![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
74 Cards in this Set
- Front
- Back
|
Name five colors of mucus membranes and what they mean?
|
Pink: Normal
Pale/White: Anemic or poor perfusion Bright red: Septic Shock Dark Blue: hypoxia Gray: poor perfusion Yellow: hepatic dysfunction Brown: methemogloinemia (acetaminophen toxicity) |
|
|
What are the levels of consciousness from awake to not awake?
|
1. Alert
2. Depressed 3. Obtunded 4. Stuperous 5. Comatose |
|
|
Define each of the following words
1. alert 2. depressed 3. Obtunded 4. Stuperous 5. Comatose |
1. normal
2. quiet, unwilling to perform normally. responds to environmental stimuli. 3. minimally responsive to auditory or tactile stimuli 4. Unresponsive to environmental stimuli. Responds to painful stimuli. 5. No response to environmental and pain stimuli. |
|
|
What is the difference between the bell and the diaphragm of the stethescope?
|
The Bell is for listening to low frequency sounds.
The diaphragm is for listening to high frequency sounds. |
|
|
How much pressure do you use with the bell and the diaphragm?
|
Bell: light pressure - too much will tighten skin and create a functional diaphragm which filters out the lower frequency sounds.
Diaphragm: firmly since it filters out the lower frequency sounds and lets you hear high frequency sounds. |
|
|
What else should you do when you listen to the heart?
|
palpate a peripheral artery in order to simultaneously feel and listen to the sounds.
|
|
|
Name different ways to get a heart rate?
|
Ascult with stethascope
Doppler Dinamap |
|
|
What are the normal heart sounds?
|
S1 (lub) and S2 (dub)
|
|
|
What is S3 or S4 heart sounds called?
|
Gallop
|
|
|
What causes S1 heart sound?
|
synchronous closure of the atrioventricular valves
|
|
|
What causes the S2 heart sounds?
|
synchronous closure of the semilunar valves and indicated ventricle relaxation.
|
|
|
What is a doppler?
What information does it give? Who are the best patients for it? |
a probe emits an ultrasonic signal that detects the movement of blood through the artery and converts it to an audible sound.
Only gives systolic pressure For small dogs and cats. |
|
|
What is an Oscillometric Method?
Whats another name for it? What information does it give? Who are the best patients for it? |
Measures oscillations caused by blood flowing through the artery with a cuff that is automatically inflated and deflated on the animals leg.
Dinamap Gives Systolic, Diastolic, MAP, Pulse Used in medium and large sized dogs. |
|
|
What are some sources of error?
|
shivering, trembling, movement, stress, inappropriate cuff size. Inconsistent measuring technique.
|
|
|
Causes of Hypotension?
|
hypovolemic shock
hypothyroidism sepsis secondary to anesthesia administration |
|
|
Causes of Hypertension?
|
chronic renal failure
hyperthyroidism cushings disease diabetes mellitus |
|
|
What does NIBP mean??????
|
Non-invasive blood pressure!
|
|
|
What is diastolic pressure? What is systolic pressure?
|
Diastolic: Pressure exerted by the blood on the vessel when the ventricles are at rest.
Systolic: Pressure exerted by the blood on the vessels when the left ventricle contracts. |
|
|
DRIP RATE:
Fido needs 1L of fluid over the next 5 hours. |
(15/60) x (1000/5) = 50 drops/min
60seconds/50 drops/min = 1.2 drops/second |
|
|
What is a Pulse-Oximetry vs Oxygen saturation?
|
Pulse-ox: non-invasive method for measuring arterial oxygen saturation.
O2 saturation - percentage of hemoglobin sites that are chemically combined with oxygen. |
|
|
Where do you place the pulse-ox probe?
|
Tongue, lip, toe web, inguinal area, ear
|
|
|
Sources of error for Pulse-Ox?
|
dark pigment, shaking/movement, vasoconstriction, hypovolemia, hypothermia, severe hypotension.
|
|
|
What are the three different types of IV catheters?
|
Over-The-Needle Catheter: Insyte, angiocath -- most commonly used
Through-The-Needle: intracath -- Placed as central lines Double/Triple Lumen Catheters: placed in critical patients when multiple fluids will need to run simultaneously. can be placed as central lines. |
|
|
IV catheter Gauge from smallest to largest and what are they used for?
|
26 - ped's and exotics
24 - ped's exotics and severe hypovolemic or vasoconstriction 22 - cats 20 - dogs 18 - fluid bolus, cases that need rapid replacement 16 - large animals (horse) |
|
|
Give the steps to placing an IV catheter?
|
1. Clip the site
2. clean site with antiseptic 3. palpate vein and have restrainer hold off 4. insert IV catheter, bevel up, at 20-30 degree angle. 5. when blood flash appears in hub stop advancing. 6. advance catheter off needle into the vein. 7.remove stylet 8.insert T-set into distal end of catheter 9. flush cath with heparinized saline 10. tape in place 11. check patency. |
|
|
What steps are involved in a fluid check?
|
1. visualize the catheter
2. check tape for wetness or blood 3. check for puffy paw (swelling) 4. check fluid rate |
|
|
What are the five things that would indicate a catheter needs to be removed?
|
redness, swelling, inflammation, bleeding at the site, excessive bruising.
|
|
|
How do you turn on a fluid pump to run?
|
1. clear volume
2. set rate of infusion at mL/hr 3. set total volume of fluid to be given 4. turn to run. |
|
|
If you need to give a 1 L bolus over 1 hour, how would you set the fluid pump?
|
Rate: 1000
VTBI: 1000mL/hr |
|
|
If you need to give a 300 mL bolus over 30 minutes, how would you set the pump?
|
Rate: 600
VTBI: 300ml because there are two 30 min in 1 hour....so you would multiply the 300 mL by 2 which is the 600 mL/hr |
|
|
If you need to give a 100 mL bolus over 20 minutes, how would you set the fluid pump?
|
Rate: 300 mL/hr
VTBI: 100 mL |
|
|
If you need to give a 200 mL bolus over 15 minutes, how would you set the fluid pump?
|
Rate: 800 mL/hour
VTBI: 200 mL |
|
|
Why do you place a urinary catheter?
|
1. collect single urine sample
2. dislodge a urethral obstruction (blocked Fe) 3. monitoring urine productions 4. maintain cleanliness of patient. |
|
|
Name the three types of urinary catheters
|
Red Rubber Catheters
Tomcat Catheter Foley Catheter |
|
|
How are Red Rubber Catheters measured? what are they used for?
|
3.5-8 French
used in dogs and cats. can be used for single collection or sutured in for in-dwelling cath. usually used for blocked cats. Soft rubber. |
|
|
What are Tomcat Catheters? Whats their normal size? When should they not be used?
|
short and fairly stiff catheters.
3.5 french should no be left in as in-dwelling because they can irritate the patient. Used to dislodge blockages in Blocked Fe. |
|
|
Foley Catheters are what? When are they used? What 2 things makes them different?
|
Most expensive catheter.
only used when in-dwelling catheter is needed. 1. inflatable bulb at the end that can be filled with liquid to keep cath in the bladder. 2. Males get the white Foley thats stiffer and gets to where it needs to be while females get the softer yellow catheter. |
|
|
What type of problems can occur with an indwelling catheter?
|
kinking of the catheter or tubing
premature removal of the catheter obstruction of the catheter with debris irritation or inflammation of the urethra. introduction of urinary tract infection. |
|
|
Fill in the blanks.
Blood comes from the upper body into the ___A___ and goes down in the ___B___. From there it passes through the ___C___ and into the ___D____. Then it goes through the ___E____ into the ____F____ which goes to the lung. Then it comes back from the lung into the heart through the ___G___ into the __H___. From there it goes through the ___I___ into the ___J____. Then it goes through the ___K___ into the __L___ and out the body. |
A.superior vena cava
B.Right atrium C. Tricuspid valve D. right ventricle E. pulmonary valve F. pulmonary artery G. pulmonary vein H. left atrium I. mitral valve J. Left Ventricle K. Aortic valve L. Aorta |
|
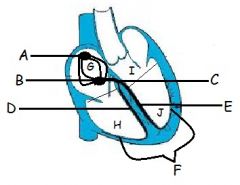
Label Each Thing
|
A. SA Node
B. AV Node C. Bundle of His D. Right Bundle Branch E. Left Bundle Branch F. Perkinge Fibers G. Right Atrium H. Right Ventricle I. Left Atrium J. Left Ventricle |
|
|
What is the sinoatrial Node?
|
main pacemaker of the heart
|
|
|
What is the Atrioventricular node?
|
alternative pacemaker of the heart. electrical impulse from SA Node to AV node causes contraction of atria.
|
|
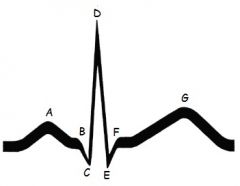
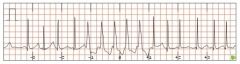
Label and Define Each part of the ECG Wave
|
A. P wave - atrial depolarization
B. PR interval - time electrical impulses takes to travel from SA node to AV node and entering ventricles. Tells us how AV node is functioning C/D/E. QRS Complex - ventricular depolarization F. ST segment - period when ventricles depolarize. G. T wave - Ventricular repolarization |
|
|
How do you Perform an ECG?
|
1. Place patient in Right lateral Recumbency
2. place patient on heavy blanket or rubber mat. 3. Clip hair if needed. Place Electrodes - 3 lead system. 4. use alcohol or ultrasound gel on the lead location. |
|
|
What color goes where for an ECG
|
White - Right front leg ( white/right)
Black - left front leg (newspaper) Red - left read (smoke over fire) |
|
|
What is the difference between the following: Sinus Arrhythmia, Sinus Bradycardia, Sinus Tachycardia
|
S. Arrhythmia - normal rate with abnormal rhythm.
S. bradycardia - normal rhythm with a decreased rate S. Tachycardia - normal rhythm with an increased rate |
|
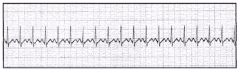
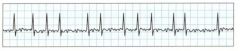
What is this?
|
Sinus Tachycardia
|
|
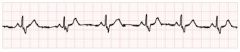
What is this?
|
Sinus Arrythmia
|
|

What is this?
|
Sinus Bradycardia
|
|
What is this?
|
Atrial Fibrillation
|
|
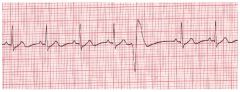
What is this?
|
Ventricular premature contraction
|
|

What is this?
|
Ventricular fibrillation
|
|
What is this?
|
Ventricular tachycardia
|
|
|
What position should an animal be in to be intubated?
|
sternal recumbency
|
|
|
What tool do you need to depress the tounge, flatter the epiglottis and use as a flashlight?
|
laryngoscope
|
|
|
What is a common intubation problem in cats that leads to serious breathing restrictions?
|
laryngospasm - reflex that prevents aspiration of foreign material and prevents oxygen from entering the lungs.
|
|
|
What is tracheitis?
|
inflammation of the trachea due to stretching of the tracheal wall due to over-inflation of the cuff.
|
|
|
What is CPRC?
|
provide artificial ventilation and circulation until advanced life support can be provided and spontaneous circulation and ventilation can be restored.
|
|
|
What is cardio pulmoary arrest?
|
cessation of an effective cardiac output and respiration
|
|
|
What happens when an animal arrests?
|
loss of consciousness
absence of ventilation or agonal breathing cyanosis absence of palpable pulses absence of heart sounds dilation of pupils |
|
|
What are the ABC's and DEF of CPR? :D
|
Airway
Breathing Circulation Drugs Ecg Fibrilation |
|
|
What needs to be done for Airway?
|
check the oral cavity. clear any foreign material, intubate.
|
|
|
What needs to be done for Breathing?
|
administer breaths via ambu bag and oxygen. 1 breath every 3 seconds. correct breaths will achieve normal chest wall movement.
|
|
|
What needs to be done for Circulation?
|
Begin external cardiac compressions with the animal in RLR. Done over the heart in the area of the 6th rib. rate of 120-150/min. maintain contact with body during this.
|
|
|
What needs to be done during the drug phase? and what drugs used?
|
Need IV access. If IV access is not possible initially, drugs can be given via the endotracheal tube. Give IV fluids given to maintain an effective circulating volume.
Epinephrine and Atropine should be given |
|
|
What will happen with a successful arrest?
|
spontaneous circulation
spontaneous respiration return of central nervous system function. |
|
|
Post CPCR care
|
closely monitored
frequent subsequent arrests can occur underlying cause of the arrest must be identified and treated cerebral hypoxia and edema commonly occur after five minutes of an arrest. monitor all body functions. |
|
|
Why do you place a bandage?
|
Fracture Stabilization - distal limbs one joint above and below to properly stabilize.
Wound healing - protect from contamination, protect from additional trauma, immobilize the wound, promote wound healing. |
|
|
Name the types of bandages and what they are used for?
|
Robert Jones - temp. immobilization of fractures distal to elbow or stifle before surgery.
Modified Robert Jones - less bulky - reduce postoperative swelling of limbs. Chest or Abdomen - compression no more than 4 hours Distal limb splints - temp immonilization of stabilization of fractures Ehmer sling - immonbilize a limb after reduction of craniodorsal coxofemoral luxation. Prevent weight-bearing. Tail wrap - protects amputation or trauma to tip. Ear bandage - used after aural hematomas, after ear surgery, or after traumatic injury to the pinna. |
|
|
What are the three layers of a bandage?
|
Primary or contact layer - non-adherent
Secondary - absorbent, padded Tertiary layer - the holding, protective layer. Always leave a toe out to check color, warmth, and for swelling. |
|
|
How do you provide after care for a bandage?
|
check toes, warm and pink
keep clean and dry place e-collar if needed. check for "strike through" |
|
|
List two abnormal lung sounds
|
fluid in lungs, crackles, rhales, ronchi
|
|
What do you say to this?
|
HAHAHA
|
|
What do you say to this?
|
HAHA
|

