![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
24 Cards in this Set
- Front
- Back
|
What is the most common cause of syncope in young adults?
|

Vasovagal syncope
(neurogenic) |
|
|
What are four non-syncopal causes of loss of consciousness?
|
1) Falls
2) Psychogenic ""pseudo-syncope"" 3) Seizures 4) Hypoglycemia 5) Intoxication |
|
|
What causes of syncope are most likely in younger patients? (3 main categories)
|
Neurocardiogenic (e.g. vasovagal)
Congenital or inherited heart disease (e.g. HCM, LQTS) Psychogenic causes (e.g. conversion disorder) |
|
|
What are the four most common etiologies of syncope in middle-aged patients?
|
Neurocardiogenic (vasovagal)
Orthostatic changes. Structural heart disease (CAD) Arrhythmias |
|
|
What are four common causes of syncope in older patients?
|
Orthostatic hypotension
Obstructive cardiac lesion Arrhythmias from structural heart disease Bradyarrhythmias |
|
|
What are the five broad categories for causes of syncope?
|
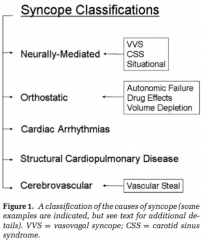
Neurally mediated
Orthostatic Cardiac arrhythmias Structural cardiopulmonary disease Cerebrovascular |
|
|
What are the three causes of Neurally mediated syncope?
|
Vasovagal
Carotid sinus syndrome Situational |
|
|
Name 3 triggers can lead to Situational syncope
|
micturition syncope
cough syncope defecation syncope cold to hot breath holding post-exercise post-prandial |
|
|
What is the mechanism for Carotid Sinus Syndrome syncope?
|
A hypersensitive carotid baroreceptor causes marked bradycardia with stimulation of the neck, leading to decreased cerebral perfusion and syncope.
|
|
|
For patients with syncope related to orthostatic hypotension, what are three different possible causes of their syncope?
|
Choose from:
Autonomic failure, (multiple system atrophy, Parkinson's with autonomic failure) Secondary autonomic failure (diabetic or amyloid neuropathy) Post-exercise or post-prandial deficits Drug-induced orthostasis Volume depletion |
|
|
Name three types of drugs that can cause orthostatic hypotension.
|
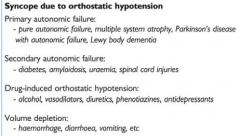
Alcohol,
Vasodilators, Diuretics, Phenotiazines, Antidepressants |
|
|
How can you narrow down causes of syncope in the physical exam? (give 2 tests/findings)
|
orthostatic blood pressures
carotid bruits parkinsonian features? normal cardiac exam? ECG |
|
|
A patient presents with a history of syncope. You've ruled out drugs or non-syncopal TLOCs. Name three elements of the history that can point to a cardiogenic cause.
|

Looking for history of:
MI, Heart surgery, Known valvular heart disease, History of palpitations, Family history or risk of inherited heart condition (sudden cardiac death, or known disease). Syncope on exertion, Syncope with chest pain, or other cardinal symptoms of CV disease. |
|
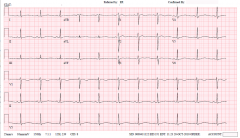
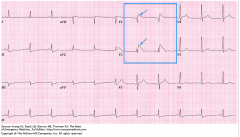
In a patient with recurrent syncope, what etiology is indicated by this ECG?
|
Analysing the ECG:
T-wave appears abnormal, looks like an abnormally prolonged QT interval, so you should work out the value of QTc: QTc = QT/sqrt(RR) QT = 0.56 s RR = 0.92 s QTc = 0.58 s A QTc of >0.46 s is prolonged in all age groups, so this ECG points to Long QT syndrome. |
|
|
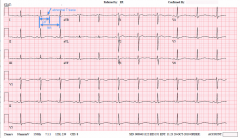
In a patient with recurrent syncope, what etiology is indicated by this ECG?
(hint: look at V1 and V2) |
The RBBB pattern, with ST elevation in V1 & V2 is indicative of Brugada Syndrome.
|
|
|
What is the main concern for patients with Brugada syndrome?
|
SCD
|
|
|
What causes of syncope can be picked up by an ECG or Implantable Loop Recorder (ILR)?
(give 3) |
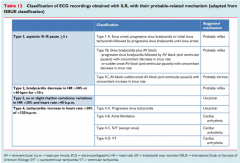
Some choices:
Sinus bradycardia, Conduction defects (BBBs, AV blocks), Long QT syndrome, Brugada syndrome Arryhthmogenic right ventricular dysplasia |
|
|
What causes of syncope can be picked up by an echocardiogram? (give 2)
|
Syncope due to:
Ventricular dysfunction, Valvular heart disease, Hypertrophic cardiomegaly, Other structural or flow-related defects (e.g. pulmonary hypertension, tumours, etc.) |
|
|
When might you initiate an exercise treadmill test in a patient with syncope?
|
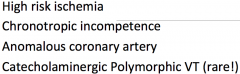
To confirm a history of exercise-induced syncope, and rule out some rare conditions, after other investigations have proven fruitless.
Practically, it is very rarely indicated in an investigation of syncope. |
|
|
What are three ways to non-pharmacologically help a patient avoid episodes of neurocardiogenic syncope?
|
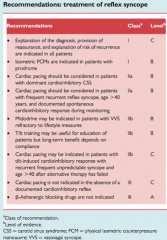
Many ways:
Avoid triggering events, Help them recognize premonitory symptoms (nausea etc) Teach them maneuvers to avoid the syncope (leg crossing, hand grip/arm tensing, adopting supine position) Avoid volume depletion, Avoid prolonged upright posture, or hot confining environments. Avoid vasodilator medications. |
|
|
What are two indications for an implantable pacemaker?
|
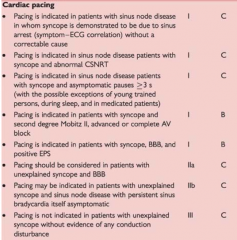
3rd degree and advanced 2nd degree AV block with symptoms.
Heart block with pauses >3sec or escape rate <40 Fascicular blocks with 2nd or 3rd degree block, or alternating bundle branch block, Syncope, thought to be heart block. |
|
|
What are the primary indications for an Implantable Cardioverter Defibrillator?
|
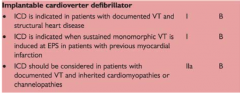
Patients with:
Documented VT and structural heart disease, An Electrophyisological Study (EPS)-induced monomorphic VT in patients with previous MI. Patients with inherited cardiomyopathies or channelopathies with documented VT. |
|
|
What is the goal of ICD therapy?
|
reduction in SCD
|
|
|
What is the advantage of biventricular pacing?
|
For patients with cardiac dyssynchrony (caused by bundle branch blocks, AV nodal dysfunction, with EF< 30%) it can improve:
Suboptimal ventricular filling, Reduced LV pressure rise, Mitral regurgitation, Septal dysfunction |

