![]()
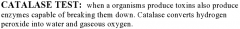
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
64 Cards in this Set
- Front
- Back
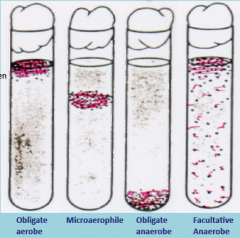
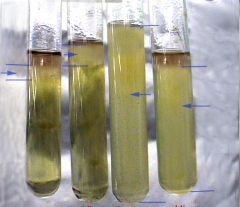
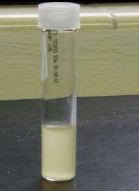
Does not require oxygen. Can grow with or without it. Able to detoxify toxic by products of oxygen.
Growth THROUGHOUT the test tube. Due to ability to grow with or without oxygen. |
Oxygen relation: Facultative Anaerobe
Example: E. Coli |
|

Does not grow in atmospheric oxygen, but requires a small amount for growth. Able to detoxify toxic by products of oxygen.
Growth in the MIDDLE of tube. Due to not being able to grow in high oxygen, or no oxygen. |
Oxygen relation: Microaerophile
Example: Micrococcus luteus |
|

Lacks the enzyme for using oxygen. Can’t live in oxygen. NOT able to detoxify toxic by products of oxygen.
Growth at BOTTOM of tube. Due to not being able to grow in oxygen. |
Oxygen relation: Anaerobe
Example: Clostridium |
|
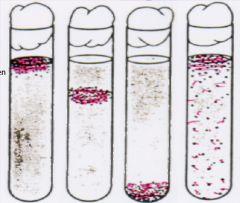
These test tubes have an oxygen gradient. The highest oxygen level at the top of the tube, and little to no oxygen at the bottom.
|
|
|

A gas pak is used to create anaerobic conditions in the jar.
By comparing bacterial growth on plates grown in the jar and outside the jar in aerobic conditions, you can determine aerobic, anaerobic and microaerophilic bacteria. |
Anaerobic Jar
A methylene blue indicator is used to show the oxygen content. Blue = oxygen, white = NO oxygen. |
|
|
are substances that reduce the number of pathogens on inanimate objects
|
Disinfectants
|
|
|
Substances that reduce the number of pathogens on living surfaces
|
Antiseptics
|
|
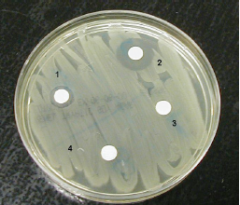
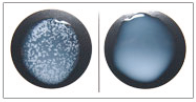
Sensitive:
Resistant: |
Sensitive
doesn't like the disinfectant and there will be a zone around the disk Resistant disinfectant has no effect on the bacteria and they will grow right up to the disk |
|
|
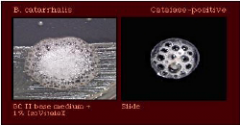
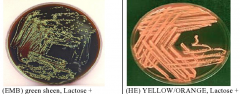
E. Coli is distinguished from Enterobactor on the EMB agar
|
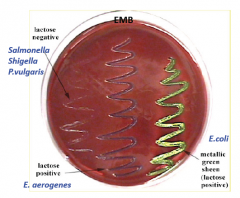
By having a green sheen. GRAM + will not grow due to bile salts and some dyes on these plates.
|
|
|

|
|
|
E.F.
|
|

|
M.M.
|
|

|
C.O. (obligate anaerobe)
|
|
|

|
|
|

|
|
|
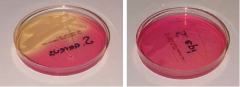
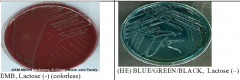
Staphylococcus Aureus
Staphylococcus / Epidermidis |
|

|
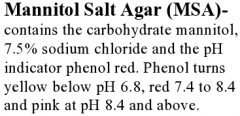
Staphylococcus Aureus (beta - hemolysis)
Staphylococcus Epidermidis (gamma - hemolysis) Streptococcus Pyogenes (beta - hemolysis) |
|
|
|
|
|
|
|

|
|
|
|
|
|

|
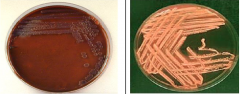
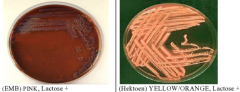
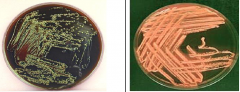
EMB Agar Plate
|
|

|
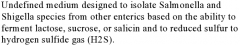
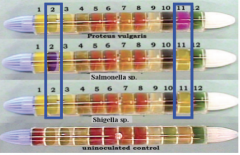
Hektoen Agar Plate
|
|
|
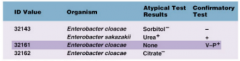
Enterobacter
|
|
|
E. Coli
|
|
|
Salmonella
Non Fermanter |
|
|
Shigella
|
|
|
Proteus
|
|

Name:
EMB: Blood Agar: SAB: |

Name: E. coli
EMB: Green Blood Agar: Alpha Hemolysis SAB: Pinpoint Colonies |
|

Name:
EMB: Blood Agar: SAB: |

Name: Enterobacter
EMB: Pink Blood Agar: Alpha hemolysis partial breakdown of RBC's also known as translucent SAB: Pinpoint Colonies |
|
|
Name: Strep Pyogenes
EMB: Blood Agar: SAB: |
Name: Strep Pyogenes
EMB: No Growth Blood Agar: Beta Hemolysis - complete breakdown of RBC's also known as transparent SAB: No Growth |
|
|
Name: Staph Aureus
EMB: Blood Agar: SAB: |

Name: Staph Aureus
EMB: Growth Blood Agar: Beta hemolysis - complete breakdown of RBC's also known as transparent SAB: Pinpoint Colonies |
|
|
Name: Staph Epidermidis / candida albicans mix culture
EMB: Blood Agar: SAB: |

Name: Staph Epidermidis / candida albicans mix culture
EMB: No Growth Blood Agar: Gamma - none hemolysis SAB: pinpoint colonies |
|
|
Name: Staphylococcus epidermidis
EMB: Blood Agar: SAB: |
Name: Staphylococcus epidermidis
EMB: N/A Blood Agar: Gamma - none hemolysis SAB: No Growth |
|
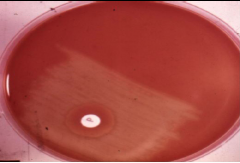
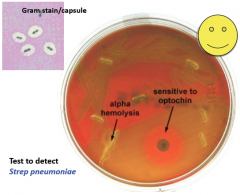
Name: Streptococcus pneumonia
|
Alpha hemolysis - partial breakdown on RBC's also known as translucent
this known as the sensitive to OPTOCHIN (P-disk) |
|
|
Staph Aureus
|
Grown on Manmtol salt agar. In a blood agar is a Beta hemolysis - complete breakdown RBC's also known as transparent
|
|

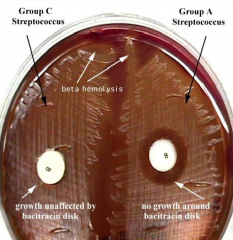
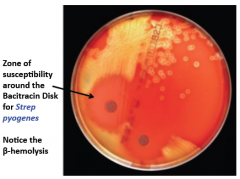
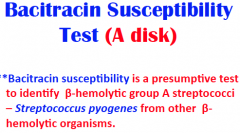
Streptococcus Pyogenes
|
Beta hemolysis - complete breakdown of RBC's also known as transparent. This is known as the Senstitive to BACITRACIN (A-disk)
|
|
|
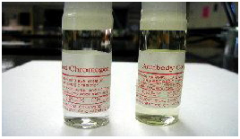
ELISA
|
Enzyme Linked Immunoabsorbent Assay
HIV Test |
|
|

|
|
|
|
|
|

|
|
|
|
|
|
How does the Elisa test works?
|

|
|
|
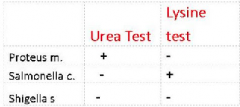
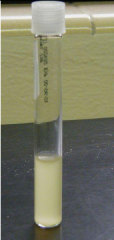
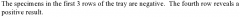
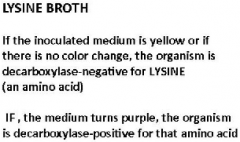
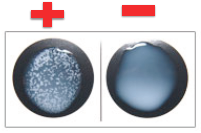
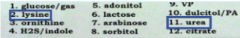
Urea Broth
- the presence of urease is detected when the organisms are grown in a urea broth medium containing the pH indicator phenol red -If ammonia is produced a highly alkaline environment will result in phenol red turning a deep pink -A positive test for Urease = Deep Pink Color -A negative test for Urease is the failure to produce this color. No change from the original. (Peach Color) |
|
|
|
|
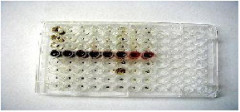
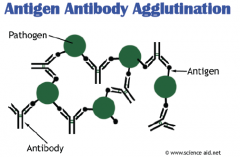
This is a direct antigen agglutination test for the identification of
|
Staph aureus.
when atibodies encounter an antigen they will form a clump called an agglutinate |
|
|
If the patient has gastrointestinal symptoms, what agar would you use to isolate a potential pathogen?
|
EMB, HE
|
|
|
If the patient feels a burning feeling in their urethra, what agars would you use to isolate a potential pathogen?
|
EMB, SAB, Blood Agar
|
|
|
If the patient has a very painful sore throat, what agar would you use to isolate a potential pathogen? Would you include an antibiotic disc? Which one?
|
Blood agar, A disc
|
|
|
If the patient has symptoms of pneumonia, what agar would you use to isolate a potential pathogen? Would you include an antibiotic disc? Which one?
|
Pneumoniae, P disc
|
|
|
Diseases Caused by Staphylococcus a.
|
Impetigo, cellulitis, abscess, boils, furuncle, food poisoning, Toxic Shock Syndrome, septicemia
Skin infection, Food Poisoning |
|
|
Diseases caused by Streptococcus species
|
Sepsis, scarlet fever, Rheumatic Fever, Necrotizing Fasciitis, Toxic Shock Syndrome, septicemia, nephritis
|
|
|
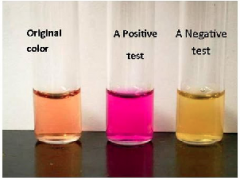
You will use EMB and Hektoen to help you identify each species
|
Gram negative organisms you will be identifying:
• E. coli • Enterobacter aerogenes • Proteus vulgaris • Salmonella spp. • Shigella spp. |
|
|
|
|

|
|
|

|
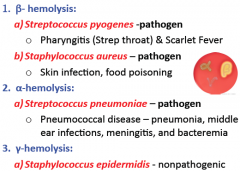
Blood agar hemolysis: allows differentiation of bacteria based on their ability to hemolyze red blood cells
Beta: Clearing medium total destruction Alpha: Greenish discoloration, partial destruction Gamma: non hemolytic |
|
|
|
|
|
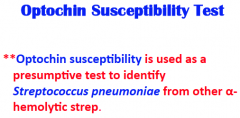
P-test
|
|
|
Rapid Testing
|
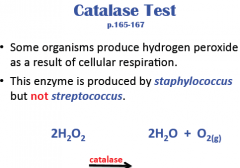
1. Differentiates Staph from Strep
2. Differentiates St.aureus from St.epidermidis 3. Identifies St.aureus |
|

|
|
|

|
|
|
|
|
|

|
|
|

|
|

