![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
52 Cards in this Set
- Front
- Back
|
Cardiovascular disease CVD affects what percentage of the population? |
50% |
|
|
50% of over 65s suffer from what? |
Hypertension |
|
|
Recap- what are arteries, veins and capillaries? |

• Artery: muscular (pump, resist pressure)- 25% blood vol. (pressure reservoir)
• Capillary: highly permeable
• Vein: lower pressure, valves- 75% blood vol. (volume reservoir) |
|
|
What happens to arteries with age? |

• Vessels stiffen with age • Less elastic • ↑ damage by sheer stress • Lumen ↓ • Atherosclerosis- “fatty streak” – fibrosis (protrusion) • Same blood volume |
|
|
Blood is ejected at....? |
...high pressure |
|
|
What do arteries do with this high pressure blood flow? |
Arteries smooth pressure changes – more constant in periphery (heartbeat fluctuations) |
|
|
What happens to elastin fibres with age? |
Elasticity decreases with age, which increases pressure changes |
|
|
Where is reverse pressure wave more prominent? |

More prominent in periphery (smaller vessel and proximity) |
|
|
What affect does the ripple effect have? |

absorbed when young • summative with vessel stiffness (∴ further ↑ in BP) |
|
|
What is sphygmomanometry? |
Measuring blood pressure |
|
|
How is blood pressure measured? |

Should be performed by optometrists! • Restrict blood flow (supra-pressure) • Gradually reduce • First blood through (systolic) • Flow normalised (diastolic) |
|
|
What can affects the blood pressure reading? |
• Cuff size (too small ↑10-40mmHg) • Clothing (↑ 10-50mmHg) • Rest (seated for 5 minutes) • Posture (back supported, legs uncrossed, arm on desk) • Stress (white-coat hypertension) • Talking • Smoking, alcohol, caffeine (30 minutes before) • Temperature (cold office can increase blood pressure) • Exercise |
|
|
Blood pressure stages |

|
|
|
What is Arteriosclerosis? |
Thickening of vessel wall Hyalinisation Hypertrophy Hyperplasia |
|
|
What is Hyalinisation? |
Reduced flexibility |
|
|
What is Hypertrophy? |
Thickening= constriction |
|
|
What is Hyperplasia? |
Cell proliferation |
|
|
Why does hypertensive retinopathy develop? |

as the vascular anatomy is gradually degraded by persistent increase(s) in blood pressure |
|
|
What are the stages of hypertensive retinopathy? |
• Vasoconstrictive phase • Sclerotic phase • Exudative phase
• Malignant Hypertension |
|
|
What is the Vasoconstrictive phase of hypertensive retinopathy? |
• vasospasm and arteriole narrowing • ↓ A:V ratio (veins unchanged) • Some damaged vascular segments can’t undergo narrowing ∴ focal arteriolar narrowing (esp. older Px) |
|
|
What is the Sclerotic phase of hypertensive retinopathy? |

• Intimal thickening • Medial hyperplasia • Hyaline degeneration of vessel wall • Severe narrowing, compression of underlying veins, broad and brighter reflex. |
|
|
What is the Exudative phase of hypertensive retinopathy? |

• Retinal haemorrhages (dot, blot, flame) • Hard exudates (macular star) • Necrosis of smooth muscle and retinal ischemia (cotton wool spots) |
|
|
What is Malignant Hypertension? |

Severely raised intracranial BP causes optic nerve ischemia and oedema: • Papilloedema |
|
|
State the 4 stages of hypertensive retinopathy. |
1. Arteriosclerosis (thickening of vessel wall) 2. Arterial narrowing (general / focal) 3. Cotton-wool spots (ischemia) 4. Haemorrhages (vascular leakage) |
|

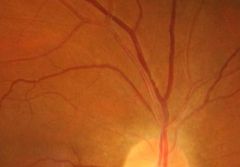
What is this? |
Arteriosclerosis |
|

What is this? |
Arterial narrowing |
|

What is this? |
Cotton-wool spots (ischemia) |
|
|
What is Grade I of the Keith-Wagner-Barker grading scale? |

Generalised arterial narrowing (+ mild increase in reflex) |
|

What is Grade II of the Keith-Wagner-Barker grading scale? |

• Obvious ↑ arterial light reflex • Salus’ sign – S-deflection of veins at A:V crossing (no tapering) |
|
|
What is Grade III of the Keith-Wagner-Barker grading scale? |

• Copper wiring • Bonnet’s sign – vein deflected away from A:V crossing • Gunn’s sign – tapering of vein either side of A:V crossing (“nipping”) |
|
|
What is Grade IV of the Keith-Wagner-Barker grading scale? |

G III and silver wiring (NOT occlusion) |
|
|
What are the issues with the KWB grading scale? |
• Subjective • Out-dated • Subtle cases • Longitudinal changes |
|

KWB grading scale |

KWB grading scale |
|
|
Scheie grading scale |

Comparison |
|
|
What is the underlying mechanism to vessel tortuosity? |
veins less muscular, less able to adjust to ↑ pressure |
|

What is this? |
Macular star |
|
|
What is macular star? |
• Seen in severe cases of hypertensive retinopathy • Hard exudates deposited around macula • Associated with macular oedema |
|
|
What is the management for hypertensive? |
• Some GPs – newly-diagnosed hypertensive scheme • Measure BP? • Advise Px • See GP • Lifestyle • Family Hx |
|
|
How would you record vessel appearance? |

• Tortuosity • Branching angles • Fractal dimension |
|
|
What is Malignant Hypertension? |

• Sudden, rapid, severe increase in blood pressure (aka accelerated hypertension) • BP: >220/120mmHg (syst./diast.) • Papilloedema • ASx (h/a?) |
|
|
How do you manage Malignant Hypertension? |
• Emergency – require specialised anti-hypertensive therapy • At risk of further damage |
|
|
What is Hypertensive Choroidopathy? |

• Rare • Acute hypertensive crisis (young adults, pre-eclampsia) • Non-perfusion (lobular – anatomy of vasculature) |
|
|
Name some haematological pathologies. |
• Sickle-cell anaemia • Leukaemia • Hyperviscosity • Valsalva manoeuvre |
|
|
What is Sickle-cell anaemia? |
• Genetic condition (African, Caribbean, Middle Eastern, Asian)
• Unusual shaped RBCs (esp. in hypoxia & acidosis)
• short life span • ↑ rigidity - prone to block blood vessels |
|
|
What are the steps of proliferative sickle cell retinopathy? |
1. Peripheral arterial occlusion
2. Peripheral AV anastomoses – pre-existing capillaries
3. Neovascularisation from anastomoses – sea-fan
4. Proliferation continues → vitreous haemorrhage
5. Fibrovascular proliferation → tractional RD |
|
|
What is Leukaemia? |
Cancer of WBC • Acute / Chronic: 1. Lymphocytes (NB – attack virus cells)
2. Myeloid cells (NB – protect cell, fight bacteria) |
|
|
What are the secondary changes with Leukaemia? |
• Haemorrhage • Infection • Occlusion • Non-retinal (iritis, CN palsies, hyphaema …) |
|
|
What is Acute leukaemia? |

• Haemorrhages, CW spots, Roth spots (haemorrhage with white centre)
• Haemorrhage →WBC adhesion to damaged endothelium → coagulate |
|
|
What is Chronic leukaemia? |

• Peripheral neovascularisation
• Choroidal deposits (leopard-print retina) |
|
|
What is Hyperviscosity? |

“Sticky blood” • Secondary to underlying pathology • Polycythaemia • Proliferation of RBCs |
|
|
What is Valsalva retinopathy? |
• ↑ intrathoracic pressure
• ↑ in BP, baroreceptors in aorta: ↓ cardiac output, ∴can feel dizzy
• ‘Pop’ ears with a cold |
|
|
What can happen with Valsalva retinopathy? |

• Spontaneous haemorrhage of capillaries: - Pre-retinal haemorrhage - Subconjunctival haemorrhage
• ASx • Vision affected depending on location of haemorrhage
• Resolve (if serious, refer) |

