![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
38 Cards in this Set
- Front
- Back
|
Define stenosis and atresia.
|
Stenosis is a narrowing.
Atresia refers to insufficient growth. |
|
|
What are the three main categories of congenital heart disease?
|
1. Cyanotic CHD
2. Acyanotic CHD 3. Obstructive |
|
|
Name at least three specific examples of cyanotic congenital heart defects.
|
Transposition of the great arteries
Tetralogy of Fallot Tricuspid atresia Truncus arteriosis Total anomalous pulmonary venous drainage Pulmonary atresia Single ventricle Ebsteins anomaly |
|
|
What is a tetralogy spell?
|
A life-threatening acute decrease in pulmonary blood flow. Systemic vascular resistence falls during the spell and pulmonary vascular resistence and subpulmonary contractions (muscle spasms) increase.
|
|
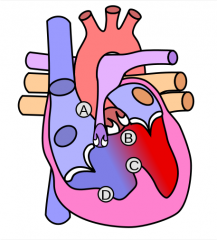
Name this syndrome and its features (A-D).
|
"Tetralogy of Fallot:
A. Pulmonic stenosis B. Overriding aorta C. Ventricular septal defect D. Right ventricular hypertrophy " |
|
|
What is the embryologic origin of all four defects in Tetralogy of Fallot syndrome?
|
Defect in the development of the aorticopulmonary septum - this deviates medially and superiorly.
|
|
|
How should you treat a tetralogy spell?
|
Increase systemic vascular resistence:
-knee to chest position, squatting -Phenylephrine -Fluid bolus Decrease pulmonary vascular resistence: -beta blocker (relaxes subpulmonary muscle) -morphine |
|
|
Describe the management of Tetralogy of Fallot.
|
Early treatment:
-if pt has severe cyanosis: prostaglandin -mild cyanosis: beta blockers -very mild cyanosis: (rare) CHF treatment Surgical repair at 4-6 months " |
|
|
How do you repair a ToF
|
removal of PV and repair of VSD
removal of pv causes "free" pulmonary insufficiency and leads to RV dilation and sometimes dysfunction over time |
|
|
Name two surgical repair options for transposition of the great arteries.
|
-balloon atrial septostomy
-transposition repair |
|
|
Name at least three specific acyanotic congenital heart defects.
|
ASD
VSD AVSD patent arterial duct |
|
|
Describe the treatment for ASD.
|
Surgical or interventional closure before age of 25 to prevent pulmonary HTN. Surgery is generally done at age 4 or 5.
|
|
|
Name at least two long term complications of unrepaired ASDs.
|
Pulmonary HTN
Stroke R heart enlargement Tricuspid valve insufficiency Rhythm disturbance (atrial) |
|
|
What is Eisenmenger's Syndrome?
|
Irreversible pulmonary HTN after prolonged L to R shunt (specifically, intimal proliferation and fibrosis).
|
|
|
List common signs of pulmonary hypertension.
|
clubbing
JVP changes RV heave and/or palpable S2 single, loud S2 ejection click from dilated PA |
|
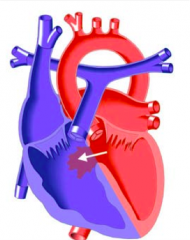
name this defect
|
VSD
|
|
|
In a pt with a VSD, which side of the heart is most likely to develop dilation and ventricular hypertrophy?
|
The left side - there is increased blood flow to the LA and LV.
|
|
|
When does a VSD usually present in an infant?
|
At approximately the of age 2-6 weeks, after PVR falls.
|
|
|
What are the three cardinal signs of heart failure in infants?
|
Tachypnea
Tachycardia Hepatomegaly Other signs of heart failure in infants include: -diaphoresis -pallor -displaced apex -active precordium |
|
|
What is the appropriate management of VSDs?
|
provide additional nutrition because of the increase in energy expenditure: high calorie feed, NG feeds
monitor and manage fluid balance with diuretics if necessary. vaccine against RSV (Respiratory syncytial virus) and influenza *note: ACE inhibitors, beta blockers and digoxin have not shown any benefit in pts with VSDs. |
|
|
What defect requires earlier intervention: ASD or VSD?
|
VSD - the defect should be closed at approx. 4-6 months of age. It is especially important to close before the age of one year if the defect is hemodynamically significant.
This is in contrast to ASDs which are generally closed at 4-6 years of age (and up to 25 years of age). |
|
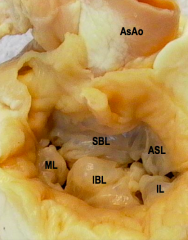
name this defect
|
AVSD
|
|
|
What are the clinical manifistations of AVSD?
|
Depends on the exact nature of the defect: if it involves the atria, the symptoms will resemble and ASD. If the AVSD involves the ventricles, it will resemble and VSD and if it involves both atria and ventricles, the VSD-type symptoms will dominate.
|
|
|
What kind of murmur will you hear in a patient who has Patent Ductus Arteriosus?
|
Continuous - blood is continually 'leaking' from the high resistence systemic circulation/aorta, into the low resistence pulmonary circulation/pulmonary trunk.
|
|
|
Which obstructive congenital heart defect is always progressive: aortic stenosis or pulmonary stenosis?
|
Aortic
|
|
|
What are common clinical findings in a patient with aortic coarctation?
|
-delayed or absent femoral pulses
-normal or strong radial/brachial pulses -radio-femoral delay -higher BP in right arm compared to legs |
|
|
Where will you hear a murmur caused by coarctation of the aorta?
where does the murmur of coarctation radiate and what other 2 murmurs radiate to the same place? |
LUSB, radiates to the back and can be heard interscapularly (is that actually a word?)
PS, and PDA |
|
|
What are some long-term medical and social issues to discuss with patients who have CHD and their families?
|
Medical: ongoing followup, nutritional support, scarring from surgery can lead to arrhythmias,
Social: psychological impact of having dangerous heart defect, employment counselling, increased risk of learning disabilities, risk of genetic reoccurrence in any future children, etc. " |
|
|
What is Kawasaki Disease?
|
Medium size vessel vasculitis of unknown origin that generally affects children under age 5.
-Japanese ancestry makes a patient more susceptible. -Can cause cardiac inflammation and coronary artery aneurysms |
|
|
How is Kawasaki disease diagnosed?
|
5 days of fever and 4/5 of:
-truncal rash -bilateral conjunctivitis (non-suppurative) -extremity changes: swollen, red, peeling -really dry and red mucous membranes -cervical lymphadenopathy |
|
|
Why is it so important to recognize and treat Kawasaki disease?
|
Because there is a risk of coronary aneurysms of up to 20-25%, if untreated. Treatment with IVIG and ASA drops this number to below 5%.
|
|
|
what are the common clinical features of TGA
|
significant desaturation 65-80%
on exam: normal pules and precordium Normal S1 Single S2 because AV and PV are directly anterior-posterior usually no murmur liver not enlarged |
|
|
clinical features of ASD
|
presents as an asymptomatic murmur
if there are symptoms they include: -SOB -exercise intolerance -frequent lung infections On exam: precordial bulge RV heave Normal S1, widely split and fixed S2 Systolic ejection murmur at the left upper sternal border (murmur comes though the PV not the ASD) |
|
|
What are the long term effects of unrepaired ASDs?
|
causes when defect is bigger than 2cm
right heart enlargement leading to RSHF, leaky tricuspid valve heart rhythm disturbances stroke PHTN |
|
|
what is the difference in the pathphys of VSDs compared to ASDs?
|
both depend on the size of the hole but in VSD another factor is the resistence of the pulmonary circuit and in ASD the other factor is relative compliance of the RV and LV
|
|
|
what are some common RFs for patent arterial duct and under what circumstances could it be a R-to-L shunt
|
hypoxia
acidemia structural anomaly R-to-L shunt at ductal level persistent pulmonary hypertension of the newborn |
|
|
clinical findinds in PDA
|
similar to VSD and AVSD
unique physical findings: active precordium with displaced apex wide pulse pressure bounding pulses continuous murmur |
|
|
what's different about left to right shunts above and below the tricuspid valve?
|
shunts above the TV cause RA and RV dliation
shunts below the TV cause LA and LV dilation |

