![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
23 Cards in this Set
- Front
- Back
|
Describe the anatomical components of the mitral valve.
What two regions does the mitral valve separate? |
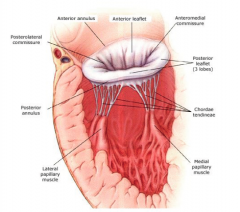
- Annulus
- Two leaflets (Anterior and Posterior) - Chordae (attach the leaflets to the papillary muscles) - Papillary Muscles Separates the left atrium from the left ventricle. |
|
|
The mitral valve is separated from which valve my a curtain?
Which leaflet (anterior or posterior) is larger in the mitral valve? |
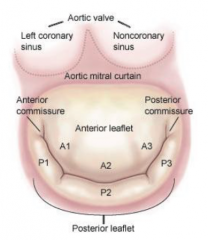
Aortic valve
The anterior leaflet. |
|
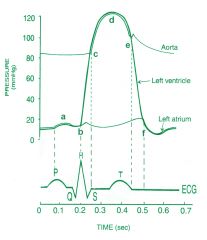
At which letter on the Wigger's diagram does the mitral valve open?
At which letter does it close? |
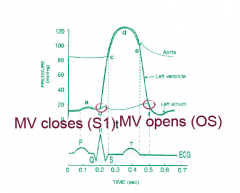
Opens - f
Closes - b |
|
|
What is the most common cause of mitral stenosis?
2 other causes? One the was specified the other I like |
Rheumatic fever.
tumors of the left atrium - myxoma and endocarditis with large vegetation |
|
|
What is rheumatic fever?
What are common symptoms and what is the treatment? |
Inflammatory condition leading to a complicated URTI due to Group A Strep.
Sx - chills, fever, fatigue, migratory arthralgias, other sx as per Jones Criteria Tx - Anti-inflammatory and penicillin |
|
|
Describe the Jones criteria (major and minor) for rheumatic fever.
|
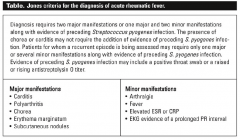
Major
1) Carditis 2) Polyarthritis 3) Chorea 4) Erythema marginatum 5) Subcutaneous nodules Minor 1) Arthralgia 2) Fever 3) Elevated ESR or CRP 4) EKG eveidence of prolonged PR interval Diagnosis requires 2 major criteria, or 1 major and 2 minor with preceding evidence of strep infection. |
|
|
Describe the pathology (cause) of mitral stenosis.
|
Inflammation produces fibrous thickening and calcification, the commisures fuse, there is chordal thickening and shortening, leading to poor valve compliance.
|
|
|
Describe the pathophysiology (systemic consequences) of mitral stenosis.
|
The poorly functioning valve leads to a pressure build-up in LA, which may lead to pulmonary hypertension and RHF.
|
|
|
What is the normal size of the mitral valve (cm^2) and when is stenosis considered significant?
|
Normal: 4-6 cm^2
Hemodynamically significant stenosis: < 2 cm^2 |
|
|
What are some symptoms of severe mitral stenosis?
|
SOBOE and reduced exercise capcity
Pulmonary congestion at rest, leading to orthopnea and PND Pulmonary hypertension leading to RHF Hoarseness due to LA enlargement, compressing the recurrent laryngeal nerve. |
|
|
What are some complications of MS?
|
endocarditis
Afib hemoptysis thrombus formation |
|
|
What is found with auscultation in mitral stenosis?
|
Loud S1 (in early disease, soft S1 in late disease), opening snap following S2 (stiff valve).
Murmur is low pitched, diastolic rumble with pre-systolic accentuation. |
|
|
What investigations would you order to evaluate mitral stenosis?
|
ECG - LA enlargement, +/- RVH, atrial fibrillation
CXR - LA enlargement, pulmonary vascular redistribution, edema, Kerley B lines Echocardiography – visual assessment of valve, velocity of blood across the valve allows us to estimate the pressure gradient and MVA (mitral valve area) |
|
|
What are the pharmacological and surgical interventions for treatment of mitral stenosis and what are the indications?
|
Pharmacological:
Diuretics (for pulmonary hypertension) Beta-blockers or CCB (decrease HR) Anticoagulants (only if in atrial fibrillation) Surgery: Percutaneous valvuloplasty Mitral Valve replacement (in patients where valvuloplasty is not suitable i.e. LA clot, severe calcification, MR) |
|
|
What is the most common cause of mitral regurgitation? What can cause this?
|
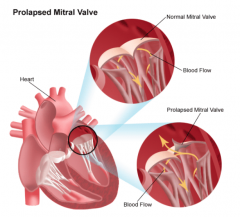
Mitral valve prolapse.
Excess tissue makes the valve floppy, May be associated with Marfan's and Ehler's Danlos |
|
|
What are some other causes of MR? Remember your anatomy
|
annulus - mitral annular calcifications
leaflets - MVP, rheumatic, endocarditis, systolic anterior motion chordae - rupture papillary - dysfunction, rupture LV - cavity dilation |
|
|
What is the pathophysiology (systemic consequences) of mitral regurgitation?
|
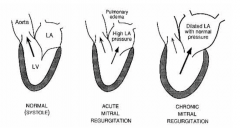
A portion of the LV stroke volume is ejected back into the LA during systole. As a result, forward CO is reduced. LA volume and pressure increase and volume related stress on LV - SV increases.
Over time, the dilated LA returns to normal pressure, the LV dilates and high SV maintained, leading to eventual LV failure. |
|
|
What are the typical presentations of acute and chronic mitral regurgitation?
|
ACUTE - Pulmonary edema leading to dyspnea, orthopnea, PND.
CHRONIC - Sx of low cardiac output, fatigue, weakness, SOB with exertion Once the patient starts to decompensate, they will begin to experience orthopnea, PND, Sx of right heart failure such as edema |
|
|
What is found with auscultation in mitral regurgitation?
|
- Pansystolic murmur at the apex radiating to axilla (most often)
- S1 may be soft (depending on etiology) - S3 present (chronic) - Displaced apex (chronic) - Signs of R heart failure if acute or decompensated chronic (elevated JVP, edema) |
|
|
What physiologic factor make MR better/ worse?
|
better - decreased afterload (medical interventions)
worse - increased afterload (hypertension, aoritc stenosis) |
|
|
What would you order to investigate mitral regurgitation?
|
"CXR - pulmonary edema if acute. If chronic, LA/LV enlargement
ECG - LA enlargement, LVH if chronic ECHO - important to evaluate LV size and function, mechanism and degree of MR. Cath - measure pressure, check coronaries, degree of MR |
|
|
What are the pharmacological treatments for mitral regurgitation?
|
ACUTE - diuretics and vasodilators
CHRONIC - some evidence for use of ACE-I (to reduce afterload) if HTN or LV dysfunction Surgery is usually recommended |
|
|
What are the criteria for surgery in chronic mitral regurgitation?
|
- Severity of symptoms
- Reduction in EF - LV dilatation - New-onset atrial fib / PHTN - Whether or not valve is repairable |

