![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
179 Cards in this Set
- Front
- Back
|
Psychomotor agitation |
Excessive motor and cognitive activity, usually non productive and in response to inner tension. |
|
|
Psychomotor retardation |
Visible slowing of thought, speech and movements |
|
|
Catatonia |
Motoric abnormality |
|
|
Tics |
Involuntary, spasmodic motor movement |
|
|
Akathesia |
Subjective feeling of muscular tension, secondary to anti-psychotic medication. Can cause restlessness, pacing, repeated sitting and standing. |
|
|
Stereotypy |
Repetitive fixed pattern of physical action or speech. |
|
|
Tardive Dyskinesia |
Delayed effect of antipscyhotics consisting of abnormal involuntary, irregular choreathetoid movements. |
|
|
Echopraxia |
Pathological motor immitation |
|
|
Dystonia |
Prolonged contracts that cause twisting |
|
|
Affect |
the examiners observation of the patients current emotional expression |
|
|
Mood |
A patients subjective description of their feelings |
|
|
Range of mood MSE |
expansive, full, blunted or flat. |
|
|
Appropriateness of mood MSE |
congruent or incongruent |
|
|
Mobility of mood MSE |
Labile, normal or constricted. |
|
|
Speech MSE |
amount, rate, inflection, reciprocal flow, articulation |
|
|
Thought processes |
goal directed, circumstantial, tangential, flight of ideas, word salad, clang associations, neologisms, echolalia, blocking, magical thinking. |
|
|
Circumstantial thought process |
Indirect and delayed in reaching the point; characterised by over inclusion |
|
|
Tangential thought process |
Inability to have goal directed associations of thought, never get from thought to desired goal |
|
|
Loosening of associations |
Flow of thoughts shifts from one subject to another in a completely un connected way. |
|
|
Flight of ideas |
Rapid continuous verbalisations or plays on words that produce constant shifting from one idea to another |
|
|
Word Salad |
Incoherant mixture of words and phrases |
|
|
Clang associations |
Association of words with similar meaning but no logical connection |
|
|
Neologisms |
New words created by the patient |
|
|
Echolalia |
Pathological repeating of words and phrases of a noter person |
|
|
Blocking |
Abrupt interruption in train of thought before finished, no recall. |
|
|
Magical thinking |
belief that merely thinking about an event in the external world can cause it to occur |
|
|
Thought content |
Suicidal ideation, ruminations, obsessions, ideas of reference, delusions. |
|
|
Delusion |
fixed false belief about external reality |
|
|
Perception |
Hallucination, illusion, approriate, depersonalisation, derealisation, agnosia, synesthesia. |
|
|
Agnosia- |
can't recognise objects or people |
|
|
Synesthesia- |
sensation caused by another sensation. |
|
|
Benefits of watch, wait, wonder |
enjoy their child more stimulate their child’s creativity and imagination help their child to play more by themselves settle difficult behaviours, especially sibling rivalries and jealousies foster a surge in development.
Allows exploration and coming back, secure based attachment--> increase in pretend play |
|
|
How to do watch wait wonder |
“Non directiveness on the part of the mother is the only stringent requirement”.
Get down on the floor for half an hour daily and develop the presence of a “passive but gently reinforcing interest". |
|
|
Protective factors for children with parents with mental illness |
support groups, community involvement, tutoring, counselling, exploring understanding, roles and meanings.
social competence, attachment, empathy, optimism, school achievement, easy temperament, good coping skills, supporting caring parents, family harmony, secure and stable family, supportive relationship with other adults, sting family norms, positive school climate, pro-social peer group, sense of belonging, success at school, school norms on violence, meeting a significant person, moving to a new area, opportunity, support services, community networking, attachment to community, community group, |
|
|
Risk factors for kids with parents with mental illness |
low self esteem, poor social skills, difficult temperament, lack of empathy, family violence, poor supervision, harsh or inconsistent discipline, lack of warmth and affection, abuse and neglect, stigma, social isolation, poverty, school failure, bullying, rejection, divorce, death of family member, mental illness in family, homeless, neighbourhood violence and circle, lack of services, violent community |
|
|
Interpersonal strategies |
validation- convey respect for experience or perspective and their knowledge of their experience, show you value them and their concern is accepted.
Setting limits- identify behaviours you are unwilling to tolerate.
Encouraging- providing emotional support and assurance for their actions, behaviours and choices.
Advice- Recommending a course of action or choice.
Coaching- Instructing a client during activity. Demonstrating, guiding, prompting, when necessary.
Confrontation- to oppose or bring together for examination or compassion, present for acknowledgement or contradiction.
Reframing- providing alternative interpretations for behaviours, actions, performance patterns or skills.
Interpretation- conveys the therapist understands clint motivations.
Metaphors- transfer of meaning and a way of quickly grasping an object without explaining it with lengthy words.
Reality testing- counter obvious distortions or denials that clients may use. |
|
|
Self management strategies for psychosis |
Helps develop skills to reduce or prevent the possibility of having another relapse. The early warning signs are the very fist changes that occur when psychosis is returning. They can occur quite slowly.
Identify tiggers, early warning sings, actions to take, actions others need to take.
E.g. increased anxiety, difficulty concentrating, quiet and withdrawn, eating and sleeping patterns. - these will likely make a pattern during each onset.
This way early action can take place to prevent the relapse or reduce its severity. |
|
|
What is the MOHOST? |
The MOHOST has been developed to document and communicate to others a persons level of occupational participation.
Useful if they can't identify this themselves, or to further help people to understand how they work.
|
|
|
Breathing techniques are useful for... |
master slow and even breathing to make it more effortless. This diverts attention from external stimuli, reducing physical and thought activity. Reduces autonomic arousal.
For- portability, hyperventilate, quick way to fight situational stress. |
|
|
PMR is useful for |
detecting, attending to and systematically tensing up and releasing tension.
Useful for- easy and unthreatening, inexperienced, difficulty relaxing, somatic tension, muscle groups which are a source of tension. |
|
|
Visualisation is useful for... |
Creating a passive relaxing setting. Induce disengagement.
Useful- preadolescent, good at generating imagery, do not need highly structured. |
|
|
Self stigma is caused by? |
Society- people are aware of the negative stereotypes
Local community- some people will be careful about disclosure of mental illness
Using services- reluctant to have it known using mental health services
Individual- paying attention to personal appearance and manners so people will treat them normally
Family- Disappointment and lack of support
The workplace- colleagues doubt capabilities.
|
|
|
The impact of self stigma? |
Downgrading expectations and a loss of hope
Low confidence and self esteem, a sense of worthlessness and failure
Modifying and changing behaviours.
Withdrawal and social isolation
The openness dilemma- |
|
|
Therapeutic use of self |
1. recognition of the individuality of the client 2. respect for the dignity and rights of each person 3. empathy- entering the experience of another persons without losing their objectivity and sense of separateness- join in with the client and connect with their feelings, and emerge undamaged from the encounter 4. Humility- recognise the limit of ones knowledge and skills as a therapist 5. unconditional positive regard- concern for the client without making moral judgements regarding their thoughts and action 6. Honesty- telling the client the truth demonstrates respect 7. a relaxed manner 8. flexibility- ability to modify behaviour according to the demands of the situation 9. self awareness/insight 10. Humour- lightness of approach when needed facilitates the therapeutic process 11. self awareness- ability to reflect on ones own reactions to the world and the impact this might have. |
|
|
The DSM stands for |
Diagnostic and statistical manual of mental disorders |
|
|
Lithium |
is a drug used to treat mood disorders, in high dosages can be toxic, can cause abnormalities in babies if taken during pregnancy |
|
|
The mental illness prevalence is |
1 in 5 |
|
|
To be diagnosed with an anxiety disorder, excessive anxiety and worry must have been experienced for... |
6 months |
|
|
Which of the following symptoms are commonly seen in an individual who has been diagnosed with schizophrenia? |
Hallucination, disorganised speech, disorganised or catatonic behaviour. |
|
|
Principles of recovery x 6 |
1. uniqueness of the individual: not about cure, but about a meaningful, purposeful life; outcomes are personal and unique. 2. real choices: building on strengths; balance between duty of care and support to take positive risks. 3. Attitudes and rights: listening to; promote human nights; support engagement in meaningful activities; instil hope. 4. dignity and respect: respectful and honest interactions; respect for an individuals values, beliefs and culture; challenge discrimination and stigma. 5. partnership and communication: work in partnership; each individual is an expert in their own life. 6. evaluating recovery- ensure evaluation and that individuals can track their own progress. i.e. alienation to self discovery. |
|
|
Does the DSM 5 use an axial system? |
No. The axial system diagnosed peoples: clinical syndromes, any developmental/personality disorders, any physical conditions, severity of psychological stressors, global level of functioning. |
|
|
Changes in the DSM 5 |
OCD and related disorders now have their own category; disruptive mood dysregulation disorder (reduce bipolar diagnosis in children) |
|
|
Major depression diagnosis |
Five or more of the following symptoms; at least one being the depressed mood or loss of interest or pleasure. -depressed mood -markedly diminished interest of pleasure in activities -significant weight loss or gain -insomnia or hypersomnia -psychomotor agitation or retardation -fatigue or loss of energy -feelings of worthless ness or excessive or inappropriate guilt -diminished ability to think or concentrate -recurrant thoughts of death, suicidal ideation |
|
|
Prevalence depression? |
15% population 25% for women (post-natal impacts on this). |
|
|
Mean age of depression onset, who is it more common in, and what is the impact of socioeconomic factors? |
40
More common in people without close interpersonal relationships
No correlation with SES factors, more common in rural areas |
|
|
Possible causes of depression? |
Life events- stress, unemployment, abusive relationships
Personal factors- family history, personality (worrier, perfectionist), serious mental illness, drug and alcohol abuse
Biochemical- serotonin, norepinephrine and dopamine- main chemicals related to mood and motivation.
|
|
|
Prognosis for depression? |
Tends to be chronic with relapses, psychotic features indicate more severe illness, 10-15% commit suicide. |
|
|
Changes in: appearance, behaviour and conversation, affect, mood, perception, cognition, insight, judgement, rapport and safety in depression?? |
Appearance: disheveled, poor posture
Behaviour: more agitated, slower movements, poor eye contact.
Conversation: slowed rate, volume, content reduced.
Affect: blunted or down
Mood: told to us by person.
Perception: not impacted greatly
Cognition: not able to concentrate and focus
Judgement: self harm and suicide are not rational
Rapport: hard to develop
Safety: risk of being at harm or harming others |
|
|
Children and depression |
Children experience and manifest depression in similar ways to adults, albeit with some symptoms unique to their developmental age. |
|
|
Potential causes of depression in children? |
Attachment trauma, physical health, life events, genetic vulnerability, bio-chemical imbalance. |
|
|
Characteristics of the attachment system? |
Attachement style - is gradually patterned -predicts later life behaviour -generalises to other relationships -remains relatively stable over our life span -attachment is a life space contract |
|
|
What are the four attachment styles? |
secure attachment (55-65%); insecure ambivalent (5-15%); insecure avoidant (20-30%); disorganised (10-19%). |
|
|
Secure attachment |
Parent: emotionally available, nurturing, reliable source of comfort and protection
Infant: ability to self regulate, organise themselves in a relationship, trust in self and others. |
|
|
Insecure ambivalent |
Helicopter parenting
Parent: inconsistently emotionally unavailable, intrusive and inappropriate, low availability and neglect
infant: heightened distress, overly preoccupied with relationship, inhibited. |
|
|
Insecure avoidant |
parent- consistently emotionally unavailable, withdrawn, respond selectively, direct infants attention outwards
infant- over regulates, avoids relationships, precocious independence |
|
|
Disorganised attachment |
parent: inaccessible, affords little protection, reacts inn appropriately
infant- no ability to regulate, lack any organised strategy to regulate, bizarre incoherent behaviours
The aren't is the source of fear and haven for safety. Raised in the context of frightened (helpless withdrawn) or frightening (hostile-intrusive) parenting. |
|
|
Trauma in infancy |
closely associated with caregivers affect and availability to help them emotionally regulate.
Can be direct trauma- maltreatment effects of parental behaviour- frightened or frightening
|
|
|
2 patterns of traumatised infants |
1. high degree of dissociation and withdrawal 2. highly aroused and vigilant |
|
|
Traumatised children- characteristic behaviours |
-work hard to control situations -relish power struggles and have to win -feel empowered by saying no -poor response to dicipline -strongly hold a negative self concept -have very limited ability to regulate their affect -avoid fun and engagement -avoid needing others -avoid being praised -carry lots of shame |
|
|
0-3 mental health indicators |
regulation difficulties (sleep, feeding, arousal) failure to thrive disrupted attachment developmental delays
|
|
|
3-12 depression |
Behaviour- quiet, sullen, withdrawn, irritable, draws attention to self, changes appetite, fatigue and concentrating, reduced interest in activities,
emotion- sad and hopeless, worthless and guilt, crying, worrying, sensitive to rejection
statements- more vocal outbursts, evidence of negative cognitions, physical complaints increased |
|
|
12-18 depression |
behaviour- quiet, appetite, weight, sleep, alcohol, academic, sexual patterns, no energy, no pleasure in normal activities, no concentration, somatic complaints, withdrawal, aggression, giving away possessions
emotion- withdrawal, hopeless and helpless, crying , tearful, low self esteem, mood swings, guilt and remorse
statements- i just want to lay down and sleep forever, do you ever wonder what it would feel like to be dead, nobody would miss me if, death and suicide. |
|
|
comorbidity with child depression
Risks |
anxiety disorder, adhd, disruptive behaviour disorders, eating disorders, learning disorders, substance abuse
aborigninal, sexual identity issues, pregnant, family history, rural, medical problems |
|
|
Risk factors for depression in later life |
increase in physical health problems, chronic illness, social isolation, side effects of meds, change in living arrangements, reduced physical functioning, particular anniversaries and the memories they evoke.
It is the most common mental health disorder in the aged --> functional decline, poor quality of life, greater morbidity and mortality and greater healthcare utilisation. |
|
|
how is depression different in older people? |
less verbalisations of emotion or guild, mask it, preoccupied with somatic symptoms, cognitive impairment can be marked, hopelessness |
|
|
what may complicate the picture of depression in older people? |
thyroid disorders, cardiac problems, dementia, bereavement, anxiety, substance abuse, personality disorder, diabetes, psychosis, parkinsons |
|
|
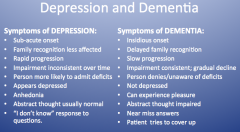
Depression and dementia |
|
|
|
Best practice for depression treatment: |
demotivation process, activity scheduling, social engagement, exercise, diet, problem solving therapy, CBT, interpersonal therapy, medication, ECT. |
|
|
What makes the difference between normal anxiety and anxiety disorders? |
When anxiety is ongoing beyond a stressful event, when it happens for no reason or when it significantly impacts on a persons occupational performance it is considered to be an anxiety disorder.
|
|
|
Anxiety disorder prevalence |
It is the most common mental health issue in australia. one in ten annually and 1 in 4 in a lifetime. |
|
|
What does anxiety disorders no longer include? |
PTSD and OCD. They have their own groups. i.e. obsessive compulsive and related disorders & trauma and stressor related disorders.
|
|
|
Treatment strategies anxiety |
CBT, relaxation, self help strategies, ACT, meds, narrative therapy, hypnotherapy, exercise and lifestyle approaches and psychoeducation. |
|
|
CBT |
An approach that is based on the premise that how we think influences how we feel. Ordinarily we might think situations directly predict our feelings and behaviour. In this process we challenge beliefs and thoughts, assessing if they realistic, accurate and helpful and reframing them if they are not.
A- situation B-beliefs and thoughts C- feeling and behaviour D-new beliefs and thoughts E- new feeling and behaviour. |
|
|
ACT |
acceptance and commitment therapy: To accept what is out of your personal control to do whatever is in your personal control to improve your quality of life. |
|
|
Bipolar 1 |
one or more manic episode or mixed episode of depression and mania |
|
|
Bipolar 2 |
one or major depressive episode and at least one hypomanic episode. |
|
|
Cyclothymic disorder |
fluctuating hypomanic and depressive symptoms not sufficient to meet other criteria for at least 2 years. |
|
|
Mania vs hypomania |
Mania- abnormally elevated, expansive or irritable mood (at least a week) PLUS things like: inflated self esteem or grandiosity, decreased need for sleep, rapid speech, psychomotor agitation, involvement in high risk activities.
Hypomania- less intense- periods of elevated, expansive or irritable mood, without marked impairment of social or occupational functioning.
|
|
|
Prevalence of bipolar |
varies depending on source. approx 2% lifetime. 65% have symptoms before 19. episodes can reoccur after many years. |
|
|
Etiology bipolar |
Stress may be a precipitating factor, genetic transmission is highly likely. if relative 5-10x greater risk. |
|
|
impact of bipolar on OP |
many have poor functional recovery even if meeting criteria for syndrome recovery.
6th most disabling condition
Likely to persist even with stabilised meds and mood
comorbid with personality disorders.
-wages, employment, work absenteeism -interpersonal relationships and divorce rates. - educational attainment -rates of arrest -general health, hospitalisation, premature death -emotional quality of life. |
|
|
subsyndromal symptoms and prodomal symptoms definition |
s- just fall short of meeting full diagnostic criteria for a mood episode p- precipitate the onset of affective symptoms. |
|
|
perspective of a person with bipolar |
1. routine is importnat - order in the chaos 2. independence- needing to have a sense of control 3. stigma and disclosure- most report being stereotyped 4. identity- build up self esteem so bipolar doesn't define them 5. social support- don't try to six them, just accept. 6. spirituality- difficulty disentangling real religious experience from hypereligisity .
|
|
|
what can impact the frequency of bipolar episodes? |
events that impact on sleep wake, goal related achievements, cognitive attributional styles, lack of social support. |
|
|
what improves long term outcomes for bipolar? |
integrated approach- combine meds with psychotherapy Psychotherapy should enhance med effect and improve adherence, reduce depressive symptoms, recognise early relapse, increase lifestyle regularity, lessen impact of stressful life events. |
|
|
therapy for bipolar |
psychoeducation- address taking meds, avoiding substance abuse, early symptom detection, coping, skills to cope with stress and interpersonal difficulties , decrease stigma family focussed interventions- family attitudes, reduce over involvement and high expressed emotion, stable routine, re-establish family relationships. CBT- challenge negative self statements, interpretations of life events. recognise prodomal, meds, lifestyle interpersonal and social rhythm therapy- helps recognise impact of interpersonal events on social and circadian rhythms. emphasises need for sleep wake cycle. clients keep detailed record of everything |
|
|
What is a community treatment order? |
A CTO enables a person who needs treatment for a mental illness who will not accept services voluntarily to be treated in the community. They can be treated for mental illness without consent if authorised by a psychiatrist who has examined the person.
It provides a framework to protect their rights |
|
|
What is the MOHO concerned with understanding? |
how people are motivated towards and choose the things they fill their lives with. how they learn and sustain patterns of doing that makes up everyday life. how are people about to engage in such a wide range of physical, cognitive and social action.
motivated, patterned and performed. |
|
|
What is volition? |
volitional thoughts and feeling pertain to: 1. personal causation- what people feel they can and can't do well. This is impacted by how effective we feel about our capacities, how effective we feel our efforts in our life how aware we are of potential abilities, whether we feel we can bring about what we want. 2. values- what they consider important. Impacted only what we think is worth doing, how it should be performed and what to commit to do. 3. interests- what they enjoy doing. This is generated by experiences of pleasure and satisfaction. Level of interest is based on the anticipation of a positive experience.
There is a cycle of anticipation, making choices, experiencing and evaluating. |
|
|
What is habituation? |
Refers to the process by which occupation is organised into patterns or routines. Much of what we do belongs to a taken for granted round of daily life. Includes two constructs- habits and roles.
Habits are semiautomatic patterns of behaviour what we have internalised through repeated performance. Organise and enable us to perform activities within our environment.
Roles shape sense of self and evoke behaviours. Without roles people lack identity and structure in their life. |
|
|
Performance capacity MOHO |
physcial and mental abilities that underly the ability to do. |
|
|
Environment MOHO |
plays a part in choices of doing, routine patterns of behaviour and performance. influence of culture, demands and contrasts, spaces and objects, impact of physical and social environments. |
|
|
Remotivation process |
Exploration- stages: validation; disposition for environmental exploration; choice making; pleasure and efficacy in action. Goal- facilitate a sense of capacity, a sense of personal significance and a sense of security with the env.
Competency: stages: meeting new performance expectations; increasing challenges and responsibilities within roles. Goals: developing a sense of efficacy, reaffirming capacity and control over decisions.
Achievement- stages: self monitoring and identification of critical skills; self advocacy. Goals: integrating new areas of OP into total life.V |
|
|
Volitional hierarchy |
?? |
|
|
Schizophrenia diagnosis |
A: Two or more of the following for a significant time in the past month. 1. delusions 2. hallucinations 3. disorganised speech 4. grossly disorganised or catatonic behaviour 5. negative symptoms i.e. affective flattening, alogia or avolition
B: social and occupational dysfunction. One or more of major areas of functioning are markedly below level achieved prior to onset.
C: Continuous in disturbance for at least 6 months. |
|
|
Conditions that may include psychosis |
depression, bipolar, schizoaffective, dru induced, neurological conditions |
|
|
Prevalence of schizophrenia? |
1% of population. All societies approx the same. Equally prevalent in men and women. men much earlier 10-25 and women 25-35. |
|
|
Etiology schizophrenia |
stress vulnerability model- symptoms develop in response to stress neurotransmitters- increase in dopamine psychosocial factors- numerous theories. Link with influenza in third trimester of pregnancy.
Genetics- identical twin 47%, two parents 40%, one parent 12% |
|
|
Course of schizophrenia? |
exacerbations and remissions. further deterioration in baseline functioning follows each relapse. positive symptoms tend to become less severe with time, negative symptoms tend to become more sever with time. |
|
|
Prognosis schizophenia: |
20-30% normal lives, 20-30% moderate symptoms 40-60% impaired entire life. 15% commit suicide.
Good prognosis- late onset, obvious precipitating facts, acute onset, good premorbid function, mood disorder symptoms, married, family history of mood disorders, good support, positive symptoms.
Poor prognosis- young onset, no precipitating facts, insidious onset,poor premorbid, withdraw, sinlge, family history, poor support, negative, relapses, |
|
|
Treatment of schizophrenia? |
Hospitalisation: diagnosis, stabilise, safety for disorganised and inappropriate behaviour Medication- oral and injection, many sir effects such as weight gain and diabetes. Social skills training. Psychoeducation Group therapy case management CBT
|
|
|
What can an OT do for schizophrenia? |
Graded program,MOHO, compensatory strategies. |
|
|
Complex trauma |
is a process and not an event. It has a pervasive neurobiological and socioemotional impact on OP. |
|
|
Types of stress. |
Positive stress: short term such as the challenge of doing a puzzle in the context of stable and responsive relationships. Tolerable stress: could potentially impact on brain circuits. More serious events- death, homeless, divorce. Can go back to baseline. Toxic stress: strong frequent exposure in the absence of support. Changes in brain architecture and lowers the response threshold. |
|
|
Neurobiological explanation of trauma |
Decrease in amygdala activation sustained cortisol secretion cortisol induced damage of neural circuits in the hippocampus which impacts on new memory and learning.
|
|
|
Traumatised infact characteristic behaviours |
learn to miscue caregivers. Present a cue that will regulate others emotion and hide their own need. This may be seen in infants who... - act as if they are independent and don't need their caregiver -act as if they can't separate from their caregiver -act as a carer to their caregiver -act bigger and stronger than their caregiver
Leads to... developmental delays (motor, language, social and cognitive), odd eating behaviours, odd soothing behaviours, indiscriminate attachment, aggression,
physical attributes (head circumference and height), cognitive function, language, socioemotional development and psychological adjustment. - attachment relationships, emotional recognition and regulation, self system development, school functioning, later romantic relationship.s |
|
|
Behaviour patterns of traumatised children |
-chronic vigilence- anticipates new trauma -compulsions to reenact loss -poor skills needed to create healthy attachment -mismatch with new relational experience. |
|
|
Impact on long term health related quality of life of trauma in childhood |
arthritis, high BP, asthma, bronchitis, autoimmune, cancer, PTSD, dissociative, anxiety, phobias, substance abuse, depression, increased suicide risk. |
|
|
Cognitive, socioemotional and psychological impacts of trauma |
hyperarousal- hypervigilence, emotional tantrums, anxiety. Role of social information processing (negative attribution bias).
Hypoarousal- flat affect, numbness, feeling detached, passive aggression.
Emotional dysregulation and difficulty with identification and expression of emotions. Role of sensory thresholds.
There is strong evidence that the shame humiliation dynamic accompanies child abuse. |
|
|
Traumatised adults will have... |
intrusion of traumatic memories hyperactivity and hyper vigilence compulsive exposure to dangerous situations- reenactments. dissociation- altered ability to attend and process info loss of trust in world poor self perception extreme difficulty with emotional regulation split off parts of self. |
|
|
Disorders in traumatised adults |
PTSD, anxiety, phobias, substance abuse, depression, increased suicide risk, dissociative identity disorders, personality disorder, particularly BPD. |
|
|
PTSD |
A person witnesed/ experienced trauma- which threatened death or physical safety.
Traumatic event re-experienced through- recurrent, intrusive, distressing recollections. recurrent distressing dreams acting or feeling like the event is reoccuring intense psychological distress as exposure to cues physiological reactivity to cues
Persistant avoidance of stimuli associated with trauma
persistant symptoms of increased arousal
duration more than one month
Causes significant distress or impairment in social, occupational or other areas of functioning.
|
|
|
Dissociative identity disorder |
the presence of 2 or more distinct identities or personality states
with at least 2 of these identities or personality states recurrently taking control of the persons behaviour
inability to recall important personal information
not due to the direct physiological effects of a substance or a general medical condition. Symptoms in children are not imaginary playmates or imaginative play. |
|
|
Trauma intervention |
CBT- correcting the painful and intrusive patterns of behaviour and though by challenging mental processes causing the problem dialectical behaviour therapy exposure therapy psychodynamic psychotherapy - focuses on helping the individual examine personal values and how behaviour and experience during the traumatic event affected them. family therapy- may also be recommended because the behaviour of spouse and children may result from and affect the individual groupwork- share. realise many people are the same medication- controls some of the symptoms attachment based interventions e.g. circle of security |
|
|
the three stages of treatment model for trauma |
Stabilisation processing and grieving reconnection |
|
|
Trauma and emotional development- child who has experience trauma may... |
attribute hostile intent to others, have difficulties in accurately identifying emotions in others, dissociate to avoid painful experiences, be hypervigilent. Disruptions in emotional development may result in long term difficulties in emotional regulation |
|
|
Two new subtypes of PTSD in DSM5 |
preschool subtype, PTSD dissociate subtype - prominent dissociative symptoms (feeling detached from mind or body) -or experiences in which the world seems unreal |
|
|
What is emotion? |
An evaluative mental state produced by a neural impulse. It is different from a feeling. Includes: physiological arousal, subjective experience, behavioural or affective expression, and cognition. Involves the nervous and endocrine systems emotional stress plays a large role in the development of many physical and mental illnesses and disease. Emotional stress- a sustained, damaging emotional response and the inability to control such responses. |
|
|
What is emotional regulation? |
The ability to control emotional states, very important for successful OP. Includes ability to: -inhibit inappropriate behaviour -accept and experience negative emotions -act to attain external goals, regardless of mode state -self soothe physiological arousal -refocus attention, despite having strong emotions. |
|
|
What is emotional dysregulation? |
Emotional responses that are maladpative prevent the person from reaching their goals often negative, but can also be positive impairment in modulation of emotion, i.e. intense feelings are retained beyond what might be considered usual, there is an inability to accept it and move on. |
|
|
Emotional regulation and mental illness |
borderline personality disorder, substance abuse, bipolar disorder, disruptive behaviour disorders. |
|
|
Personality disorder are... |
An enduring pattern of inner experience and behaviour that deviates markedly from the expectations of the persons culture, is pervasive and inflexible, has an onset in adolescence or early adulthood, is stable over time, and leads to distress or impairment.
- largely unchanged criteria. |
|
|
Personality disorder clusters |
A- paranoid, schizoid and schizotypal; discomfot in interpersonal situations, emotionally distanct, distrustful and sustpicious; 5.7% prevalence.
B- antisocial, borderline, histrionic and narciccistic. Expressive and unstable expression of emotions, difficulties in relationships, disregard for needs of others. prevalence 1.5%
C- avoidant, dependent, obsessive compulisive. Anxiety is a key issue e.g. fear of rejection or humiliation, preoccupation with perfection. prevalence 6%. |
|
|
Personality disorder impact on OP |
social skills, emotional modulation, coping.
--> social participation, rest and sleep, work, play and leisure. |
|
|
Borderline personality disorder |
-frantic efforts to avoid real or imagined abandonment -pattern of unstable and intense interpersonal relationships -identity disturbance -impulisivity in at least tow areas that are potentially self damaging -recurrent suicidal behaviours, threats, gestures or self-mutilitating. -affective instability to marked reactivity of mood -chronic feelings of emptiness -innappropirate intense anger or difficulty controlling anger -stress related paranoid ideation or severe dissociative symptoms. |
|
|
BPD traits and mohost oncepts |
motivation for occupation- will be influenced by frantic efforts to avoid real or imagined abandonment and indentity disturbance, problems with self and chronic feelings of emptiness, transient stress related paranoid ideation and sever dissociative symptoms.
pattern of occ- will be influenced by pattern of intense and unstable relationships, impulsivity and recurrent suicidal or parasuicidal behaviour.
comm and interaction skills- influenced by affective instability and inappropriate intense and uncontrollable anger.
process skills- influenced by ............ |
|
|
Impact on OP BPD |
Motivation for occupation- all areas affected
pattern of occupation- habits and routines affect work, adls etc.
communication and interaction skills- instability and uncontrollable anger impacts all.
process skills- impacted by dissociation and impulisivity which in turn affects work, rest and relaxation
|
|
|
Personality disorder intervnetions- |
medication- treat symptoms interpersonal approach important- limit setting, reality testing CBT and inpartibcular DBT OT- important to have an consistent collaborative therapeutic relationship that validates and builds motivation for change.
Address Occ dysfunction- leisure, work, social participation, self care
prevention
|
|
|
Dialectical behaviour therapy BPD |
They feel discouraged by constant focus on change in CBT, and that their suffering was underestimated.
DBT validates the persons emotional functioning -core mindfulness, distress tolerance, interpersonal effectiveness, emotional regulation skills. |
|
|
Prevalence of behaviour and emotional problems in children 4-17 |
one in 7. fewer than half receive needed help, about half of children's problems will persist, current service system cannot effective respond to needs of children and families. |
|
|
Children behavioural, emotional and ASD problems. |
behavioural- conduct disorder, ADHD, oppositional defiant disorder.
emotional- anxiety, fears and phobias, depression and anxiety.
ASD- autistic disorder, aspergers disorder, childhood disinitegrative disorder and pervasive developmental disorder not otherwise specified.
|
|
|
Conduct disorder |
Chronic behaviour problem e.g. impassive or defiant behaviour, drug use, criminal activity, can be encopresis.
Severe symptoms have the poorest outlook.
prevalence- 1-4% of 9-17 year old.
Associated with later personality disorder (e.g. antisocial personality disorder),, depression and bipolar.
Challenges for OP- difficulty following procedures in class/ at work (e.g. punctuality, taking direction). |
|
|
ADHD |
Difficulty with inattentiveness, over activity, impulsivity or a combination. Must be outside of normal range for a childs age and development.
Prevalence- 3-5% school aged.
--> drug abuse, academic difficulties, difficulty maintaining a job, criminal activity. |
|
|
oppositional defiant disorder |
pattern of disobedient, hostile and defiant behaviours towards authority figures. Can include encopresis.
e.g. do not follow requests, angry and resentful, argues, blames others, has few or no friends, in constant trouble, loses temper, spiteful,
Prevalence hard to obtain. Starts by 8 sometimes younger. . Needs to be present for at least 6 months and beyond normal behaviour. |
|
|
Internalising problems children |
anxiety- need to clearly differentiate from ADHD Depression- difficult to diagnose because of normal mood swings. Epsides often continue into adulthood. Children are more likely to have other more sever illnesses in adulthood, oy pretend to be sick, refuse to go to school et.c |
|
|
Other mental health disorders in children |
PTSD, attachment disorder (emotional withdrawn or inhibited, indiscriminant or disinhibited or combination), eating disorder, personality disorder.
Schizophrenia- is rare in children 1 in 40,000.
Bipolar- early onset, can be more sever than bipolar disorder in teens and adults. Switch moods often. Co-occur with substance abuse, ADHD and anxiety. |
|
|
Risk factors for mental illness in children |
parenting practices- harsh/overprotective insecure attachment relationships innate temperment parents mental health problems childs sleep habits family stress and trauma preventive work in early childhood most cost effective. |
|
|
Interventions for children with mental illness |
greater emphasis on prevention and early intervention parenting programs early visitation programs play therapy/ psychotherapy focus on OP and increasing sense of self efficacy sensory processing dyad based therapy
watch wait and wonder.
PLACE. playfulness, love, acceptance, curiosity and empathy. |
|
|
Directive vs non directive approach with traumatised children |
a directive approach- the therapists is in charge yet.
non directive- a need to be responsive to the movement with an empathetic stance
focus needs to be relationship centred and curiously and playfulness.
an emotional richness to the interaction with a focus on the attachment sequences to asset in the processing of trauma in the relationship. |
|
|
Principles of therapeutic focus- dyad therapy |
ensure safety for adult / child and infant. restore sense of self by validating experience increase capacity to manage feelings and sensory memories and manage arousal levels. integrate trauma memories into self narratives. mourn losses development of self in relationships supper healthy formation of relationships. |
|
|
therapy for children involves... |
creating a safe space, moving from parent to baby and back again, acknowledging that everything in the room is intentional communication, working with the minutia, working with defences, creating a new experience, providing guidance.
The focus on relationship is key- empathetic, sensitive to attunement, support emotional regulation, predictable and consistent, work to understand childs experience and create meaningful behaviour, curiosity and playfulness |
|
|
Time out for caregivers
Time in |
when caregiver and child are upset, not as a punishment, use until they can be bigger, stronger, wiser and kidder. Limit time out to reduce the message of rejection.
When the parent is calm and the child is upset- take charge so the child is not too out of control, stay with the child until their feelings start to change, use a calm firm kind reassuring voice, give worlds for the feeling of the child and self
When angry- foster attachment, offer empathy to maintain emotional bond.
Help the child to think- |
|
|
Sensory based interventions in children |
used broadly in mental health. deep reassure are begin used as an alternative to seclusion and restraint in psychiatric facilitaties.
many different theories. sensory sensitive, sensory avoiding, low registration, sensation seeking. |
|
|
alcohol and drug use prevalence |
1/2 12 plus use alcohol in last 30 days.
8.3% illicit drugs in last 30 days. |
|
|
The impact of substance abuse in adolescence |
cognitive development, moral development and identity. |
|
|
Alcohol |
is a depressant. Can cause nausea, vomitting, hangover, unintended sexual activity. |
|
|
What is binge drinking? |
4 drinks in one setting, often linked to violence |
|
|
Cannabis |
is a depressant. can be hallucinogenic, linked to psychotic behaviour, have to have genetics as well, very affordable, |
|
|
Other depressant illicit drugs |
inhalant and benzodiazepines. |
|
|
Ectasy |
is a stimulant. Increased confidence and energy, anxiety, paranoia, aggression and psychosis, moor muscle control and unsteadiness, nausea, loss of appetite, increase in body temp, skin tingles, dilated pupils, heightened sensation, jaw clenching, teeth girding. |
|
|
Cocaine |
stimulant. can cause overdose. Usually snorted but can be injected. Higher doses- anxiety, sleep disorders, paranoia, tenors and muscle twitches, nausea and vomiting, rapid and weak pulse, chest pain, heart attack, kidney failure, hypothermia, seizures, increased heart rate and body temp, brain haemorrhage, stroke and convulsions. |
|
|
Coming down off cocaine |
tension and anxiety, radical mood swings, depression, total exhaustion. --> depression, anxiety, paranoia and psychosis, eating disorders and weight loss, hallucination, cerebral atrophy and impaired thinking |
|
|
Amphetamines |
are stimulants.
--> blurred vision, tremors, irregular breathing, loss of coordination, collapse, rapid pounding heart, violent or aggressive behaviour, hallucinations, seizures, stroke, coma.
Coming down- feeling restless, anxious, aggression, tension, radical mood swings, depression, paranoia, lethargy and total exhaustion.
--> depression, anxiety and tension, paranoia, violence, panic and confusion, poor memory and concentration. |
|
|
Most common illicit drug over 14 years?
Drugs most serious concern for the general community
Drugs that cause the most deaths over 14 |
cannabis,
alcohol.
alcohol and cannabis.
|
|
|
The effect of alcohol |
7000 hospitalisation, 300 deaths, 30% of serious road accident, 34% falls and drawing, 44% fire injury, 16% child abuse, 12% suicide, 10 % industrial accidents, depression,
70% of prisoners drunk it before their offense - victim reported crime, serious and minor assaults. |
|
|
Co-occuring disroder |
substance related disorders and mental health disorder. There is controversy over cause and effect. Complicated by homelessness, incurceration, infectious disease, trauma and PTSD. |
|
|
Indigenous mental health and substance abuse |
more indigenous abstain than non indigenous. However if they drink they are more likely to drink to harmful levels. Illicit drug use rates are twice those of non indigenous. --> violence, social disorder, family breakdown, child neglect, loss or diversion of income, and imprisonment. |
|
|
substance abuse and suicide |
indigenous 3 times the rate than non indigenous. Alcohol related deaths are common. data obtains through cause of death and hospital admission is only the tip. |
|
|
suicide prevention 7 goals |
to provide a socially inclusive community of resilient individuals and supportive environment.
to provide a sustainable, coordinated approach to service delivery, resources and info within communities to prevent suicing
to provide targeted suicide prevention initiates, activities and programs
to address, as a priority, the issues that affect regional south australia,
to provide targeted postvention activities and programs.
to improve the evidence base and understanding of suicide and suicide prevention
to implement standards and continuous practice improvement in suicide prevention. |
|
|
mental health first aid, signs of suicidal. |
-threatening to hurt or kill themselves. -looking for ways to kill themselves -talking or writing about death, dying or suicide -hopelessness -rage, anger, seeking revenge -acting recklessly or engaging in risky activities, -feeling trapped, like there is no way out - icnreasing alcohol and durg use -withdrawing from friends, family and society, -anxiety, agitation, unable to sleep or sleeping all the time. -dramatic changes in mood -no reason for living. M |
|
|
Motivational interviewing- |
psychological treatment, non confrontational approach, focuses on collar, considered a good fit for young people.
Types of questions: evocative, elaborative, examples, looking back, look forwards, queires, rainy scales, explore goals and values.
|
|
|
What is a comorbidity? |
the presence of more than 1 distinct condition in an individual. |
|
|
Common comorbidities |
major depression, adhd, GAD, panic attacks,
2/3 mdd and gad, sad or ptsd have their anxiety disorder first.
eating disorders and borderline personality disorder
PTSD and substance abuse. |
|
|
forensic mental health- patent perspectives |
- chronic mental illness or treatment resistant -cognitive defecits. -homelessness -poor functioning in a variety of areas -poor impulse control -non compliance with remediation attempts -substance abuse |
|
|
What is grief? and how is it experienced? |
grief is an emotional reaction to loss.
emotionally- sadness, anger, guilt and anxiety physically- hollow stomach, tight chest, short of breath. cognitively- disbelief, confusion, preoccupation behaviourally- sleep, appetite, withdrawal, loss of interest, crying, hostility socially- relationship difficulties spirituality- loss of meaning, anger at god. |
|
|
what is bereavement? |
reaction to loss. includes emotional and physical reactions to grief and mourning. letting go of relationships, state of being. |
|
|
What is mourning? |
behavioural action. Integration of grief and bereavement,opportunity for healing and growth, culturally driven, includes rituals and tasks associated with the death of loved one. |
|
|
Grief for family members with serious mental illness |
adjustment to loss of normality, worry about the future, lack of control, upset by changes yet resentful of demands/ needs. Siblings fear they are at risk, lose reciprocity in the relationship. Children feel different from their peers, awkward, avoid from bringing friends home, stigma. |
|
|
Define recovery |
mental health recovery is a journey of healing and transformation enabling a person with mental health problem to live a meaningful life in a community of his or her choice while striving to achieve his or her full potential.
It should be self directed, individualised, empowerment, holistic, nonlinear, strengths based, peer support, respect, responsibility, hope. |

