![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
63 Cards in this Set
- Front
- Back
|
What is the prevalence of retinal detachments? |
• Relatively rare (9 per 100000 cases) • Detachment bilateral in 10-30% of cases |
|
|
When does retinal detachment incidence increase? |
Incidence increases with age |
|
|
What is the prognosis of retinal detachment? |
Good with early detection |
|
|
How is retinal detachment classified? |

Primary rhegmatogenous = break
Secondary tractional or exudative |
|
|
What are the symptoms of retinal detatchment? |
• Sudden onset of or an increase in the number of floaters (tobacco dust). • Sudden shower of floaters like small insects. • Sudden onset flashes of light or a change in the pattern of flashes normally seen or flashes of light that do not go away. • Sudden change in vision. • Any loss of peripheral vision when one eye is covered. • The appearance of a curtain or discolouration over your vision |
|
|
What is a retinal detachment? |
Separation of the neurosensory retina from the retinal pigment epithelium (RPE) by subretinal fluid (SRF). |
|
|
What is a Tractional detachment? |

Detachment of vitreous by fibro-proliferative strands |
|
|
What is a Exudative or serous detachment? |
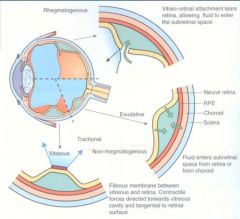
Accumulation of fluid under retina without an associated retinal break |
|
|
What is a Rhegmatogenous detachment? |

Accumulation of liquefied vitreous / fluid under retina following a retinal break. |
|
|
What are the symptoms with Tractional Retinal Detachment? |
• Usually asymptomatic unless encroaching on posterior pole • Sudden abrupt loss of visual acuity |
|
|
What are the signs with Tractional Retinal Detachment? |

• Vitreal strands and membranes • Concave, smooth-surfaced detachment • Dense and immobile detachment • RAPD • Visual field defect |
|
|
What should you do with a Tractional Retinal Detachment? |
Needs rapid referral to eye casualty, normally ring eye casualty and send direct that day. |
|
|
What is Exudative Retinal Detachment in association with? |
Occur in association with subretinal disorders that damage the RPE layer
• choroidal neoplasms • posterior scleritis • congenital optic disc anomalies (optic pits, morning glory syndrome) • Coat's disease |
|
|
What would be seen with a Exudative Retinal Detachment? |

• Photopsiae ( flashing lights) are not usually noticed. • May have sudden visual field defect. • Metamorphopsia if near to fovea. |
|

What is this? |
Coats disease |
|
|
What is coats disease? |
Coats’ disease is an abnormality of the blood vessels in the retina.
Bloody vessels may leak which means that fluid can leave the vessels, becoming trapped within, and sometimes underneath, the retina causing it to lift up. |
|
|
What ia the prevalence of Rhegmatogenous Retinal Detachment? |
• 1:10,000 of the population each year • Both eyes involved 10% - Not at the same time |
|
|
What causes Rhegmatogenous Retinal Detachment? |
• Dynamic vitreoretinal traction • Predisposing retinal degeneration • High myopia |
|
|
What are the predisposing retinal detachment factors |
• Lattice degeneration - present in 40% of RD • Retinal thinning • Overlying area of vitreous liquefaction (vitreous is abnormal) • Usually occurs from the ora to the equator • Snail track degeneration • “ White without pressure” |
|
|
What is Lattice degeneration. |

The peripheral retina becomes atrophic in a lattice pattern and may develop tears, breaks, or holes, which may further progress to retinal detachment.
• Appears as a linear track circumferentially
• Found in 6-10% of general population – develops early |
|
|
What is Lattice degeneration associated with? |
Associated RPE hyperplasia |
|
|
What would be seen with lattice degeneration? |

• Yellow glistening flecks • Sclerosed vessels • Chorioretinal atrophy may be present • Atrophic holes and flap retinal tears may be present |
|
|
Lattice degeneration |

|
|
|
How does Rhegmatogenous Retinal Detachment occur? |
• Posterior vitreous detachment (PVD) • Dynamic vitreoretinal traction occurs at abnormal adhesions • This can → vitreous haemorrhage • Traction → energy transmission to retina • To relieve traction, a break forms • RD caused by collection of subretinal fluid • Common cause of failure following RD surgery |
|

What is Proliferative Vitreoretinopathy? |
Proliferative vitreoretinopathy (PVR) is a disease that develops as a complication of rhegmatogenous retinal detachment. PVR occurs in about 8–10% of patients undergoing primary retinal detachment surgery and prevents the successful surgical repair of rhegmatogenous retinal detachment. |
|
|
What causes Proliferative Vitreoretinopathy? |
Caused by contraction of the membranes of the inner retinal surface (epiretinal membranes ERM) |
|
|
What are the clinical signs of Proliferative Vitreoretinopathy? |

Clinical sign are retinal folds |
|
|
Name the types of breaks that can occur. |
• Horseshoe or U-shaped tear • Operculated • Atrophic hole • Dialysis • Macular hole - Idiopathic; myopia; Commotio retinae |
|
|
What is a Dialysis break? |
• Involves splitting of vitreous base • Usually infero-temporal • Can be spontaneous or traumatic |
|

What is this? |
Horse shoe break |
|

What is this? |
Treatment prophylaxis with retinopexy |
|
|
What is Operculated Retinal Holes? |

• Round red hole with associated floating plug of tissue.
• The fresher the break the more likely the development of retinal detachment. |
|
|
What might surround Operculated Retinal Holes? |

Cuff of whitish oedema |
|
|
How would you manage Operculated Retinal Holes? |
• Symptomatic – same day referral • Asymptomatic - review 6 months |
|
|
What are Atrophic Retinal Holes? |

• A round retinal break without accompanying vitreo-retinal traction |
|
|
What percentage of the population is Atrophic Retinal Holes present in? |
2-3% |
|
|
How would you manage Atrophic Retinal Holes? |
• Keep in mind that retinal detachment may occur
• An isolated, asymptomatic atrophic retinal hole with no associated cuff of oedema - review in 12 months
– ENSURE that patient is educated correctly regarding symptoms of retinal detachment and comment in your notes you have done so.
• Any atrophic hole with cuff of oedema and associated symptoms should be same day referral |
|
|
What would increase the chances of getting an retinal detachment? |
• Risk factors • Increased age Age • Myopia (High) • Acute PVD • Family history of a retinal detachment or break • Previous retinal detachment or break • History of recent trauma, surgery or inflammation • Predisposing conditions • Vitreoretinal degenerations |
|
|
What symptoms may be presented with retinal detachment? |
• Photopsia • Floaters • Shadow in field of vision • 60% of patients with RD have ALL symptoms • Round asymptomatic holes may be associated with asymptomatic retinal detachments in young myopia |
|
|
When would photopsia be more noticeable? |
• More noticeable with eye movements and in dim illumination.
• Projected into temporal peripheral field most commonly. |
|
|
What should you ask if floaters are reported with retinal detachment? |
• Recent or long-standing • Last day, week,month significant? • Which eye? • What do they look like? • How many are there? • Any flashes? • Any shadows, curtains? |
|
|
What should you ask if photopsia is reported? |
• Describe the flashes? • How long do they last? • Which eye? • When do you notice them? |
|
|
How would the VAs be affected with retinal detachments? |
Normal unless macular detached or SRF approaching macula. |
|
|
How would the visual fields be affected with retinal detachments. |
• Peripheral • Maybe normal |
|
|
How would the pupil reactions be affected with retinal detachment? |
RAPD may be present |
|
|
How would the IOPs be affected with retinal detachments? |
5mmHg in affected eye |
|
|
How would you evaluate the perihipheral retina? |
• Dilated fundus examination • Superfield or SuperVitreo |
|
|
What might you see in the anterior vitreous? |
Pigment or blood in anterior vitreous |
|

What is this? |
Shafers sign |
|
|
What is shafers sign? |
Shafer's sign alludes to the clinical finding of pigment cells in the vitreous. |
|
|
How would the retina appear upon examination with a retinal detachment? |

• Slightly opaque & corrugated • Convex configuration and a slightly opaque • Loss of the underlying choroidal pattern • Retinal blood vessels appear darker than in flat • Out of focus compared to flat retina |
|
|
What symptoms would require a same day referral? |
• Sudden increase in number of floaters, patient may report as "numerous". • "too many to count" or “sudden shower or cloud of floaters”. • Cloud, curtain or veil over the vision. • Retinal detachment with good vision. • Vitreous or pre-retinal haemorrhage. • Pigment 'tobacco dust' in anterior vitreous. • Retinal tear/hole with symptoms. |
|
|
What signs would require referral ASAP next available clinic appointment? |
• Retinal detachment with poor vision (macula off). • Retinal hole/tear without symptoms. • Lattice degeneration with symptoms of recent. • flashes and/or floaters? Check for PVD first! |
|

What is this? |
Macula off detachments |
|
|
What would require discharge with SOS advice (verbal advice and a leaflet)? |
• Uncomplicated PVD without signs • Signs of lattice degeneration without symptoms listed previously |
|

What is this? |
Weiss ring |
|
|
What are the treatments for retinal detachment? |
Localisation & closure of breaks: • Relief of vitreoretinal traction • Buckling or vitrectomy • Neuroretinal-RPE adhesion Photocoagulation or cryotherapy: • Internal tamponade • Air; longer acting gases; Silicone oil |
|

What is this? |
Scleral Buckle |
|
|
What is Retinoschisis? |
Splits or cysts within the neurosensory retina |
|
|
Name the types of Retinoschisis? |
Primary • Senile (level of OPL) • Juvenile/congenital (level of RNFL) Secondary to other conditions • Trauma, proliferative retinopathies, vitreous traction |
|
|
What is Senile Retinoschisis? |

• Bilateral in 33% • Usually infero-temporal • Usually hyperopic • Dome elevation of inner • retinal layers • White dots (snowflakes) on inner limiting membrane • Inner leaf has beaten metal appearance • Sheathing of peripheral vessels |
|
|
What is Juvenile Retinoschisis? |
• X-linked recessive • Splits in NFL • Bilateral • Foveal (cystoid changes BUT not CMO) or peripheral • Associated with systemic diseases • Poor visual prognosis • Predisposes to RD, esp infero-temporally |
|
|
What would be seen with Retinoschisis? |
• Px Exam Symmetrical location no pigment cells in vitreous. • Scotoma Absolute with Retinoschisis, relative scotoma with RD. |

