![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
75 Cards in this Set
- Front
- Back
|
134. The drug most likely to cause an increase in intra-ocular pressure is
A. ketamine B. propofol C. thiopentone D. diazepam E. etomidate |
A
|
|
|
133. In Wolff-Parkinson-White (WPW) syndrome,
A. the delta wave is caused by a delay in conduction in the accessory pathway B. the PR interval is of normal duration but the QRS complex is widened C. a narrow complex supraventricular tachycardia (SVT) is the most common form of arrhythmia D. central venous cannulation is unlikely to trigger SVT E. cardioversion of arrhythmias is seldom effective |
C
|
|
|
131. Changes in the fetal circulation following birth include
A. an immediate increase in pulmonary vascular resistance B. functional closure of the foramen ovale at one hour C. physical closure of the foramen ovale at several weeks D. a decrease in systemic vascular resistance E. closure of the ductus arteriosus in the first few hours |
B
PVR decreases functional closure is generally in place at one hour Total physical closure of the foramen ovale (when it occurs) takes up to a year SVR increases (loss of placental circulation) The actual closure of the ductus takes place in two stages. In healthy full term newborns, functional ductal closure occurs by 96 h. This functional closure is followed later by anatomical closure via endothelial and fibrous tissue proliferation |
|
|
130. Advantages of rofecoxib over an equi-analgesic dose of naproxen include
A. a lower incidence of thrombo-embolic stroke B. greater safety in patients with renal impairment C. a longer duration of action D. less risk of bronchospasm E. less risk of fluid retention and hypertension |
C and D
Product iformation “when established on daily dose eg 1000 mg patients may administer their daily requirements as a single dose as naproxen has been shown to be effective when administered as a single daily dose” ANZCA pain book – cox-2’s do have reduced risk of bronchospasm |
|
|
129. The most INCORRECT statement regarding spinal abscesses is that they present
A. at any age B. without a previous history of infection C. with fever, malaise and back pain D. with spastic paralysis E. with myelogram and CT scan signs of extradural compression |
D
From wiki - references state “flaccid paralysis” initially - Extradural compression if the spinal abscess is an epidural abscess? |
|
|
128. Post-intubation croup in paediatric anaesthesia
A. rarely occurs if uncuffed endotracheal tubes are used B. is reduced if prophylactic steroids are administered infra-operatively C. occurs predominantly in children under the age of five years D. can be treated with one millilitre of aerosolysed 4% racemic adrenaline E. is less frequent if local anaesthetic lubricants are used |
C
A : False is no evidence of difference between cuffed and uncuffed so about 1% - see Bestbet below B : False trend towards reduction but insignificant (Cochrane) C : True the smaller the airway the less narrowing necessary to make significant difference D : False Dose is 1-5ml of 1:1000 (=1-5mg) adrenaline (actually L-adrenaline) in Aus/UK/NZ or 0.5 ml of 2.25% in 3 ml NS (= 11mg of racemic = 5mg L-adrenaline) in US. E : False makes no difference; this is about oedema Contributory Factors Trauma during intubation Tight fitting ETT Coughing on ETT Changing patient's head position while intubated Intubation > 1 hour Operations in neck region pre-existing subglottic stenosis (? Down’s syndrome) Non-Contributory Factors History of upper respiratory infection Presence of upper respiratory infection Cuff on tube - there are large series showing this Humidification Lignocaine (spray or gel) on larynx Gender Treatment of Post Extubation Croup Preventive - identify high-risk patients, consider steroids (Sit up - reduces edema, helps breathing Calm child - reduces peak gas flow Oxygen (humidify) Racemic epinephrine (lasts 1 hour, dose may be repeated, condition may rebound after epinephrine has worn off, patient should be observed for 2 hours post nebulization) |
|
|
126. When the calcium antagonists diltiazem, verapamil and nifedipine are used in patients with stable angina
A. diltiazem causes the greatest depression of atrioventricular nodal conduction B. nifedipine is the most likely to increase the heart rate C. nifedipine causes the least systemic vasodilation D. diltiazem causes the greatest depression of myocardial contractility E. verapamil is the most likely to cause lower limb oedema |
B
Goodman & Gilman's The Pharmacological Basis of Therapeutics: A. diltiazem causes the greatest depression of atrioventricular nodal conduction - false: Verapamil>diltiazem B. nifedipine is the most likely to increase the heart rate - true: HR increases in response to decreased SVR to maintain CO C. nifedipine causes the least systemic vasodilation - false: Nifedipine is a dihydropyridine. "The dihydropyridines are more potent vasodilators in vivo and in vitro than verapamil, which is more potent than diltiazem." D. diltiazem causes the greatest depression of myocardial contractility - false: It is verapamil. "In contrast, in patients with congestive heart failure, intravenous verapamil can cause a marked decrease in contractility and left ventricular function." E. verapamil is the most likely to cause lower limb oedema - false: "The most common side effects caused by the Ca2+ channel antagonists, particularly the dihydropyridines, are due to excessive vasodilation. Symptoms include dizziness, hypotension, headache, flushing, digital dysesthesia, and nausea. Patients also may experience constipation, peripheral edema, coughing, wheezing, and pulmonary edema." |
|
|
125. Acute visual loss following surgery in the prone position is most commonly caused by
A. trauma to the cornea B. compression of the globe C. ischaemia of the visual cortex D. retinal detachment E. ischaemia of the optic nerve |
E
ASA Newsletter 2000: "Ischemic optic neuropathy is the most common diagnosis in postoperative visual loss. Ischemic optic neuropathy is divided into anterior and posterior, depending upon the location of the lesion on the optic nerve. The majority of anterior ischemic optic neuropathy cases occur during cardiopulmonary bypass procedures (53 percent), followed by prone spine cases (12 percent). Most posterior ischemic optic neuropathy cases have occurred during neck, nose or sinus operations (48 percent) followed by prone spine cases (16 percent) and cardiopulmonary bypass procedures (11 percent)" |
|
|
124.A woman has an epidural placed for forceps delivery after a prolonged second stage of labour. The next day she has a right foot drop, and numbness over the anterior part of her lower leg and the dorsal surface of her right foot. The most likely cause is
A. right common peroneal nerve lesion from the use of stirrups in the lithotomy position B. right L5 nerve root lesion from the epidural placement C. right lumbar plexus lesion from compression by the fetal head D. L5 nerve root lesion from a disc protrusion E. transient neurological symptoms (TNS) syndrome |
C
CEACCP article: Most common cause of foot drop is lumbosacral nerve root compression by a big foetal head in the birth canal, potentially forceps also. Common peroneal N less commonly (usually compression in lithotomy position) |
|
|
123. Regarding extracorporeal shockwave lithotripsy (ESWL) for renal calculi in patients with a permanent pacemaker in situ,
A. ESWL is contraindicated B. ESWL pulses should be timed to coincide with the ST interval C. rate modulation of the pacemaker should be deactivated during the ESWL procedure D. there is a risk that the ESWL pulse will reprogramme the pacemaker E. regional anaesthesia is relatively contraindicated |
C
CEACCP - Anaesthesia for patients with pacemakers and similar devices: "Lithotripsy may be used in patients with a pacemaker insitu, but the lithotriptor must be kept at least 6 inches away from the pacemaker. The lithotripsy pulses should be timed with the ECG and rate-modulation should be de-activated" |
|
|
122. Forty patients are randomly dived into two groups - one to receive induction agent A and another to receive induction agent B. The next day they are asked to rate their anaesthetic experience on a scale of 1
(very bad) to 5 (very good). The most appropriate test to compare the anaesthetic experience of the two groups is the A. unpaired t-test B. Mann-Whitney test C. Chi-square test D. Kruskal-Wallis test E. paired t-test |
B
Miles & Gin: "If there is a natural order among categories, so that there is a relative value among them... then the data can be considered ordinal data” "The Mann-Whitney U test is the recommended test to use when comparing two groups that have data measured on an ordinal scale” |
|
|
121. The risk of complications with insertion of a Swan-Ganz catheter is increased in all of the following EXCEPT
A. coagulopathy B. left bundle branch block C. prosthetic right heart valve D. recently inserted endocardial pacemaker leads E. aortic stenosis |
E
coagulopathy obviously inreases risk LBBB (risk of CHB estimated at 5% risk of causing RBBB so theotraical CHB) Right heart vavle – could be damaged and is listed in several places as a relative Recent PPM leads could be dislodged AS patient could decompensate if had an atrial arrhythmia – but not sure the PA cath would actually increase the risk |
|
|
120. In patients undergoing vascular surgery, myocardial ischaemia is most likely to occur
A. in the pre-operative period B. during induction of anaesthesia C. intra-operatively, prior to revascularisation D. in the first 48 hours post-operatively E. 48 to 72 hours post-operatively |
D
Myocardial infarction after vascular surgery: The role of prolonged stress-induced, ST depression-type ischemia. J Am Coll Cardiol 37, 2001: • Article was published at the right time for the 2002 paper • Continuous ECG monitoring of vascular surgery patient up to 72 hrs • 67% of ischaemic episodes within 2 hrs of end of surgery |
|
|
119. The peak effect of oral midazolarn as a premedication in children occurs after
A. 10 - 20 minutes B. 20 - 30 minutes C. 30 - 40 minutes D. 40 - 50 minutes E. 50 - 60 minutes |
B
"The dose of oral midazolam... usually results in a satisfactorily sedated child in approximately 10-15 min with a peak effect occurring at approximately 20-30 min, with minimal to no delay in recovery, even for brief procedures." (Cote, Preoperative preparation and premedication, BJA 1999, 83:16-28) |
|
|
118. In order to decrease the likelihood of causing a pneumothorax when performing a thoracic paravertebral block it is best to
A. use a loss of resistance technique when advancing the needle B. check that the catheter threads easily before injecting the local anaesthetic C. ask the patient to breathhold while advancing the needle D. locate the appropriate transverse process with the needle before advancing deeply E. use a more lateral approach |
D
Thoracic paravertebral block, Anaesthesiolgy 2001: To avoid pneumothorax while performing TPVB it is advised to restrict the needle insertion to 3-4 cm from skin and attempt to strike the bone (transverse process of the corresponding vertebrae). Before advancing the needle any further, if the needle does not meet bone with in this distance then withdraw the needle and reinsert it a cm cephalad or caudad to the initial insertion site Procedure • Insert needle (attached to tubing or syringe) perpendicular to the skin to contact transverse process at 2-4 cm depth. • Then walk off the superior or inferior aspect of the transverse process, until ‘pop’/loss of resistance to saline or air. Loss of resistance is subjective and indefinite. • The needle may be advanced a fixed distance (1-2 cm) without eliciting loss of resistance – very effective and low risk of complications. • Limit insertion to < 2 cm past the transverse process. It is imperative to locate the transverse process before advancing the needle any further to prevent inadvertent deep insertion and possible pleural puncture. • Difficulty is common during catheter insertion, and may require manipulation of needle. Very easy passage may indicate interpleural placement. • Medial redirection not recommended because of risk of neuraxial injection |
|
|
117. A six-week-old baby is booked for elective right inguinal hernia repair. The gestational age is 38 weeks. An appropriate fasting time is
A. 6 hours for breast and formula milk B. 4 hours for solids C. 2 hours for formula milk D. 3 hours for breast milk E. 6 hours for solids and 3 hours for all fluids |
A
RCH Fasting guidelines Children less than 6 months of age: • Please plan for the last breast feed to finish no later than 3 Hours before anaesthesia. • Please plan for a formula or cow's milk feed to finish no later than 4 Hours before anaesthesia. All other patients: • Please do not give milk drinks, food, lollies or chewing gum for 6 Hours before anaesthesia. • Please offer clear fluids up to 2 Hours before anaesthesia NOTE: this is different to the ANZCA day surgery guidelines: • limited solid food may be taken up to six hours prior to anaesthesia and clear fluids totalling not more than 200 mls per hour may be taken up to two hours prior to anaesthesia. • Children over six weeks of age, limited solid food and formula milk may be given up to six hours, breast milk may be given up to four hours and clear fluids up to two hours prior to anaesthesia. • For infants under six weeks, formula or breast milk may be given up to four hours and clear fluids up to two hours prior to anaesthesia. So A correct as per ANZCA guidelines (or D if using RCH) |
|
|
116.A one-month-old infant requires analgesia following simple inguinal hernia repair. The most appropriate paracetamol dosing regimen for the first 48 hours is
Route Loading dose (mg.kg-1) Subsequent doses (mg.kg-1) Maximum daily dose (mg.kg-1.day-1) A. Oral 20 15 45 B. Oral 20 20 90 C. Oral 20 20 60 D. Rectal 20 20 90 E. Rectal 40 20 90 |
C
ANZCA Pain book: Paracetamol dosing in children • Over 6 months: 90 mg/kg/day • Under 6 months: 60 mg/kg/day • 34 wk prem: 45 mg/kg/day |
|
|
115. The most effective treatment for the prevention of early (< 6 hours) post-operative vomiting in adults is
A. omission of nitrous oxide B. droperidol 0.5 mg IV (intravenously) intra-operatively C. a propofol induction D. ondansetron 4mg IV intra-operatively E. a propofol TIVA (total intravenous anaesthesia) technique |
E
From SAMBA trial: - Propofol induction/maintenance (NNT 5) - Ondansetron NNT6 (Vomiting), NNT7 (Nausea) - Droperidol (with PCA) NNT 3, without NNT 5 - Haloperidol (NNT 4-6) - Transdermal scopolamine (NNT 6) - TENS, Acupuncture, Acupressure (NNT5) |
|
|
114. Side effects or complications of coeliac plexus block using a neurolytic agent include all of the following EXCEPT
A. hypotension B. paraplegia C. intestinal hypermotility D. pneumothorax E. retroperitoneal haematoma |
Can all happen
Miller: "Side effects associated with celiac plexus blockade include hypotension; spinal, epidural, or intravascular injection; pneumothorax; puncture of viscera, such as the kidney, ureter, or gut; and retroperitoneal hematoma." Diarrhoea common (i.e. intestinal hypermotility) |
|
|
113. Propofol for induction and maintenance of anaesthesia in healthy children, compared to healthy adults, has
A. a larger central volume of distribution B. a lower total body clearance C. the same context sensitive half-time D. a more rapid awakening time E. a lower infusion rate requirement |
A
Stoelting: “Children require higher induction doses of propofol on a mg/kg basis, presumably reflecting a larger central distribution volume and higher clearance rate" • ↑ Central Vd • ↑ Elimination / Total Body Clearance • ↑ CSHT / Wake Time • ↑ Induction Dose & Infusion Rates |
|
|
112. The best estimated incidence of post-operative nausea and vomiting in adult patients undergoing inhalational anaesthesia who are female, non-smokers and have a history of motion sickness is
A. 30% B. 45% C. 60% D. 80% E. 95% |
C
Apfel Risk Index • Risk factors o Female o Non smoker o History of PONV or motion sickness o Post-op opioid analgesia To calculate PONV Incidence • 10% if no risk factors • 20% for each risk factor (i.e. see below) Risk Factors Present Vs Incidence of PONV • Nil => 10% • 1 => 21% • 2 => 39% • 3 => 61% • 4 => 79% |
|
|
111. Electrocardiographic changes in acute hyperkalaemia include
A. the appearance of a J wave B. loss of P waves C. flattening of the T wave D. a prominent U wave E. a prolonged QT interval |
B
• J-wave is with hypothermia • UptoDate: "Hyperkalemia may be associated with a variety of changes on the ECG . Tall peaked T waves with a shortened QT interval are usually the first findings . As the hyperkalemia gets more severe, there is progressive lengthening of the PR interval and QRS duration, the P wave may disappear, and ultimately the QRS widens further to a sine wave pattern. Ventricular standstill with a flat line on the ECG ensues with complete absence of electrical activity." • Peaked not flattened T waves • U waves seen with hypokalaemia • QT shortened not lengthened |
|
|
110. The h wave is seen on the CVP (central venous pressure) waveform
A. following the x descent, prior to the v wave B. during tachycardia C. following the y descent, prior to the a wave D. with tricuspid regurgitation E. with pericardial restriction |
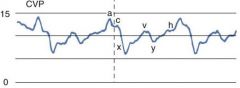
C
Miller: A final component of the CVP waveform, the h wave, occasionally appears as a pressure plateau in mid to late diastole. The h wave is not normally seen unless the heart rate is slow and venous pressure is elevated |
|
|
109. In pre-eclampsia
A. once delivery of the placenta takes place, the condition improves B. in the absence of other risk factors, a platelet count of greater than 50 x 109.1-1 is adequate for epidural anaesthesia C. corticosteroid therapy has no effect on the severity of thrombocytopaenia D. magnesium sulphate halves the risk of eclampsia E. spinal anaesthesia is contraindicated |
D
• Still at risk of eclampsia post delivery • Obstetric Anaesthesia Scientific Evidence from ANZCA gives 75 as a safe figure • Apparently steroids do improve platelet counts • MAGPIE trial (Do women with pre-eclampsia, and their babies, benefit from magnesium sulphate? The Magpie Trial: a randomised placebo-controlled trial) – risk of eclampsia decreased by 50% with magnesium • Spinal not contraindicated |
|
|
108. This ECG tracing was obtained pre-operatively from an 84 year old patient. It most likely represents
A. first degree heart block B. complete heart block C. nodal rhythm D. Wolff-Parkinson-White (WPW) syndrome E. Mobitz type II block |
B
|
|
|
107. Glycine, if absorbed into the circulation in large amounts during transurethral prostatic (TURP) surgery, may cause any of the following EXCEPT
A. an elevated serum ammonia B. hyponatraemia C. disseminated intravascular coagulation D. restlessness E. temporary blindness |
C
A. an elevated serum ammonia - true: "Absorption of glycine may result in CNS toxicity as a result of oxidative biotransformation of glycine to ammonia. [93] [94] In a report of delayed awakening after TURP in three patients,[93] an association with elevated blood ammonia concentrations was noted." (Miller Ch 65) B. hyponatraemia - true: "Transurethral resection of prostate (TURP) syndrome is a recognized cause of hyponatremia (see Chapter 65 ). TURP syndrome is caused by intravascular absorption of irrigation solution, which typically contains glycine, but no other electrolytes.[16] The absorption of free water causes hyponatremia because of the dilution of serum sodium" (Miller Ch 54) C. disseminated intravascular coagulation - FALSE D. restlessness - true E. temporary blindness - true |
|
|
106. The most likely cause of superior vena cava syndrome is
A. bronchogenic carcinoma B. mesothelioma C. thymoma D. teratoma E. apical pulmonary bullae |
A
Harrison’s: Lung cancer is the underlying process in approximately 85% of the patients with SVC syndrome |
|
|
105. In relation to obstetric haemorrhage
A. amniotic fluid embolism is unlikely to present as unexplained haemorrhage B. coagulopathy is uncommon, when severe abruption leads to maternal shock and fetal death C. the risk of placenta accreta, but NOT placenta praevia, increases with an increasing number of caesarean sections D. treatment of uterine atony with prostaglandins is rarely associated with adverse maternal effects E. intravenous magnesium may facilitate replacement of an inverted uterus |
E
"Uterine relaxation may be necessary to replace the uterus; β-sympathomimetic agents, magnesium, and nitroglycerin all have been used to achieve this goal." (Miller 7th ed Ch 69) |
|
|
104. Significant differences between the LMA-ProSealTm and the standard laryngeal mask (LMA-ClassicTm) include all of the following EXCEPT
A. an independent oesophageal drain tube B. a double cuff arrangement C. a built in bite-block D. an improved seal pressure at a given cuff pressure E. improved aperture bars to prevent the epiglottis occluding the airway tub |
E
Proseal product information. Added features: • A softer silicone cuff reducing the likelihood of throat irritation and stimulation • High seal pressure - up to 30 cm H20 - Providing a tighter seal against the glottic opening with no increase in mucosal pressure – (this is provided by the 2nd cuff – the bump at the back) • A built-in drain tube designed to channel fluid away and permit gastric access for patients with GERD or during extended cases where endotracheal intubation is not required |
|
|
103. First-line therapy for trigeminal neuralgia is
A, carbamazepine B. amitriptyline C. mexilitene D. gabapentin E. baclofen |
A
ANZCA pain book: “Carbamazepine is effective in the treatment of trigeminal neuralgia” |
|
|
102. Each of the following is a complication of loop diuretic treatment EXCEPT
A. hypokalaemia B. hyponatraemia C. hypermagnesaemia D. irreversible sensori-neural deafness E. metabolic alkalosis |
C
Yentis: "Loop diuretics: May cause hypokalaemia, hyperuricaemia, hypomagnesaemia and hyperglycaemia. Damage to 8th cranial nerve may occur following rapid IV injection and with concurrent aminoglycoside therapy." Causes a hypochloraemic metabolic alkalosis |
|
|
101. Thiazide diuretics may cause
A. hypernatraemia B. precipitation of acute gout C. hypoglycaemia D. hyperkalaemia E. hepatic failure |
B
Yentis: "Side effects include hypokalaemia, hyponatraemia, hyperuricaemia, hypomagnesaemia, hypochloraemic alkalosis, hyperglycaemia, hypercholesterolaemia, exacerbation of renal and hepatic impairment, impotence, and rarely rashes and thrombocytopaenia." |
|
|
100. Compared to a normal adult, in the neonate
A. functional residual capacity (FRC) is a more efficient buffer to changes in partial pressure of inspired gases B. closing volume in ml.kg-1 is lower C. oxygen consumption in ml.kg-1 is similar D. FRC in ml.kg-1 is higher E. the ratio of alveolar ventilation to FRC is higher |
E
|
|
|
99. Aortic dissection is most commonly seen in association with
A. atherosclerosis B. blunt chest trauma C. chronic renal failure D. Marfan's syndrome E. hypertension |
E
Stoelting: “Systemic hypertension is the most important risk factor for thoracic aortic dissection” Four major inherited disorders are known to affect major arteries: • Marfan syndrome (1/3 of marfans get dissection), Ehlers-Danlos syndrome, bicuspid aortic valve, and nonsyndromic familial aortic dissection Other associations: • Blunt Trauma (usually deceleration injury) • Men > women • Approximately half of all aortic dissections in women younger than 40 years of age occur during pregnancy, usually during the third trimester • Iatrogenic – eg. Aortic cannulation |
|
|
98. Peri-operative hypothermia in the elderly is associated with
A. an increase in post-operative cardiac morbidity B. no change in the risk of infection C. a decrease in the circulating noradrenaline concentration D. a decrease in hospital stay E. a decrease in blood loss during hip replacement surgery |
A
Br J Anaesth 2001; 87: 608–24 Minimizing perioperative adverse events in the elderly: “Perioperative hypothermia is prevalent in both young and elderly surgical patients, but more frequent, pronounced and and prolonged in the elderly who have compromised ability to regain normal thermoregulatory control quickly. In the early postoperative period, mild hypothermia can elevate norepinephrine concentrations and increased peripheral vasoconstiction and arterial blood pressue, thereby contributing to cardiovascular ischemia and arrhythmia. Mild hypothermia may also increase blood loss during total hip replacement procedures and risk of wound infection, decrease drug metabolism, and prolong hospitalization.” |
|
|
97. In relation to intra-arterial drug injection
A. aberrant branches of the radial artery are found in approximately 1% of individuals B. propofol is reported to cause significant adverse effects C. there is an increased incidence of inadvertent arterial cannulation near the anatomical snuffbox and the antecubital fossa D. midazolam causes severe vasoconstriction and endothelial damage E. metoclopramide is likely to cause intense vasospasm and endothelial damage because of its low pH and metabisulphite preservative |
C
Anaesthesia and Analgesia 95(2), Aug 2002, p487-491: 1% have aberrant radial artery – but this is talking about aberrant branch? Anesth Analg, Volume 103(3).September 2006.792-794: • Midazolam has little side effect on IA injection. • Propofol cause hyperemia and diastal blanching, but I won't call it "very dangerous". So we can rule out B&D Metoclopramide causes both vasoconstriction DA2 antag and vasodil 5HT2 antag. Nothing else mentioned in article about preservative |
|
|
96. The correct ranking of fat/blood partition co-efficients, in order of increasing solubility in fat, for sevoflurane (S), isoflurane (I), desflurane (D) and nitrous oxide (N20) is
A. N2O < D < S approx = I B. N20 approx = D < S < I C. N20 < S < D < I D. D < N20 < S < I E. D < N20 approx = S < I |
A
Table 1-7 p24 of Stoelting: Nitrous 2.3 Desflurane 27.2 Isoflurane 44.9 Sevoflurane 47.5 |
|
|
95. An 89 year-old female is admitted for same day cataract extraction and intra-ocular lens placement. Admission observations include a blood pressure of 160/95 mmHg and a pulse rate of 90 beats.min-1. Following topical administration of 2 drops of 10% phenylephrine to dilate the pupil, the blood pressure is 215/120 mmHg and the pulse 85 beats.min-1. The most appropriate treatment is intravenous
A. clonidine B. hydralazine C. esmolol D. phentolamine E. verapamil |
D
B also seems right, but is of slower onset than phentolamine New York State Guidelines on the Topical Use of Phenylephrine in the Operating Room Anesthesiology 2000;92(3). Summary: 1. The initial dose of phenylephrine for adults should not exceed 0.5 mg (four drops of a 0.25% solution). This dosage is based on the product insert for the intravenous administration of phenylephrine for the treatment of mild/moderate hypotension. This dosage assumes 100% absorption of the administered phenylephrine. In children (up to 25 kg), the initial dose should not exceed 20 micro-g/kg. 2. The minimal amount of phenylephrine needed to achieve vasoconstriction should be administered. BP and pulse should be closely monitored after phenylephrine is given. 3. The dose of phenylephrine should be administered in a calibrated syringe and should be verified by a physician. 4. The anesthesiologist should be aware of all medications that are administered to the patient perioperatively. 5. Mild-to-moderate hypertension resulting from phenylephrine use, in a healthy individual, should be closely monitored for 10-15 min before antihypertensive medications are given. Severe hypertension, as well as its adverse effects such as electrocardiographic changes or pulmonary edema, must be treated immediately. Antihypertensive agents that are direct vasodilators or alpha-receptor antagonists are appropriate treatments. 6. The use of beta-blockers and calcium-channel blockers should be avoided when vasoconstrictive agents such as phenylephrine are used in the operating room. Case reviews, as well as a review of the medical literature, suggest that the use of beta-blockers, and potentially calcium- channel blockers, as treatment of hypertension secondary to a vasoconstrictor may worsen cardiac output and result in pulmonary edema. 7. If a beta-blocker is used for the treatment of resulting hypertension, glucagon may be considered to counteract the loss of cardiac contractility as well as other standard therapies |
|
|
94. Acute reactions to drugs are unlikely with
A. acute intermittent porphyria B. plumboporphyria C. variegate porphyria D. porphyria cutanea tarda E. hereditary coproporphyria |
D
Porphyrias: • Acute: acute intermittent porphyria (AIP); variegate porphyria (VP); hereditary coproporphyria (HC); plumboporphyria (PP) • Non-acute: porphyria cutanea tarda (PCT); erythropoietic porphyrias: congenital erythropoietic porphyria (CEP); erythropoietic protoporphyria (EPP) |
|
|
93. Immunologically mediated heparin-induced thrombocytopaenia is characterised by
A. onset within a few days of first starting heparin therapy B. intravascular thromboses C. platelet count rarely reduced below 100 x 109.1-1 D. continuation of thrombocytopaenia after cessation of heparin E. presence of non-specific (heparin-independent) platelet antibodies |
B
• Stoelting: “In patients receiving heparin for more than 5 days, antibodies to the heparin-platelet factor 4 complex can form, which are capable of binding to platelet Fc receptors and inducing platelet activation and aggregation." • "In vivo, this leads to both an increased clearance of platelets with resultant thrombocytopenia and venous and/or arterial thrombus formation, with the potential for severe organ damage (loss of limbs, stroke, myocardial infarction) as well as unusual sites of thrombosis (adrenal, portal vein, skin)." • Can certainly be lower than 100 • Not sure about this one • They are heparin dependent antibodies |
|
|
92. The most significant predictor for inotrope requirement to wean a patient from cardiopulmonary bypass is
A. use of warm cardioplegia B. insulin dependent diabetes mellitus C. an elevated creatinine D. cardiomegaly on chest X-ray E. left main coronary artery disease |
C
Incidence and risk calculation of inotropic support in patients undergoing cardiac surgery with cardiopulmonary bypass using an automated anaesthesia record-keeping system. BJA 2002: Factors with significant influence on the use of positive inotropic drugs: • age, gender, weight, congestive heart failure, myocardial infarction, ejection fractions, renal failure, COPD, preoperative use of diuretics, digitalis and ß-adrenergic blockers, type of surgery, duration of surgery, CPB time, aortic cross-clamping time and reperfusion time Factors not influencing use of positive inotropic drugs: • height, BMI, left main coronary artery disease, history of hypertension, diabetes mellitus, long-term therapy with ACE inhibitors, calcium-blocking drugs, nitroglycerin and antidysrhythmic drugs A lot of people on wiki think D (reasoning that cardiomegaly = heart failure) |
|
|
90. The Mallampati classification of the airway using the view of the faucial pillars, the soft palate and the uvula obtained with the tongue protruding, is
A. validated in both children and adults B. is associated with a high false positive rate for difficult laryngoscopy C. NOT applicable to edentulous patients D. useful for choosing the size of endotracheal tube E. associated with a positive predictive value of approximately 90% |
B
|
|
|
89. The most reliable clinical sign to demonstrate reversal of neuromuscular blockade is
A. ability to abduct an arm to shoulder level. B. a normal vital capacity. C. a maximum inspiratory pressure of minus 25 cm H20 D. a sustained hand grip for 5 seconds E. protrusion of the tongue |
D
Sustained head lift and Sustained hand grip are best clinical signs Inspiratory pressure needs to be -50cm H20 |
|
|
88. Negative pressure pulmonary oedema
A. does NOT typically occur in young patients B. is manifest by clinical signs different to other causes of pulmonary oedema C. is usually associated with cardiomegaly on chest X-ray D. responds well to supportive therapy, avoiding intubation in the majority of cases E. needs to be followed up by a physician |
D
|
|
|
86. A recently published large Australian multicentre trial of patients undergoing major abdominal surgery (The MASTER Trial) concluded that the use of epidural anaesthesia (with general anaesthesia) and postoperative epidural analgesia, compared with general anesthesia alone, was associated with a decrease in
A. mortality at 30 days B. both mortality at 30 days and adverse cardiovascular events C. both mortality at 30 days and respiratory failure D. adverse cardiovascular events E. respiratory failure |
E
MASTER Trial “In a primary analysis of a large recently completed randomized trial in 915 high-risk patients undergoing major abdominal surgery, we found no difference in outcome between patients receiving perioperative epidural analgesia and those receiving IV opioids, apart from the incidence of respiratory failure” |
|
|
85. When assessing a patient with unstable angina, the clinical feature most predictive of an adverse short-term outcome (death or myocardial infarction within 6 months) is
A, increased angina frequency or severity B. angina provoked at a lower threshold of exercise C. new onset angina on effort D. an angina episode lasting more than 10 minutes E. age less than 65 years |

C
ACC/AHA guidelines for Mx of unstable angina & NSTEMI: So by these: • A, B and D are all low risk • Age >70 associated with intermediate risk and age >75 for high risk • C correct if this is Class III or IV angina |
|
|
84. The absorption of fluid into the circulation during transurethral prostatectomy (TURP) is NOT related to
A. prostate size B. height of the irrigation fluid bag C. duration of surgery D. surgical technique E. type of irrigation fluid |
E
The Internet Journal of Anesthesiology 1999; Vol3: "Several factors contribute to the rapid volume expansion, namely the intravesicular pressure (governed by the height of the irrigation bag above the prostatic sinuses), the number of prostatic sinuses opened and maybe most important the duration of the surgical procedure“ Transurethral Resection of the Prostate (TURP) Syndrome: A Review of the Pathophysiology and Management. Anesth & Analg 1997: “using continuous irrigating resectoscopes or suprapubic trocar drainage can minimize absorption” |
|
|
82. Of the following situations, the strongest contraindication to retrobulbar anaesthesia is
A. an operative eye axial length of 24 mm B. a staphyloma of the operative eye C. warfarin for embolism prophylaxis in a patient in atrial fibrillation D. treated glaucoma E. a vitreous humour biopsy for diagnosis and treatment of enophthalmitis |
B
• A is fine • B is a worry, there is more likelihood of globe perforation (staphyloma is an out-pouching of the globe resulting from pathological thinning of the sclera, choroid and retina) • C is a bit of a worry, as retrobulbar haemorrhage is one of the commoner complications with RBB, but usually this isn’t a problem with eye blocks. • D don’t think so • E sounds bad, but in actual fact, the needle is not going through infection, the infection is IN the eye. Wiki seems to lean toward B |
|
|
81. Recognised weaknesses of systematic reviews include all of the following EXCEPT
A. publication bias B. duplicate publication C. study heterogeneity D. inclusion of outdated studies E. systematic review author bias |
E
Myles & Gin: “In using a rigorous process to determine what types of studies will be included in a systematic review, author bias is usually eliminated” |
|
|
80. Twenty-four hours following a vaginal hysterectomy, a 48-year-old obese female complains of severe pain that radiates down both buttocks and thighs. She had received a spinal anaesthetic with hyperbaric lignocaine. The most likely explanation for these complaints is
A. transient neurological symptoms syndrome B. lumbar disc herniation C. a spinal abscess D. trauma due to improper positioning E. a spinal haematoma |
A
• Most likely • why would they suddenly have disc herniation? • Too early for spinal abscess • Why would a positioning problem suddenly present 24hrs after? • Haematoma - possibly |
|
|
79. The single most important treatment in preventing acute renal failure following crush injury is
A. maintenance of an alkaline urine (pH > 6) to prevent cast formation B. maintenance of adequate urine output with mannitol C. vigorous intravascular fluid replacement D. administration of xanthine oxidase inhibitors to prevent hyperuricaemia E. emergent dialysis to remove myoglobin from the circulation |
C
Treatment focuses on preventing myoglobin precipitation in the urine by maintaining a brisk alkaline diuresis. Immediately administer saline to patients with volume depletion. Follow-up with mannitol to induce diuresis, supported by adequate IV fluids. Raising the pH of the urine to 6.5 or more can be facilitated by adding sodium bicarbonate to the fluids. |
|
|
76. The observed fall in cardiac output induced by carbon dioxide
pneumoperitoneum during laparoscopic cholecystectomy is primarily a result of A. a fall in venous return to the heart B. reflex bradycardia C. an increase in systemic vascular resistance D. head-up tilt of patient E. increased pulmonary vascular resistance |
A
|
|
|
75. The intercostal nerves
A. arise as the sensory fibers of the anterior primary rami from their spinal segments B. give off a lateral cutaneous branch at the angle of the rib C. lie in the subcostal groove in only 50% of patients D. lie between the intercostalis intimi muscle and the pleura E. are enclosed in a dural sheath from their origin to the angle of the rib |
C
• They are also motor • AFA: “Each nerve gives off a lateral cutaneous branch in the mid-axillary line” • Classically the intercostal nerve does run in subcostal groove (NYSORA). BJA 1988 ANATOMICAL VARIATION IN THE POSITION OF THE PROXIMAL INTERCOSTAL NERVE: o “Anatomical study of the proximal intercostal nerve in cadavers revealed three nerve forms, depending on the relation between the nerve and adjacent ribs. This was found in the classical subcostal position in 16.6%, in the midzone in 73% and in the inferior supracostal position in 10%.” • False, lie between the innermost and next intercostal muscle • False, variable amount of dural sheath coverage |
|
|
74. Problems with aprotinin (Trasylol) use during coronary artery surgery (utilising cardiopulmonary bypass) include all of the following EXCEPT
A. increases in creatinine levels B. prolongation of the activated clotting time (using celite as the activator) C. increased incidence of cerebrovascular accidents D. anaphylaxis E. graft thrombosis |
C
• N Engl J Med. 2006 Jan 26 : “use of aprotinin was associated with a doubling in the risk of renal failure requiring dialysis among patients undergoing complex coronary-artery surgery” • Aprotinon does prolong the ACT (i.e. without the patient actually being anticoagulated) • Aprotinin may infact decrease the incidence of stroke. BestBets - Does use of aprotinin decrease the incidence of stroke and neurological complications in adult patients undergoing cardiac surgery?: o “There is evidence from three meta-analyses and two more recent RCTs that the use of aprotinin is associated with decreased incidence of stroke and neurological complications in some patients undergoing cardiac surgery” • Aprotinin can cause anaphylaxis • Initial data suggested aprotinin may increased graft thrombosis but this has since been proven wrong. Anaesthesiology Volume 93(1) July 2000: “Initial concerns that aprotinin might cause an increase in graft occlusion rate or myocardial infarction have recently been found to be unjustified” |
|
|
71. The amount of fluid drawn into the vascular space when 100 ml of 25% albumin is administered intravenously is
A. 125 ml B. 250 ml C. 350 ml D. 450 ml E. 625 ml |
C
Stoelting: "Administration of hypertonic albumin will draw 3 to 4 ml of fluid from the interstitial space into the intravascular space for every 1ml of albumin administered". |
|
|
68. When providing general anaesthesia to a patient with a history of asthma
A. thiopentone should NOT be used as it may cause bronchospasm B. intravenous and topical tracheal lignocaine are equally effective in preventing bronchial hyperreactivity C. ketamine provides little benefit in a patient with active wheezing D. induction with propofol is effective in reducing the incidence of wheezing following intubation E. isoflurane is as effective a bronchodilator as halothane when given in MAC equivalent doses |
D
|
|
|
66. A patient taking cyclosporine after renal transplantation is UNLIKELY to have
A. macrocytic anaemia B. interstitial renal fibrosis C. hypertension D. peripheral neuropathy E. suppression of humoral immunity |
A
Used to treat macrocytic anaemia of various origins. Can cause anaemia to, but aplastic not macrocytic Does causes interstitial renal fibrosis (Clin Anaes pl 1367). Does causes hypertension (Stoelting as above, Clin anaes also). Does cause periphipheral neuropathy (see Stoelting ref) Supresses T-lymphocyte involvement in both cellular and humoral immunity |
|
|
56. Side effects of digoxin are increased by
A. hyperthyroidism B. hypocalcaemia C. hyperkalaemia D. hypermagnesaemia E. hypothyroidism |
E
Factors that can precipitate digitalis toxicity, even in the therapeutic range, by increasing myocardial digitalis sensitivity: hypokalemia hypomagnesemia myocardial disease old age hypothyroidism ther metabolic disturbances (hypoxemia, acid-base abnormalities, hypercalcemia, and hypernatremia) |
|
|
52. A thromboelastograph (T.E.G.) result on a 64 yr old female having a portacaval bypass operation is reported as
Coagulation time (r k) 20 min (N 10 - 12 min) Maximum Amplitude (MA) 30 mm (N 50 - 70 mm) Clot formation rate 35 degrees (N > 50 degrees) These results suggest A. a defect of the intrinsic system only B. six units of fresh frozen plasma would correct the defect C. the T.E.G. should be repeated with epsilon-aminocaproic acid added to the specimen D. the presence of increased fibrinolysis E. possible heparin contamination of the specimen |
E
The there is certainly a factor deficiency, but there could also be platelet deficiency so B is probably false |
|
|
44. The plasma half-life of low molecular weight heparin is
A. increased in conditions with raised plasma proteins B. 2 to 4 times that of unfractionated heparin C. much less predictable than unfractionated heparin D. dependent upon a saturatable mechanism for clearance E. longer than unfractionated heparin because of a higher affinity for plasma protein |
B
LMWH’s Higher bioavailability Bioavailability is greater. Protein binding is much less compared to unfractionated heparin, giving superior bioavailability at lower doses. Not fully reversible with protamine unlike unfractionated heparin Less HITS and less platelet function affect Longer T 1/2 and more predictable kinetics clearance by first order kinetics, through the renal route |
|
|
43. The antibiotic LEAST likely to be effective for the management of anaerobic peritonitis is
A. carbenicillin B. cefoxitin C. cephalothin D. chloramphenicol E. clindamycin |
C
Bacteroides fragilis and Clostridium perfringens are commonly implicated in anaerobic infections. Both these bugs are sensitive to cefoxitin, clindamycin and chloramphenicol and demonstrate some sensitivity to carbenicillin |
|
|
41. Anaemia in chronic renal failure is characteristically
A. due to haemolysis in the renal vascular bed B. normochromic and microcytic C. due to defective haemoglobin synthesis D. responsive to iron and folate therapy E. associated with increased 2,3-DPG levels in blood cells |
E
Anaemia leads to increased 2.3DPG (to increased O2 offloading) |
|
|
39. The neural structure LEAST likely to be injured during attempted cannulation of the internal jugular vein at the level of the cricoid cartilage, using an anterior approach, is the
A. ansa cervicalis B. cervical plexus C. phrenic nerve D. recurrent laryngeal nerve E. vagus nerve |
B and D
Ansa cervicalis lies on carotid sheath so is at risk Cervical plexus is at C1-4, cricoid at C6, so probably too low to hit cervical plexus Phrenic and vagus are at risk AFA: “The recurrent laryngeal nerve on the right side leaves the vagus as the latter crosses the right subclavian artery; it then loops under the artery and ascends to the larynx in the groove between the oesophagus and trachea” o Seems impossible to hit if it is running between trachea and oesophagus, but perhaps lower down as it crosses the clavicle? |
|
|
34. Detrimental effects of hypothermia associated with general anaesthesia in the elderly do NOT include
A. reduced elimination of anaesthetic agents B. prolonged awakening C. increased body metabolism D. hypercoagulability E. shivering |
D
|
|
|
19. The sciatic nerve is located midway between the greater trochanter and the
A. iliac crest B. ischial tuberosity C. ischial ramus D. symphysis pubis E. tip of the coccyx |
B
Anatomy for anaesthetist: "The sciatic nerve leaves the posterior pelvic wall through the greater sciatic foramen below piriformis and enters the region of the buttock very slightly medial to the half-way point between the ischial tuberosity and the greater trochanter." |
|
|
18. Following nerve injury involving
A. axonotmesis, full recovery of function of the nerve can be expected in a few days B. neurapraxia, regrowth of the axon occurs from the node of Ranvier proximal to the injury C. neurotmesis, full functional recovery is very unlikely D. complete severance, the affected muscles no longer respond to any form of electrical stimulation E. the division of a nerve in a contaminated wound, immediate suture is essential |
C
"Axonotmesis is the disruption of axons and myelin. The surrounding connective tissues, including endoneurium, are intact. The axons degenerate proximally and distally from the area of injury. Axon regeneration within the connective tissue pathways can occur, leading to restoration of function. Axons regenerate at a rate of 1 mm per day. Significant functional recovery may occur for up to 18 months." (From Schwartz) "Neurapraxia is defined as the temporary failure of nerve function without physical axonal disruption. Axon degeneration does not occur. Return of normal axonal function occurs over hours to months, often in the 2- to 4-week range." (From Schwartz) "Neurotmesis is the disruption of axons and endoneurial tubes. Peripheral collagenous components, such as the epineurium, may or may not be intact." It is more severe than axonotmesis which definitely has connective tissue intact. Denervated muscle will still respond to electrical stimulation. Delayed suturing can be performed |
|
|
16. Urinary osmolality
A. in the presence of oliguria is a good indicator of renal function B. will increase more than specific gravity with an osmotic diuresis due to glucose C. is measured by elevation of the freezing point D. is expressed in milliosmo1.11 E. in severely ill patients gives an indication of the effectiveness of frusemide |
A
• ATN leads to tubular dysfunction and inability to conc. Urine. It will help distinguish pre-renal from renal failure (ie, urine will be concentrated in oliguric prerenal failure), whereas in renal failure, there may be failure to concentrate the urine. • Specific gravity is the ratio of the density of a substance to the density of water. There is a disproportionate increase in specific gravity compared to osmolality if larger molecules (e.g glucose), are present (i.e in glucosuria in uncontrolled DM, and the administration of radiocontrast media) (from UptoDate) • Measured by freezing point depression osmometer • Molality = mol/Kg, Molarity – mol/L |
|
|
15. The first cervical vertebra has
A. two spinous processes B. an odontoid process C. no anterior tubercle D. a facet on its anterior arch E. no foramen transversarium |
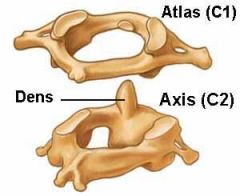
D
Has an articular facet for the dens on posterior aspect of anterior arch. Has an anterior tubercle. Has a posterior tubercle instead of spinous process. Has a transverse foramen on each side. Odontoid process = dens, so on C2. |
|
|
13. The risk of seroconversion after a needlestick injury, with a hollow
needle from a HIV positive patient, is A. 30% B. 15% C. 3% D. 0.3% E. 0.03% |
D
From Miller |
|
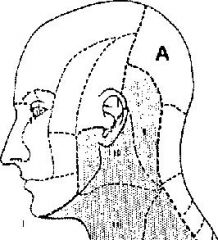
12. The cutaneous nerve supplying the territory marked 'A' in the figure below is
A. the greater occipital nerve (a branch of the posterior primary ramus of C1) B. the greater occipital nerve (a branch of the posterior primary ramus of C2) C. the lesser occipital nerve (a branch of the posterior primary ramus of C2) D. the lesser occipital nerve (a branch of the anterior primary ramus of C2) E. the third occipital nerve |
B
|
|
|
11. The percentage of the population which is heterozygous as regards pseudocholinesterase, thus having a dibucaine number between 30 and 80, is
A. 0.04% B. 0.4% C. 4.0% D. 14.0% E. 40.0% |
C
Normal 96% Heterozygous 4% Homozygous 0.04% |
|
|
9. A patient with a central dislocation of the hip following a motor car accident is noted to be shocked on admission one hour after the accident. The most likely cause is
A. ruptured bladder B. fat embolism C. ruptured urethra D. neurogenic shock E. none of the above |
E
Apparently a central dislocation is actually a fracture-dislocation, where lateral impact on trochanter smashes head medially through acetabulum. Therefore haemorrhage is more likely cause |
|
|
8. If a patient experiences parasthesia in the little finger during supraclavicular brachial plexus block, the needle is in proximity to the
A. posterior cord B. middle trunk C. ulnar nerve D. lower trunk E. medial cord |
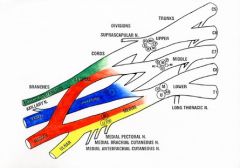
D
Sensation in this area is C8distribution, supplied by the ulnar nerve, medial cord, lower trunk Supraclavicular block targets the trunks however: NYSORA: “The block is performed at the level of the distal trunks and origin of the divisions, where the brachial plexus is confined to its smallest surface area” |
|
|
7. Carbon monoxide poisoning results in hypoxic damage by
A. reducing the arterial P02 B. shifting the oxygen-haemoglobin dissociation curve to the right C. decreasing alveolar ventilation D. reducing the number of oxygen sites available on haemoglobin E. uncoupling oxidative metabolism and ATP production |
E
Almost repeat Does bind to cytochrome C to affect oxidative metabolism – but is this the primary means of hypoxic damage – maybe so |
|
|
5. Low molecular weight heparin
A. has a similar ratio of antithrombotic to anticoagulant activity as normal heparin B. has a lower antifactor Xa activity than normal heparin C. has a higher antifactor IIa activity than normal heparin D. is prepared by fractionation of normal heparin E. anticoagulant effect can be monitored by activated clotting time and aPPT |
D
A is asking abour the X :II ratios . thrombosis is in vivo and involves platelets, coagulation is just the pathway. For options A, B & C Stoelting: “Enoxaparin has an antiactivated factor X to antiactivated factor II ratio of 4:1, compared to 1:1 with heparin” MIMS "In comparison with natural heparin, Clexane is characterised by a clear increase in the ratio between anti-Xa and anti-IIa activities, which is always greater than four." D: "These drugs are derived from the depolymerisation of heparin by either chemical or enzymatic degradation." Peck, Hill & Williams |

