hemodynamically unstable, an echocardiographic assessment of preload, myocardial contractility, pericardial collections, and myocardial and valvular structures should be performed. Measurement of troponin probably has little value in the management of blunt cardiac injury |
|
|
125. The best clinical sign to demonstrate adequate reversal of
neuromuscular blockade is A. maximum inspiratory pressure of 25 cmH20 B. normal vital capacity (VC) C. protrusion of the tongue D. sustained eye opening E. sustained head lift |

E
Miller: "In addition to using monitors of muscle strength, clinical indicators of adequacy of return of neuromuscular function should also be sought. Such clinical tests include a 5-second head lift, handgrip, and in a patient unable to cooperate with simple commands, the ability to bend the legs up off the operating room table” “Pavlin and coworkers have shown that if patients can successfully perform a head lift, their maximum inspiratory force is approximately -55 cm H2O” |
|
|
124. Intravenous paracetamol has
A. a duration of antipyretic effect of 4 hours B. an antipyretic effect within 10 minutes C. an onset of analgesic effect at 30 minutes D. a peak analgesic effect at 30 minutes E. a peak analgesic effect at 60 minutes |
E
Mims Online. "Perfalgan 10 mg/mL solution for infusion provides onset of pain relief within five to ten minutes after the start of administration. The peak analgesic effect is obtained in one hour and the duration of this effect is usually four to six hours. Perfalgan 10 mg/mL solution for infusion reduces fever within 30 minutes after the start of administration with a duration of the antipyretic effect of at least six hours." |
|
|
123. A three-week-old infant presents with vomiting for 3 days
and a diagnosis of pyloric stenosis. The most correct statement concerning resuscitation is that A. alkalosis should be treated with dilute hydrochloric acid B. 5% albumin is an appropriate fluid for initial treatment of shock C. fluid deficit should be completely replaced with 5% dextrose D. hyponatraemia should be treated with 2N (twice normal) saline E. potassium replacement should begin immediately |
B
Whilst not specifically mentioned, the guidelines do refer to treating shock initially and I can’t see that 5% albumin would be an inappropriate fluid RCH Clinical Practice guidelines: • Fluid resuscitation may be necessary with 10-20ml/kg boluses of normal saline, for patients with moderate to severe dehydration • Commence IV Fluids (0.45% Saline with 5% or 10% Dextrose + 10mmol KCl / 500mls) at 100mls/kg/day initially. Review after 4-6 hours (see below). • Stop oral feeds • Insert a nasogastric tube if vomiting continues despite stopping feeds. Replace nasogastric losses with IV normal saline • Repeat U&E, Acid-Base 4-6 hourly initially and adjust fluid accordingly. The aim for most infants should be to fully correct fluid and electrolyte deficits within 48 hours. • Initial KCl may be required if significant hypokalaemia • Replace deficit, in addition to maintenance, in those infants who are clinically dehydrated (weight is a good marker of the degree of dehydration) |
|
|
122. Von Hippel-Lindau disease is associated with
A. increased risk of malignant hyperthermia B. meningiomas C. peripheral neuropathy D. pheochromocytomas E. poor dentition |
D
Von Hippel-Lindau disease (VHL) is a rare, genetic multi-system disorder characterized by the abnormal growth of tumors in certain parts of the body The tumors of the central nervous system (CNS) are benign and are usuallyhemangioblastomas (or angiomas in the eye). Hemangioblastomas may develop in the brain, the retina of the eyes, and other areas of the nervous system. Inheritance • Familial • Autosomal dominant Features • Retinal angiomas • Haemangioblastomas • Cerebellar and visceral tumours (usually benign but can cause pressure effects) Associations An increased incidence of • Phaeochromocytoma - apparently 20% • Renal cysts • Renal cell carcinoma Anaesthesia • Treat hypertension occurring with phaeochromocytoma • Haemangioblastoma of spinal cord may limit use of spinal although epidural has been used for LSCS • Exagerrated hypertension with surgical stimulation or laryngoscopy o Treat with β blockers and/or SNP |
|
|
121. The pressure in wall oxygen gas supply pipelines in
operating theatres is approximately A. 100 kPa (kilopascals) B. 200 kPa C. 300 kPa D. 400 kPa E. 600 kPa |
D
Yentis A-Z Anaesthesia 3rd ed p415 All piped gases are at 4 bar = 400kPa (except high pressure for ortho jackhammer etc) |
|
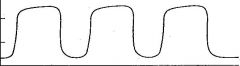
120. The capnograph below is most consistent with
A. a hypermetabolic state B. incomplete expiration C. the presence of a right-to-left shunt D. ventilation via a Circle System E. ventilation via a Mapleson D System |
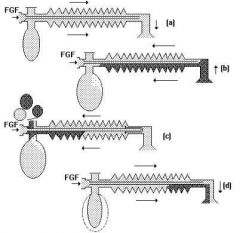
E
Raised baseline suggests partial rebreathing, typical of the Bain circuit. |
|
|
119. Which of the following statements is INCORRECT?
Selective cyclo-oxygenase-type 2 (COX-2) inhibitors A. are contraindicated in patients with ischaemic heart disease B. block the production of prostacyclin in diseased vessels C. block the synthesis of prostaglandins involved in renal salt and water homeostasis D. block thromboxane A2 synthesis in platelets E. do NOT block the synthesis of prostaglandins involved in gastric mucosal protection |
D
• Option A - True. COX II inhibitors have an increased incidence of myocardial infarction in patients who have IHD. (hence VIOXX withdrawal) • Option B - True - Prostacyclin synthesis is inhibited NEJM : COX II Inhibitor "This would be consistent with the formation of thromboxane in the absence of the concomitant generation of prostacyclin." • Option C - True - Prostaglandin is involved in renal protection. COX II Inhibitors have an effect on reducing GFR. NEJM : COX II Inhibitors "12.5 or 25 mg of rofecoxib once daily and 50 mg of indomethacin three times daily reduced the glomerular filtration rate in salt-depleted elderly subjects, but to a similar degree." • Option D - False hence the answer. Platelet thromboxane A2 production is preserved (or even enhanced due to lower prostacyclin), hence platelet aggregation is unimpaired. • Option E - True - Gastric mucosal production of prostaglandins is preserved. COX 1 and COX 2 both present in the stomach but ulcer rate not increased because COX 1 is not inhibited. |
|
|
118. A sub-Tenon's eye block is absolutely contraindicated in
A. a severely myopic patient B. a warfarinised patient C. previous glaucoma surgery D. previous retinal detachment repair E. none of the above |
E
CEACCP 2006 Preoperative assessment in ophthalmic regional anaesthesia "An absolute indication for general anaesthesia is patients who have undergone previous surgery for retinal detachment or choroidal melanoma, unless the operation can be done under topical anaesthesia. After retinal detachment surgery, the globe shape will be altered significantly if an encircling band has been attached. It is therefore impossible to know where an inferotemporal needle is in relation to the globe. Sub-Tenon’s is also not an option in these cases because of the band. Previous surgery for some intraocular melanomas can leave the sclera very thin. A needle and some sub-Tenon’s cannulae could easily puncture this." However… EJA 2005; 22; 567-77: “A review of sub-Tenon's block: current practice and recent development' under 'Limitations of sub-Tenon's block' only states: "The block may be difficult to perform in patients who have had previous sub-Tenon’s block in the same quadrant, previous retinal detachment and strabismus surgery, eye trauma and infection to the orbit." Doesn't sound as if the authors regard previous detachment surgery as an absolute contraindication Sounds like it is more a relative contraindication |
|
|
117. Features of Conn's syndrome (primary hyperaldosteronism)
include each of the following EXCEPT A. acidosis B. high urinary potassium C. hypertension D. hypokalaemia E. low plasma renin |
A
From OHA p. 170 • refractory hypertension • metabolic alkalosis from tubular H+ secretion (K+/H+ exchange) • hypervolaemia • hypokalaemia • polyuria from nephrogenic diabetes insipidus • impaired glucose tolerance in 50% • muscle weakness from hypoK+ (especially in ethnic chinese) • aldosterone to renin ratio >400 |
|
|
116. In Australasia all of the following tests are routinely
performed before releasing blood for transfusion EXCEPT A. indirect antiglobulin test to cross match ABO and Rh compatible blood B. screening the recipient serum for red cell antibodies using the indirect antiglobulin test and red cells of known antigen phenotype C. testing donor blood for Hepatitis C antibody D. testing donor blood for HIV 1 and 2 antibody E. testing donor blood for syphilis |
A
Australian Red Cross Blood Service: Serological crossmatching techniques have been simplified in recent years, and only the 37°C IAT crossmatch and immediate room temperature spin crossmatch remain in common use. The IAT crossmatch is performed when the patient’s serum/plasma contains clinically significant red blood cell antibodies. The room temperature immediate spin crossmatch has been retained primarily to detect ABO incompatibility. A request for a ‘type and screen’ (also commonly referred to as a ‘group and hold’) involves the following: • Determining the ABO and Rh(D) group of the person, and • Performing a red cell antibody screen on the person o For patients who have a negative red cell antibody screen, a rapid serological crossmatch (such as the immediate spin crossmatch) or electronic crossmatch is performed to ensure ABO compatibility prior to the issue of the donor red cells. o Patients who have a positive red cell antibody screen require antibody identification and full serological crossmatching, using the indirect antoglobulin test (IAT). Specially selected donor red cell units should be made available prior to surgery |
|
|
115. Residual Current Devices (also known as Safety Switches)
A. detect differences in current between the active and neutral wires of a circuit B. isolate the patient from earth C. monitor the isolation of the power line D. must be fitted to all Cardiac Protection areas E. must be fitted to all operating theatres |
A
Wiki: A residual-current device (RCD), similar to a Residual Current Circuit Breaker (RCCB), is an electrical wiring device that disconnects a circuit whenever it detects that the electric current is not balanced between the energized conductor and the return neutral conductor. Such an imbalance is sometimes caused by current leakage through the body of a person who is grounded and accidentally touching the energized part of the circuit. A lethal shock can result from these conditions. RCDs are designed to disconnect quickly enough to mitigate the harm caused by such shocks although they are not intended to provide protection against overload or short-circuit conditions. RCDs operate by measuring the current balance between two conductors using a differential current transformer. This measures the difference between the current flowing out the live conductor and that returning through the neutral conductor. If these do not sum to zero, there is a leakage of current to somewhere else (to earth/ground, or to another circuit), and the device will open its contacts. |
|
|
114. Prilocaine is superior to lignocaine for intravenous regional
anaesthesia because prilocaine A. exhibits no cardiotoxicity B. has a higher pKa C. has a larger volume of distribution D. is an ester, metabolised in the bloodstream E. is more highly protein bound |
C
▪ A: clearly wrong- all LAs are cardiotoxic ▪ B: similar, pKa prilocaine 7.7, pKa lignocaine7.9 ▪ C: TRUE - greater volume of distribution of prilocaine = lower plasma concentration ▪ D: Prilocaine is an AMIDE, not an ester ▪ E: False. Prilocaine has a LOWER protein binding 55% vs Ligno 60-70% (depending on source) In fact the correct answer is none of the above. The real reason Prilocaine is superior to Lignocaine for IVRA is because it is the most rapidly metaboilized LA with metabolism occurring in the kidney, liver and lungs; ideal for when you let down the torniquet and release all that IV Prilocaine |
|
|
113. Frank haemoptysis occurs LEAST frequently in
A. bronchiectasis B. chronic bronchitis C. mitral stenosis D. pulmonary infarction E. pulmonary tuberculosis |
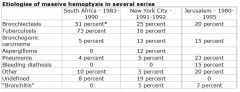
C
Almost Repeat From Uptodate: There are numerous causes of massive hemoptysis originating from the lower respiratory tract, the most common and important of which will be discussed here. The literature from the 1940s through the 1960s supports three major etiologies accounting for 90 percent of cases: tuberculosis (TB), bronchiectasis, and lung abscess. "Less commonly (< 10% of cases), pulmonary venous hypertension (eg, mitral stenosis, pulmonary embolism) causes hemoptysis." (Current Medical Dx and Tx, Ch2) |
|
|
112. The recommended concentration of hyaluronidase as an aid
for local anaesthesia in peribulbar injection for ophthalmic surgery is A. 25 IU (International Units).m1-1 of local anaesthetic solution B. 50 IU.m1-1 of local anaesthetic solution C. 100 IU.m1-1 of local anaesthetic solution D. 150 IU.m1-1 of local anaesthetic solution E. 1500 IU.m1-1 of local anaesthetic solution |
A
|
|
|
111. The respiratory pattern of a patient sustaining an acute C5
spinal cord injury is characterised by A. a rapid respiratory rate B. arterial hypoxaemia C. chest wall immobility D. preservation of the cough E. preservation of the inspiratory force |
B
The phrenic nerves arise from C3, 4 and 5 nerve roots. Thus if a lesion is below C5 diaphragmatic function is preserved. Injuries above C3 cause instant death unless ventilation is secured immediately. Lesions below C6 cause variable intercostal and abdominal muscle weakness. Intercostal paralysis leads to indrawing of the flaccid intercostal muscles during inspiration. The result is: • FRC falls. • FVC falls. • Maximum inspiratory/expiratory pressures fall. • Vital capacity is reduced to ~1500mls in C. Spine lesions. • Tidal volume is reduced (up to 60%). The overall effect is severe hypoventilation producing hypercapnia and hypoxaemia. The inability to cough and clear secretions leads to atelectasis and pneumonia. |
|
|
110. All of the following clinical findings suggest the diagnosis of
aortic stenosis EXCEPT A. an early systolic murmur B. brachioradial pulse delay C. decreased intensity or absence of S2 (second heart sound) D. decrease in murmur intensity with a Valsalva manoeuvre E. effort syncope |
A
• A false, thus correct answer. Midsystolic. “Valvular or subvalvular obstruction (stenosis) of either ventricle may ... cause a midsystolic murmur. (whereas) An early systolic murmur is often due to TR occurring in the absence of pulmonary hypertension and in other patients with acute MR.” AHA ACC Guidelines for Management of Patients with Valvular Heart Disease. • B is true, hence NOT the correct answer!!! (from BB) o Brachioradial delay and severity of aortic stenosis. Caro CG, Parker KH. Lancet. 1990 Jun 23;335(8704):1535. "During the assessment of patients with severe or symptomatic aortic stenosis, a clinically detectable delay between the brachial and radial pulses was observed. This delay was not present in normal subjects. The timed delay of 53.5 (SE 2.6) ms in severe aortic stenosis was significantly longer than that in normal volunteers 22.6 [1.3] ms) or in patients with low cardiac output. This increased delay was clinically detectable before the occurrence of left ventricular failure and often before the onset of symptoms” • C technically false, thus also correct, but not best answer. (A2 that is soft, not P2) • D true. - the murmur intensity is reduced during Valsalva strain, which is contrary to what occurs with hypertrophic obstructive cardiomyopathy where a Valsalva maneuver increases the intensity of the murmur. • E true. |
|
|
109. Correct statements regarding complementary and
alternative medications include A. ginger is a superior antiemetic to metoclopramide B. ginseng and ephedra may produce cardiovascular complications during general anaesthesia C. ginseng and ephedra may potentiate the analgesic properties, but not the bleeding side-effects, of the non-steroidal anti-inflammatory drugs (NSAIDS) D. it is generally recommended that patients can continue these medications perioperatively E. St. John's Wort is associated with acute tubular necrosis perioperatively |
B
Current Opinion in Anaesthesiology 2007, 20; 294-299 Australasian Anaesthesia 2003 Grauer, R. Herbal Medicine and Perioperative Care – An Australian Perspective. Herbal Medicines and Perioperative Care. Michael K. Ang-Lee; Jonathan Moss; Chun-Su Yuan JAMA. 2001;286(2):208-216 Anaesthesia MCQ – Herbal Medicines: http://www.kerrybrandis.com/wiki/mcqwiki/index.php?title=Herbal_medications Saw palmetto associated HT, CCF, arrhythmias, tachycardia and angina. Same with ginseng, ephedra |
|
|
108. Sickle cell disease (homozygous haemoglobin SS) is
frequently associated with A. cardiomyopathy B. chronic respiratory dysfunction C. nephropathy D. peripheral neuropathy E. all of the above |
E
Cant find specific reference for D, but the rest are true so must be E Stoelting: • Sickle cell anemia, the homozygous form of Hb S disease, presents early in life with a severe hemolytic anemia and vaso-occlusive disease involving the marrow, spleen, kidney, and central nervous system • Recurrent splenic infarction culminating in loss of splenic function in the first decade of life • The renal medulla is another prime target, with loss of concentrating ability an early feature of the disease progressing to chronic renal failure usually in the third or fourth decade of life • Lung damage results from chronic progressive lung damage due to persistent inflammatory reactions punctuated by acute chest syndrome, a pneumonia-like complication characterized by a new pulmonary infiltrate involving at least one complete lung segment and at least one of the following: chest pain, fever higher than 38.5°C, tachypnea, wheezing, or cough • Neurologic complications may include stroke, usually infarctive in adolescence and hemorrhagic later in adult life Harrisons: • "A sickle cell cardiomyopathy and/or premature coronary artery disease may compromise cardiac function in later years |
|
|
107. The risk of transmission of Hepatitis C to a health care
worker from an infected patient after a needle stick injury is approximately: A. 0.5% B. 2 - 8% C. 8 - 15% D. 15 - 20% E. 20 - 30% |
B
Either A or B depending on who you believe: Berry. Anesthesiology Clin N Am 22 (2004) 493– 508 • "Early studies suggested that the transmission rate after percutaneous exposure to HCV is 1.8% (range 0%–10%). More recent surveys using larger sample sizes demonstrate that the risk of transmission of HCV after percutaneous exposure is significantly lower, approximately 0.5%." eMJA The Medical Journal of Australia MJA 2003; 179 (3): 153-157 • "As there is a 1.8%–3% risk of transmission of HCV from a needlestick injury, two to five healthcare workers are likely to acquire HCV each year in Victoria." CDC, July 2003 • "The average risk for infection after a needlestick or cut exposure to HCV infected blood is approximately 1.8%." CEACCP 2006 – Occupational Hazards of Anaesthesia • “Hepatitis C is also a blood-borne pathogen. The risk of transmission after a hepatitis C contaminated occupational exposure has been estimated at 2%” |
|
|
106. The commonest initial presenting feature in anaphylaxis is
A. coughing B. desaturation C. hypotension D. rash E. wheeze |
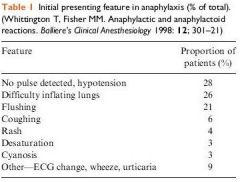
C
Anaphylaxis During the Perioperative Period. Anaesthesia & Analgesia, 2003 vol. 97 no. 5 1381-1395: • “Because patients are under drapes and mostly unconscious or sedated, the early cutaneous signs of anaphylaxis are often unrecognized, leaving bronchospasm and cardiovascular collapse as the first recognized signs of anaphylaxis. A survey of anaphylaxis during anesthesia demonstrated that cardiovascular symptoms (73.6%), cutaneous symptoms (69.6%), and bronchospasm (44.2%) were the most common clinical features” |
|
|
105. The MAC (Minimum Alveolar Concentration) of desflurane
in infants less than one year of age is A. less than 6% B. 6 to 7% C. 7 to 8% D. 8 to 9% E. greater than 9% |
E
From Stoelting: Age Des in O2 0.04 9.29% 0.6-0.7 9.96% 1.6-1.8 8.73% 2-5 8.54 7.6 8.16 25 7.25 36-49 6.00 65-70 5.17 |
|
|
104. Carbon monoxide (CO) production occurs when volatile
anaesthetics have contact with anhydrous soda lime. The volatile agent which has been found to produce the most CO is A. desflurane B. enflurane C. halothane D. isoflurane E. sevoflurane |
A
Des>Enf>Iso>Halo=Sevo Factors affecting production: • Temp: increases rate of production • Baralyme: produces more heat and therefore more CO (also more compound A) • Dehydration: dry soda/baralyme produces more CO • Low flows/closed circuit: leads to higher concentration of CO |
|
|
103. In trauma patients, the main mechanism by which
hypothermia exacerbates bleeding is by A. altering blood viscosity B. causing disseminated intravascular coagulation C. inhibiting clotting factors D. potentiating anticoagulants used for DVT (deep venous thrombosis) prophylaxis E. reducing platelet function and number |
E
Though C could also be correct (see last point) Miller: • "The inhibitory effects of hypothermia on platelet function are well recognized." Hypothermic coagulopathy in trauma: effect of varying levels of hypothermia on enzyme speed, platelet function, and fibrinolytic activity. J Trauma. 1998 May;44(5):846-54 • " Enzyme activity slowing and decreased platelet function individually contributed to hypothermic coagulopathy in patients with core temperatures below 34.0 degrees . All the coagulation measures affected are part of the polymerization process of platelets and fibrin, and this process may be the mechanism by which the alteration in coagulation occurs." • “Patients whose temperature was > or =34.0 degrees C actually demonstrated a significant hypercoagulability” J. Trauma 2008;65:748-7541 • "Hypothermia inhibits coagulation protease activity and platelet function. The activity of tissue factor or FVIIa complex decreases linearly with temperature, retaining only 50% of its activity at 28°C. Overall, however, hypothermia may have little effect on FVIIa and other protease activity. Platelets are probably more sensitive to hypothermia, with low temperatures decreasing activation. This is due to a reduced effect of von Willebrand factor traction on glycoprotein Ib/IX, which mediates the signal transduction from initial adhesion to activation, and activation is essentially absent below 30°C." |
|
|
102. In women with congenital heart disease the clinical
scenario associated with the greatest maternal mortality is A. aortic stenosis with a valve area less than 0.7 cm2 B. Eisenmenger's syndrome C. left ventricular ejection fraction less than 35% D. Marfan's syndrome with dilated aortic root E significant aortic coarctation |
B
Severe cardiac disease in pregnancy, part II: impact of congenital and acquired cardiac diseases during pregnancy. Curr Opin Crit Care 11:435—448. 2005: • A - "A review of multiple small studies yielded a maternal mortality rate of 11% and perinatal mortality of 4%. A more recent study reported no maternal mortality and general satisfactory outcome with deterioration of functional status in 20% of patients." • B - "Eisenmenger’s syndrome carries a 30% risk of maternal mortality in each pregnancy, with most complications occurring at term or the first week postpartum”. • C - "Mortality ranges from 25% to 50%, with nearly 50% of deaths occurring in the first 3 months postpartum, but outcome differs widely between reports.". • D - "Patients with aortic root diameters less than 4.5 cm without cardiovascular complications may deliver vaginally with epidural anesthesia, and assisted second stage. Maternal mortality has decreased from 30% to 1%, with a fetal mortality rate of 22%." • E - "Uncorrected coarctation of the aorta carries a maternal mortality risk of 3%, but can be higher when other associated cardiac defects, aortic abnormalities, or pre-existing longstanding hypertension are present." |
|
|
101. Spinal correction is planned for a twelve-year-old girl with
idiopathic scoliosis. Potential problems associated with this condition include A. diabetes insipidus B. laryngeal abnormalities C. mitral valve prolapse D. phaeochromocytoma E. renal artery stenosis |
C
CEACCP - Scoliosis surgery in children 25% of idiopathic scoliosis have mitral valve prolapse (rarely of clinical significance) |
|
|
136. Which of the following statements is INCORRECT?
Recombinant Factor Vila A. directly activates Factors IX and X on the surface of activated platelets, leading to thrombin formation B. has a half-life of three and a half hours C. has been used "off-label" for bleeding in trauma patients D. is best monitored by the prothrombin time, which is shortened in a dose-dependent manner at therapeutic doses E. was developed for patients with haemophilia A and B who have inhibitors to Factors VIII and IX respectively |
D
A – true. ‘Factor VIIa can also activate factors IX & X on the platelet membrane, in the absence of Tissue Factor. Although this is a lower affinity reaction for generation of Factor Xa, Factor IXa subsequently activates Factor Xa and amplifies this pathway dramatically. This reaction is often referred to as the 'Thombin Burst' and is thought to be responsible for the majority of fibrin generated in response to a local injury.’ B – trueish. Most websites actually quote 2-3 hours, including MIMS, but some have half life up to 4 hours. C – true. 1st described in 1999 – use in soldier with gunshot wound to IVC and consequent traumatic coagulopathy D – false. ‘Coagulation parameters should not be used to evaluate NovoSeven effectiveness’ MIMS Online E – true. From manufacturer’s website. www.novosevenrt.com |
|
|
20. The most useful clinical finding to exclude the presence of
airflow limitation in a 60 year old is A. a history of never smoking B. absence of hyperresonance to chest percussion C. normal cardiac dullness to percussion D. absence of pulsus paradoxus E. non-use of accessory muscles at rest |
A
Holleman and Simel: Journal of the American Medical Association 1995; 273 (4): 313-319 A thorough medical examination may detect signs and symptoms of airflow limitation. Airflow limitation is a respiratory disease characterized by narrowed lung passages and increased lung secretions. Researchers reviewed the medical literature that evaluated clinical examination findings indicative of airflow limitation. Patients' exposure to cigarette smoke, particularly the length of smoking history, is positively associated with the risk of airflow limitation. Age is related to airflow limitation, with the highest rates found in children younger than age 10 and adults older than age 30. Physical findings associated with an increased risk of airflow limitation include a rounded, large chest, abnormal breathing sounds including wheezing and rhonchi, abnormal chest sounds heard on percussion, and subxyphoid apical impulse. Patients who cannot blow out a lighted match held 10 centimeters away from their mouth and those with a forced expiratory time greater then nine seconds are likely to have airflow limitation. |
|
|
Myotonic dystrophy
A. usually presents before puberty B. is frequently associated with cardiac failure C. is associated with obstructive lung disease D. contractions are not relieved by nondepolarising neuromuscular blockers and deep anaesthesia E. is associated with mitral valve prolapse in over 50% of patients |
D
• A – false, usually presents in 20-30’s • B – Can cause cardiac failure in later stages, but probably doesn’t count as ‘frequently’ and is not the leading cause of death (pneumonia) • C- false, restrictive defect more likely • D - "Interestingly, general anesthesia, regional anesthesia, and neuromuscular blockers are not able to prevent or relieve this skeletal muscle contraction." (Stoelting Ch 18) • E – MV prolapse in 20% |
|
|
Factors associated with post-operative ulnar nerve palsy
include all of the following EXCEPT A. male gender B. sternal retraction for cardiac surgery C. cardiopulmonary bypass for cardiac surgery D. internal jugular vein catheterisation E. diabetes mellitus |
C
1. A=False - this is a risk factor : Anesthesiology Clin N Am 20:(2002) 589– 603: - This bony prominence is at least 50% larger in males, consistent with their greater susceptibility to perioperative ulnar nerve damage 2. B=False - this is a risk factor : Miller 6th ed. Pg. 1154: - “Brachial plexus injuries occur primarily in cardiothoracic procedures requiring median sternotomy. Mechanisms for injury during median sternotomy include stretch or compression of the plexus during sternal separation, direct trauma from fractured 1st ribs, stretching related to internal mammary dissection and trauma or haematoma related to internal jugular vein cannulation. “ 1. C=?True – whilst is associated with cardiac surgery it is not related to the CPB per se 3. D=False – as per above quote from miller – haematoma from IJ cannulaion could cause brachial plexus injury 4. E=False – this is a risk factor apparently (pre-existing neuropathy) |
|
|
The chief concern in the anaesthetic management of mitral
stenosis is to avoid tachycardia because it A. increases the trans-mitral pressure gradient B. aggravates left ventricular ischaemia C. increases myocardial oxygen consumption D. frequently precipitates atrial fibrillation E. reduces the size of the left atrium |
A
• A - correct: tachycardia decreases LV filling, and hence increases LA size and pressure. This means increased transmitral pressure gradient. • B - wrong: it is a reason for avoiding tachycardia in AS • C - wrong: it is a reason for avoiding tachycardia in AS • D - wrong: • E - wrong: increases |
|
|
49. In providing anaesthesia for a patient with Eisenmenger's
syndrome, it is NOT true that A. an important goal is to maintain an optimal shunt, by preventing changes to pulmonary vascular resistance (PVR) or systemic vascular resistance (SVR) B. the patient's high haemoglobin should be maintained and blood loss monitored closely C. a gaseous induction with sevoflurane presents an effective method for anaesthesia and avoids cardiovascular compromise D. if general anaesthesia is required, ketamine is an appropriate choice of drug E. careful attention to intravenous infusions and drug administration is needed to prevent paradoxical air embolism |
C
- A: From Stoelting: o "Management of anesthesia for patients with Eisenmenger's syndrome undergoing noncardiac surgery is based on maintenance of preoperative levels of systemic vascular resistance and recognizing that increases in right-to-left intracardiac shunting are likely if sudden vasodilation occurs." I.e. maintain the PVR/SVR ratio at an optimal level for the patient. - B: Obviously true - C: Whilst this may be a suitable method of induction it wouldn’t “avoid cardiovascular compromise” - D: Whilst ketamine classically said to increase PVR there are a number of sources stating it’s safe use in this setting. Including Miller: o "Ketamine has been the most popular agent for anesthetic induction in patients with cyanotic conditions because it increases SVR and cardiac output, thereby diminishing the magnitude of R-L shunting." - E: Obviously true given the right to left shunt |
|
|
In patients giving a history of penicillin allergy
A. cross-sensitvity to cephalosporins occurs in approximately 30% of patients B. there is an increased liklihood of allergic reactions to neuromuscular blocking drugs C. beta-lactamase resistant penicillins are less likely to provoke a response D. a 'test dose' of one tenth the planned dose of penicillin should be given with a 5 minute delay before the main dose |
B
o A – False http://www.australianprescriber.com/magazine/17/3/62/5/ “Cephalosporins share a common beta-lactam ring with the penicillins but the degree of cross-reactivity is quite low. Around 3-7% of those with penicillin allergy, for example, may have allergic reactions to cephalosporins as well” http://www.allergy.org.au/aer/infobulletins/hp_antibiotics.htm o B – True “A review of this subject found that patients with an allergy to penicillin were more likely (threefold) to experience an anaphylactic reaction to any other drug” http://www.anesthesia-analgesia.org/cgi/content/full/97/5/1381 o C – false Beta lacatamse resistant penicllins include flucloxacillin “The major limiting factor for the use of penicillins is the high incidence of reported allergy (5%). ….Anaphylactic reactions occur in 1/10000 patients. Symptoms range from urticaria to anaphylactic shock. All other beta lactams should be avoided in these patients.” http://www.utmb.edu/otoref/Grnds/Antibiotics-update-2005/Antibiotics-2005_0412.htm o D – false - I wouldn’t give it IV “skin prick testing is the gold standard for the diagnosis of penicillin allergy” Essentials of allergy By Mamidipudi Thirumala Krishna, George Mavroleon, S. T. Holgate |
|
|
In congenital diaphragmatic hernia
A. there is hyperplasia of pulmonary arterioles in the hypoplastic lung B. right-sided lesions are more pathologically significant C. vasodilator drugs are contraindicated D. right-sided lesions through the foramen of Bochdalek are the most common E. intrapulmonary shunts are the major cause of cyanosis |
A
• A – True. From RCH Neonatal Handbook: o Congenital diaphragmatic hernia is a serious congenital abnormality associated with pulmonary hypoplasia, worse on the ipsilateral side structural and functional lung immaturity a reduction in pulmonary arteriolar cross sectional area muscular hyperplasia of remaining pulmonary arterioles an association with other major anomalies, chromosomal and non-chromosomal, in up to 20% of cases • B - ?? • C – False. • D – False. From Emedicine: o The 3 basic types of congenital diaphragmatic hernia include the posterolateral Bochdalek hernia (occurring at approximately 6 weeks' gestation), the anterior Morgagni hernia, and the hiatus hernia. The left-sided Bochdalek hernia occurs in approximately 85% of cases. Left-sided hernias allow herniation of both the small and large bowel and intraabdominal solid organs into the thoracic cavity. In right-sided hernias (13% of cases), only the liver and a portion of the large bowel tend to herniate. Bilateral hernias are uncommon and are usually fatal. o From Wikipedia: A Bochdalek Hernia is one of two forms of a congenital diaphragmatic hernia, the other form being Morgagni's hernia. A Bochdalek Hernia is a congenital abnormality in which an opening exists in the infant’s diaphragm, allowing normally intra-abdominal organs (particularly the stomach and intestines) to protrude into the thoracic cavity. In the majority of patients, the affected lung will be deformed, and the resulting lung compression can be life-threatening. Bochdalek hernias occur more commonly on the posterior left side (85%, versus right side 15%). • E – False. |
|
|
79. Application of cricoid pressure with a force of 40 newtons
will resist reflux with an intra-oesophageal pressure of A. 30 mmHg B. 40 mmHg C. 50 mmHg D. 60 mmHg E. 70 mmHg |
E
Cricoid pressure of 40N will be effective against a lower oesophageal pressure of at least 100 cm H2O (Miller IV p1456) 100 cm H2O /1.36 cm H2O/1 mmHg =73.5 mmHG |
|
|
87. A known alcoholic with anorexia and nausea has become
jaundiced. His urine is dark and his faeces pale. He has discomfort in the right hypochondrium. The AST (SGOT) is 2000 IU.1-1, the alkaline phosphatase 100 IU.1-1 and the serum bilirubin is 75 micromo1.1-1. The best treatment would be A. withdrawal of alcohol B. expectant C. operation to remove obstruction (gallstones tumour) D. urgent liver biopsy E. endoscopy |
A
|
|
|
92. Which of the following statements is NOT true of the
neuroleptic malignant syndrome? A. it is a rare complication of dopaminergic antagonist drugs B. it may be successfully treated with bromocriptine C. it may be successfully treated with dantrolene D. unlike malignant hyperpyrexia it does not have a genetic component E. the syndrome includes extra-pyramidal signs, hyperthermia peripheral vasoconstriction, tachycardia, dyspnoea and other autonomic manifestations |
D
• A - True. "Neuroleptic malignant syndrome (NMS), first described in 1963 by Delay et al in the French psychiatric literature, is a rare but potentially lethal complication of treatment with potent neuroleptics. Neuroleptic drugs (ie, antipsychotic drugs, antischizophrenic drugs) are primarily used to treat schizophrenia and other psychotic states. Traditional drugs have action through inhibition of dopaminergic receptors, whereas the newer agents work by causing blockade of serotonin receptors." • B - True. • C - True. • D - ? False. Conflicting evidence from Adnet in BJA 2000 and Stoelting AACD. o "Because there are similarities between neuroleptic malignant syndrome and malignant hyperthermia, the possibility that patients with a history of neuroleptic malignant syndrome are vulnerable to developing malignant hyperthermia is an important issue to consider. At the present time, there is no evidence of a pathophysiologic link between the two syndromes, and there is no familial pattern or evidence of inheritance in neuroleptic malignant syndrome." Stoelting AACD. • E - True. "A potentially fatal syndrome called neuroleptic malignant syndrome has been reported in association with antipsychotic drugs including droperidol. The syndrome is characterised by muscular rigidity, fever, hyperthermia, altered consciousness and |

