![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
64 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
General Thoughts......
|
What rank # is Cerebral vascular disease in the US?
CVD – 3rd in cause of death in U.S. AND leading cause of serious disability |
|
|
|
What is the definition of cerebral vascular disease?
|
Definition: any abnormality of the brain caused by disease of blood vessels (thrombosis, embolism, hemorrhage)
|
|
|
|
What are the major categories of CVD?
|
Major categories:
Hypoxia, ischemia, infarction Intracranial hemorrhage Hypertensive CV disease |
|
|
|
What does a stroke mean?
|
Stroke (brain attack): Clinical term applies to all three:
Hypoxia, ischemia, infarction Intracranial hemorrhage Hypertensive CV disease |
|
|
|
How much does the brain weigh?
How much of the Cardiac output does the brain get? |
1-2% of body weight; receives
15% of resting cardiac output; |
|
|
|
What is the total body oxygen consumption of the brain?
What is the nl cerebral blood flow? |
20% of total body oxygen consumption;
cerebral blood flow = 50 ml/min/100 gm tissue |
|
|
|
What are risk factors for CVD?
|
CVD risk factors include hypertension, hypercholesterolemia, diabetes, heavy alcohol consumption, oral contraceptive use and, of course, smoking
|
|
|
|
What are the different signs of Hypoxia?
|
Reduced oxygen content
Reduced perfusion Watershed / border zone areas |
|
|
|
What are the different signs of Ischemia?
|
Results from any insult which significantly reduces CNS perfusion - - - hypotension, vessel obstruction
May be transient of permanent May be focal and global Clinical outcome varies – TIA: reversible, duration less than 24 hours; results from platelet thrombi or atheroemboli Gross - - edema |
|
|
|
What are the signs of Ischemia?
|
Results from long term ischemia
Causes 85% of strokes Secondary to thrombosis, embolism, small vessel disease |
|
|
|
Ill give you symptoms of CVD and you need to tell me what the disease is?
|
Let's begin
All hypoxia, ischemia, and infarction causes dementia |
|
|
|
Weakness, sensory loss contralateral leg
Transient expressive aphasia Abulia – inability to make decisions |
Anterior cerebral artery
|
|
|
|
Contralateral hemiplegia (arm, face)
Contralateral sensory loss Aphasia (if dominant hemisphere) |
Middle Cerebral Artery
|
|
|
|
Contralateral hemianopia or total cortical blindness if bilateral alexia
Thalmic syndrome (contralateral anesthesia – some develop pain) |
Posterior Cerebral Artery
|
|
|
|
You need to know the changes that occur at different times for gross and micro due to hypoxic, ischemic, infarction events......all associated with cerebral infarction
|
begin
|
|
|
|
Time 0-12
|
Gross: no change
Micro: minimal or NO changes |
|
|
|
Time 12-24 hrs
|
Gross: minimal
Micro: red (hyperesosinophilic) neurons with pykotic nuclei |
|
|
|
Time 24-48 hrs
|
Gross: Indistinct gray-white matter junction
Micro: Neutrophilic infiltration |
|
|
|
Time 2-10 days
|
Gross: Friable tissue with marked edema
Micro: Histiocytic infiltration; neurons disappear |
|
|
|
Time: 2-3 weeks
|
Gross: Tissue liquefies
Micro: Liquefactive necrosis; histiocytes filled with products of myelin breakdown |
|
|
|
Time: 3wks-1month
|
Gross: Fluid-filled cavity demarcated by gliotic scar
Micro: Fluid-filled cavity; reactive astrocytes and lipid-laden macrophages (glitter cells) |
|
|
|
Time: Years
|
Gross:Old cyst surrounded by gliotic scar
Micro: Astrogliosis surrounding a cyst |
|
|
|
New topic
Intracranial Hemorrhage |
General Thoughts
|
|
|
|
What are the 3 types of intracranial hemorrhage
|
Three types:
1. Intracerebral; 2. Subarachnoid/Ruptured Saccular; 3. Vascular Malformation |
|
|
|
Where can intracranial bleeds occur?
|
May occur anywhere in CNS – there are high risk areas
|
|
|
|
What are primary intracranial hemorrhages?
|
Primary within epidural & subdural space are usually traumatic
|
|
|
|
What are secondary intracranial hemorrhages to?
|
Subarachnoid and parenchymal are secondary to CVD
|
|
|
|
What % of strokes is from intracranial hemorrhage?
|
Cause 15% of strokes
|
|
|
|
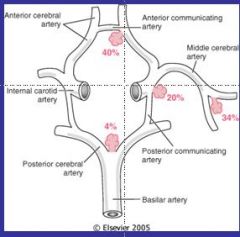
Where does most intracranial hemorrhage occur....what artery?
|
Anterior communicating artery
|
|
|
|
Intracranial Hemorrhage
Picture |
|
|
|
|
At what age does intracerebral hemorrhage peak?
|
Peak incidence about age 60
|
|
|
|
What is the most common underlying cause of intracerebral hemorrhage?
EXAM***** |
Hypertension
Hypertension is the most common underlying cause (>50%) |
|
|
|
What are the clinical signs of intracranial hemorrhage?
|
Clinical – varies by location and size; may be silent or evolve
|
|
|
|
What are the gross appearances of intracranial hemorrhage?
|
50-60 % originate in putamen
Show extravasation of blood with compression of adjacent parenchyma - - edema |
|
|
|
What are the micro appearances of intracranial hemorrhage?
|
Central area of clotted blood
Surrounding brain tissue shows anoxic neurons Edema, etc. (on chart) |
|
|
|
What is a Subarachnoid hemorrhage?
|
Most common cause is rupture of saccular (berry) aneurysm
May result from trauma, hypertension, vascular malformation, hematologic problems, tumors Saccular aneurysm is most common type of intracranial aneurysm (Others – atherosclerotic, mycotic, traumatic, dissecting |
|
|
|
What is the most common cause of a Subarachnoid hemorrhage?
|
Most common cause is rupture of saccular (berry) aneurysm
|
|
|
|
What is the most common type of subarachnoid hemorrhage?
|
Saccular aneurysm is most common type of intracranial aneurysm (Others – atherosclerotic, mycotic, traumatic, dissecting)
|
|
|
|
What are some diseases that may increase your risk of subarachnoid hemorrhage?
|
Increased risk with autosomal dominant polycystic kidney disease, Ehlers-Danlos syndrome, neurofibromatosis type I, Marfan syndrome, fibromuscular dysplasia of extracranial arteries, coarctation of aorta
|
|
|
|
What are some more factors that increase chances of subarachnoid hemorrhage?
|
Of course cigarette smoking & hypertension are factors
|
|
|
|
Are subarachnoid hemorrhages congenital?
|
Not really congenital, but develop over time because of risk factors
|
|
|
|
Are subarachnoid hemorrhages seen more in men or women?
|
Rupture seen in 40’s; slightly more often in ladies
|
|
|
|
What size do you see bleeding for subarachnoid hemorrhages?
|
10 mm or greater have 50% risk of bleeding and this is increased with increase in intracranial pressure
|
|
|
|
What Type of intracranial hemorrhage presents as, "worst headache of my life?"
EXMA***** |
Subarachnoid Hemorrhage
Presents typically as “the worst headache I’ve ever had” |
|
|
|
What % of people die from first rupture of subarachnoid hemorrhage?
|
25-50% die with first rupture; rebleeding is common
|
|
|
|
What are gross findings of subarachnoid hemorrhage?
|
Gross:
Usual saccular pattern in circle of Willis Rupture causes extravasation of blood into subarachnoid space & substance of brain |
|
|
|
What are micro findings of subarachnoid hemorrhages?
|
Micro:
Usual aneurysm / vessel morphology No muscular wall and intima in aneurysm sac only hyalinized intima |
|
|
|
Next topic
|
Vascular malformations
|
|
|
|
Vascular Malformations
Classified into four groups: Arteriovenous Cavernous Capillary Venous angiomas |
What is most common clinically significant vascular malformation?
A / V most common clinically significant; men : women = 2 X |
|
|
|
At what age do most vascular malformations present?
|
Present early – age 10 – 30 years
|
|
|
|
How do most vascular malformations present?
|
Often present with seizure disorder, intracerebral or subarachnoid hemorrhage
|
|
|
|
What is the site of most vascular malformations?
|
Most common site is middle cerebral artery (posterior branches)
|
|
|
|
What are the gross and micro findings of vascular malformations?
|
Gross & Micro show tangled network of vascular channels
|
|
|
|
Next topic......
|
Hypertensive CVD
|
|
|
|
General Thoughts.....
|
The most important sequelae of hypertension on the brain:
Massive intracerebral hemorrhage Lacunar infarcts Slit hemorrhages Hypertensive encephalopathy |
|
|
|
What 2 things are frequently seen with hypertensive CVD?
|
Atherosclerosis & diabetes are frequent compadres
|
|
|
|
What are Lacunar Infarcts
|
Result from occlusion of deep penetrating arteries which supply basal ganglia, hemispheric white matter, brainstem
|
|
|
|
What are specific areas where lacunar infarcts are found?
|
Specific areas are: lenticular nucleus, thalamus, internal capsule, deep white matter, caudate nucleus, ponds (in decreasing frequency)
|
|
|
|
What are the gross and micro findings of lacunar infarcts?
|
Gross & micro
Cavitary lesions (lacunes - - - lake–like) 15 mm wide Fat-laden macrophages with surrounding gliosis |
|
|
|
Lacunar infarcts wiki style
|
Lacunar infarcts are small (0.2 to 15 mm in diameter) noncortical infarcts caused by occlusion of a single penetrating branch of a large cerebral artery [1]. These branches arise at acute angles from the large arteries of the circle of Willis, stem of the middle cerebral artery (MCA), or the basilar artery. Although this definition implies that pathological confirmation is necessary, diagnosis in vivo may be made in the setting of appropriate clinical syndromes and radiological tests.
|
|
|
|
What are slit hemorrhages?
|
Result from small vessel rupture and hemorrhage
Healing leaves a slit-like cavity Micro shows cavity with surrounding pigment-laden macrophages |
|
|
|
What is Hypertensive encephalopathy?
|
Clinical:
Hypertensive patient who has diffuse cerebral dysfunction including: Headaches Confusion Vomiting convulsion Sometimes coma Related to increased intracranial pressure Without rapid therapeutic intervention may see patient in the necropsy suite |
|
|
|
What will you see gross and micro for Hypertensive Encephalopathy?
|
Gross & Micro
Generalized edema May have transtentorial and / or tonsillar herniation Scattered petechiae in gray and white matter Evidence of remote hemorrhage and foci of necrosis |
|
|
|
What can develop from hypertensive encephalopathy?
|
Long term with multiple episodes patients develop vascular dementia (multi-infarct).
|
|

