![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
42 Cards in this Set
- Front
- Back
|
What is Intrapleural Pressure (Pip) |
pressure in space between parietal & visceral pleura (also fluctuates with breathing) (~ slight vacuum) |
|
|
Pressure Relationships |
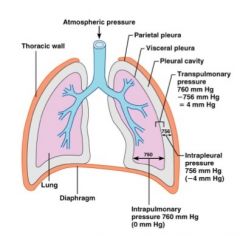
• Intra-alveolar pressure and intrapleural pressure fluctuate with the phases of breathing |
|
|
What is lung collapse? |

caused by equalization of intrapleural pressure with intra-alveolar pressure |
|
|
pneumothorax |
air enters intrapleural space |
|
|
Gas exchange in the lungs occurs because of partial pressure differences... |
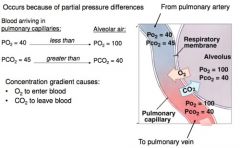
• O₂ to enter blood |
|
|
Gas exchange at the tissues occurs because of partial pressure differences... |

• O₂ to enter tissues |
|
|
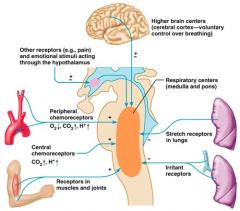
Control of Respiration involves neurons in the: |
medulla and pons |
|
|
Control of Respiration in the medulla ..... |
sets respiratory rhythm |
|
|
Control of Respiration in the pons ..... |
influences and modifies activity of medullary neurons |
|
|
What are the two respiratory groups of the Medullary Respiratory Centers? |

Ventral Respiratory Group & Dorsal Respiratory Group |
|
|
Ventral Respiratory Group (VRG) |

• Rhythm generating |
|
|
Dorsal Respiratory Group (DRG) |

• Integrates input from: |
|
|
Pons Respiratory Center |

• influences & modifies activity of medullary respiratory center |
|
|
DRG & pons respiratory centers receive info from _____ & _____ |
DRG & pons respiratory centers receive info from peripheral receptors & higher brain centers |
|
|
Breathing rate |
determined by how long inspiratory center is active (breaths per minute) |
|
|
Breathing depth |
more stimulation → more motor units excited → greater force of breath |
|
|
Factors that include breathing rate & depth are: |
• Chemical**** |
|
|
Chemoreceptos |
sensors that respond to chemical flucuations |
|
|
What are the two chemoreceptors? |
central chemoreceptors & peripheral chemoreceptors |
|
|
What are the two locations of the chemoreceptors? |
• central chemoreceptors - medulla |
|
|
Factors influencing breathing rate and depth: PCO₂ |
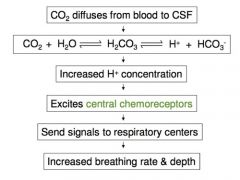
• CO₂ - most potent and closely controlled chemical |
|
|
Hyperventilation |
increased depth and rate of breathing |
|
|
Hypoventilation |
slow and shallow breathing due to abnormally low PCO₂ levels |
|
|
Apnea (breathing cessation) |
may occur until PCO₂ levels rise |
|
|
Peripheral chemoreceptors |
in aortic bodies & carotid bodies |
|
|
Factors influencing breathing rate and depth: arterial pH |
central chemoreceptors and peripheral chemoreceptors |
|
|
Central chemoreceptors |
insignificantly affected by H+ from arterial blood |
|
|
CO₂ and H+ are _____ → but they are distinct stimuli |
• Drop in pH may reflect an increase in CO₂ but... |
|
|
Body compensates for low pH by eliminating _____ by increasing breathing & respiratory rate. |
CO₂ |
|
|
Body compensates for low pH by eliminating CO₂ by increasing breathing & respiratory rate. |
CO₂ + H₂O ⇋ H₂CO₃ ⇋ H+ + HCO₃- |
|
|
Inflation reflex (Hering-Breuer reflex) |
stretch receptors in airways respond to changes in lung volume |
|
|
Pulmonary irritant reflex |
irritating physical/chemical stimuli in nasal cavity, larynx, and bronchial tree |
|
|
Factors influencing breathing rate and depth |
enter here |
|
|
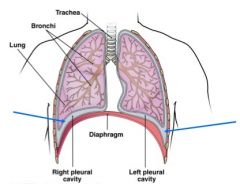
What structures make up the conducting zone of the respiratory system and what is the conducting zones purpose? |
- Structures: Pharynx, Larynx, trachea, and the brachail tree.
- Function: To conduct air into and out of the lungs. Also, serves to condition the air. |
|
|
What structures make up the respiratory zone and what is their purpose? |
- Structures: Alveoli and respiratory branchiols -Function: gas exchange |
|
|
What is the Bronchial tree? How are bronchioles different from bronchi? |
- Highly branched tubes of the lungs/respiratory system. As these tubes become smaller they lose cartilaginous support and gain more smooth muscle proportionally.
- Bronchi: larger tubes w/ cartilaginous support - Bronchioles: Smaller tubes w/o cartilaginous support |
|
|
Alveoli |
- spherical air filled structures at the end of the bronchial tree in clusters called alveolar sacs. Very compliant. Covered w/ pulmonary capillaries.
- Type I alveolar cells: Make up the walls of the aveoli.
- Type II alveolar cells: Not a part of the walls of the aveoli. Secrete surfactant. |
|
|
Respiratory membrane |
- Barrier to gas exchange in the lungs. Comprised of the Type 1 alveolar cells, endothelial cells of the capillaries, and the basement membrane that holds them together. |
|
|
Parietal pleura |
Membrane inside of the ribs |
|
|
Visceral Pluera |
Membrane on the outside of the lungs |
|
|
Intrapleural space |
the area in between the parietal and visceral pluerae. |
|
|
Pleural Fluid |
Fills the intrapleural space |

