![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
|
What family of steroids do topical corticosteroids belong to?
|
Glucocorticoid family
|
|
|
What is the mechanism of action of topical corticosteroids?
|
1. Steroid hormone binds receptor in cytoplasm
2. Translocation of steroid-receptor complex to nucleus 3. Binding of complex to DNA regulatory site 4. Transcription 5. Translation --> anti-inflammatory gene expression increased, also can prevent transcription of pro-inflammatory genes |
|
|
What are the side effects of topical corticosteroids?
|
- Mainly restricted to area of application
- Hypopigmentation, hypertrichosis, skin atrophy, and telangiectasia (reversible) - Stria (irreversible) - Acne or perioral dermatitis (form of rosacea) - Chronic use may increase risk of glaucoma and cataract |
|
|
How many classes of topical corticosteroids are there? Which are strongest/weakest?
|
- Classes: I - VII
- Class I is the most potent, class VII is the weakest |
|
|
What are the "vehicles" of topical corticosteroids?
|
- Ointment
- Cream - Lotion and solution - Foam - Gel |
|
|
What are the pros and cons of ointment administration of topical corticosteroids?
|
- Pros: occlusive barrier, better penetration, moisturizing
- Cons: greasy, patient non-compliance (texture of petroleum jelly) |
|
|
What are the pros and cons of cream administration of topical corticosteroids?
|
- Pros: better patient compliance
- Cons: less potent for some steroids, can sting on open skin |
|
|
What are the pros and cons of lotion and solution administration of topical corticosteroids?
|
- Pros: good for scalp and hair-bearing areas
- Cons: stinging (same as foam) |
|
|
What are the pros and cons of foam administration of topical corticosteroids?
|
- Pros: good for scalp and hair-bearing areas
- Cons: stinging (same as lotions and solutions) |
|
|
What are the pros and cons of gel administration of topical corticosteroids?
|
- Pros: good for intraoral use
- Cons: drying, stinging |
|
|
What measurement system is used to administer topical corticosteroids?
|
"Fingertip unit" - stripe of medication from fingertip to DIP joint (0.5 g) - cover an area equivalent to an adult palm for 2 applications
|
|
|
How do you estimate the amount of topical corticosteroid to prescribe?
|
Use palm to estimate surface area involved and multiply by 15 g to get amount necessary for 1 month
|
|
|
What are the inflammatory skin conditions?
|
- Psoriasis
- Atopic Dermatitis - Seborrheic Dermatitis - Lichen Planus |
|
|
What is the cause / trigger of Psoriasis?
|
- Immune-mediated, polygenic
- Trauma, infections, medications, etc may trigger disease in predisposed individuals |
|
|
What are the characteristic lesions in Psoriasis?
|
- Well-demarcated erythematous papules and plaques
- Pinpoint to <20 cm in diameter - Overlaying micaceous or silvery scale |
|
|
What are the clinical variants in Psoriasis?
|
- Plaque psoriasis (most common, on extensor extremities)
- Inverse (flexural, axillae, groin, perineum, chest) - Guttate psoriasis (numerous smaller lesions, often triggered by strep infection) - Erythrodermic psoriasis (generalized erythema) - Pustular psoriasis (broad patches of erythema and overlying pustules) |
|
|
What are the characteristics of Plaque Psoriasis?
|

- Most common
- Symmetric - Involves extensor elbows and knees most commonly - Pink patches and plaques w/ overlying silvery scales |
|
|
What are the characteristics of Inverse Psoriasis?
|

- Flexural locations
- Axillae, groin, perineum, chest |
|
|
What are the characteristics of Guttate Psoriasis?
|

- Drop-like
- 2-10 mm (numerous and smaller) - Symmetric trunk / proximal extremities - Often triggered by Group A strep |
|
|
What are the characteristics of Pustular Psoriasis?
|

- Pustules present on top of broad plaques of erythema
- May be localized to palms/soles or generalized - Often cyclic - Unexplained triggers |
|
|
What are the characteristics of Erythrodermic Psoriasis?
|

- Generalized erythema
- Amount of scaling is variable - Most severe |
|
|
How are nails affected by Psoriasis?
|
- Pitting (pinpoint indentations)
- Thickening - Yellow discoloration |
|
|
What non-cutaneous changes occur in Psoriasis?
|
- Psoriatic arthritis (20-30%)
- Increased risk of metabolic syndrome - Atherosclerotic CV disease |
|
|
What past medical history questions should be asked when suspecting Psoriasis?
|
- Recent infections? --> trigger (Strep)
- Risk factors for HIV? --> worse dz - Joint symptoms? --> arthritis common - BMI? --> correlation between BMI and severity - CV risk factors? --> increased risk - Family hx (genetic predisposition, 1/3 have positive family hx) |
|
|
What medications can trigger or exacerbate Psoriasis?
|
- Systemic corticosteroid withdrawal (especially pustular variant)
- Beta blockers - Lithium - Antimalarials - Interferons |
|
|
What extracutaneous site may be affected DIRECTLY by psoriasis?
|

Joints (20-30% affected by arthritis)
- Asymmetric oligoarthritis most common (knee, DIPs) - Flexural deformities - Pencil in cup deformity at MTP or MCP joints (tapering of bones) |
|
|
Which other ectodermal structures are most commonly affected by Psoriasis?
|

Nails (25-50%)
|
|
|
What is the Koebner phenomenon?
|
Development of skin lesions at sites of injury (psoriasis)
|
|
|
What is the Auspitz sign?
|
Pinpoint bleeding points seen when scale removed (psoriasis)
|
|
|
How should Psoriasis be treated?
|
Depends on extent of disease:
- Localized / mild - topicals corticosteroids only (also retinoids, coal tar derivatives, calcineurin inhibitors (tacrolimus and pimecrolimus), topical vitamin D analogs) - Generalized - combo therapy (systemic / phototherapy + topicals) - Systemics: methotrexate, cyclosporine, acitretin, and biologics (target T cells and cytokines) - TNF-alpha inhibitors: etancercept, inflixamb, adalimumab - IL-12 and IL-12 inhibitors: ustekinumab * AVOID Oral corticosteroids because withdrawal will cause psoriasis flare (often pustular) |
|
|
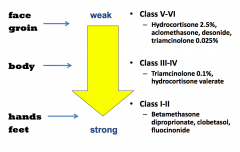
What topical corticosteroids are appropriate for face and groin?
|
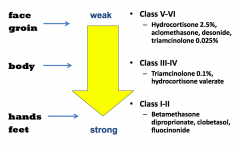
Weaker, class V - VI:
- Hydrocortisone 2.5% - Aclomethasone - Desonide - Triagmcinolone 0.025% |
|
|
What topical corticosteroids are appropriate for body?
|
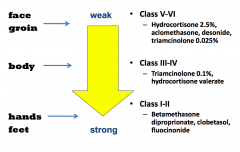
Class III - IV
- Triamcinolone 0.1% - Hydrocortisone valerate |
|
|
What topical corticosteroids are appropriate for hands and feet?
|
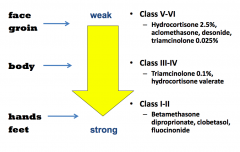
Strong, Class I - II
- Betamethasone - Diproprionate - Clobetasol - Fluocinonide |
|
|
What medications can be used for plaque type psoriasis? What are their side effects?
|
- Topical steroids - skin atrophy, hypopigmentation, striae
- Tazarotene (topical retinoid) best w/ topical corticosteroids - skin irritation, photosensitivity - Salicylic or Lactic Acid (keratolytic agents) that reduce scaling and soften plaques - systemic absorption can occur, decreases efficacy of UVB phototherapy - Coal Tar - skin irritation, odor, staining of clothes |
|
|
What medications can be used for in combination with topical steroids for added benefit? Side effects?
|
- Calcipotriene (vit. D derivative) - skin irritation, photosensitivity, no contraindication w/ UVB therapy
- Salicylic or Lactic Acid (reduces scaling and soften plaques - decreases efficacy of UVB therapy, systemic absorption can occur - Tazarotene (topical retinoid) - skin irritation, photosensitivity |
|
|
What are Calcineurin inhibitors used for?
|
- Tacrolimus and Pimecrolimus
- Off label use for facial and intertriginous psoriasis - Can cause skin burning and itching |
|
|
What kind of phototherapy is used for psoriasis?
|
- Narrowband UVB
- PUVA (psoralen + UVA) |
|

Patient has 4-week history of this facial eruption. Treated w/ 10 day course of cephalexin w/ no response. He occasionally scratches it but otherwise not bothered.
What is the diagnosis? |

Atopic Dermatitis
|
|
|
What is the most common chronic inflammatory skin disease?
|
Atopic Dermatitis (AD)
|
|
|
When is the onset of Atopic Dermatitis?
|

- Onset in infancy
- Delayed onset in adulthood may be seen - Often w/ other disorders like allergic rhinoconjunctivitis and asthma |
|

What is a major predisposing factor to Atopic Dermatitis?
|
Mutations in profillagrin gene (responsible for Ichthyosis Vulgaris - severe dry skin)
|
|
|
What can commonly complicate Atopic Dermatitis?
|
- Secondary infection w/ S. aureus - can aggravate AD by stimulating inflammatory cascade
- Rapid dissemination of Herpes Simplex Virus w/ areas of excema = Excema Herpeticum |
|
|
What are the characteristics of Atopic Dermatitis in infants?
|

– Facial involvement predominates early – Tends to spare midface
– Oozing, crusting common – Exacerbated by saliva, foods – Extensor involvement late infancy – Sparing of diaper area |
|
|
What are the characteristics of Atopic Dermatitis in childhood (>2yo to puberty)?
|

– Distribution: flexural involvement, antecubital and popliteal fossae, wrists, ankles, neck, hands
– Less crusting |
|
|
What secondary change is specific to a chronic eczematous lesion?
|

Lichenification (exaggerated skin lines)
|
|
|
What physical exam finding may be seen in patients with Atopic Dermatitis?
|

Dennie-Morgan Folds
|
|
|
What are some potential complications of atopic dermatitis?
|
- Infection
- Poor sleep (d/t itching) - Failure to thrive |
|
|
How should you treat Atopic Dermatitis?
|
- Topical corticosteroids - OINTMENTS, may add wet wrap to increase penetration (creams can sting)
- Immunomodulators (calcineurin inhibitors, tacrolimus, pimecrolimus) - Anti-histamines (alleviate pruritus) - Bleach baths to treat/prevent secondary infections - Phototherapy (narrowband UVB) - AVOD systemic steroids (rapid rebound) - Systemic: Cyclosporine, methotrexate, mycophenolate mofetil, azathiprine |
|
|
What factors influence what topical corticosteroid to use for Atopic Dermatitis?
|
- Duration of lesion: new will respond to weaker agents, chronic will need stronger agents
- Location of lesion: thin skin use lower strength d/t side effects, thicker skin use stronger strength to insure penetration/absorption |
|
|
What allergies are associated with Atopic Dermatitis?
|
EGG allergy (greatest link to AD exacerbations)
|
|
|
What mediates acute and chronic atopic dermatitis?
|
- Acute: Th2 response (IL-4, -5, -10)
- Chronic: Th1 response (IFN-y, IL-12) |

