![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
142 Cards in this Set
- Front
- Back
|
What are the major components of bone? |
Bone Cells, Osteoid, hydroxyatiles (mineral salts), Ca Phosphates |
|
|
What are the three types of cartilage and there function? |
1) Hyaline: Support, flexibility and resilience
2) Fibrocartilage: Absorb heavy forces, resist stretching.
3) Elastic) Allows for repeated bending |
|
|
Osteogenic Cell |
Bone stem cell |
|
|
Osteoblast |
Cell responsible for the formation of the matrix during bone growth. |
|
|
Osteocyte |
mature bone cell that maintains the bone matrix |
|
|
Osteoclast |
Bone resorbing cell |
|
|
Intramembranous Ossification (6 steps) |
1) Mesenchymal cells produce fibrous membrane 2) ossification center appears with osteoblasts 3) bone matrix is secreted 4) woven bone and periosteum form 5) Compact bone (lamellar) forms 6) Red marrow apears in spongy bone |
|
|
endochondral ossification (7) |
1) Formation of a bone collar 2) cavitation of the hyaline cartilage and matrix deteriorates 3) invasion of the internal cavities by periosteal bud and spongy bone formation. 4) formation of the medullary cavity 5) secondary ossification centers form in the epiphyses 6) ossification of the epiphyses 7) hyaline cartilage remains only in the epiphyseal plates |
|
|
What hormones are important for bone growth in infancy/childhood versus puberty |
Infancy/ childhood = growth hormone and thyroid hormone
puberty= testosterone and estrogen |
|
|
Diaphysis |
Tubular shaft, exterior is compact bone, and the medullary is yellow ( fatty) marrow. Ends of long bones |
|
|
Epiphysis
|
Expands ends of long bones, Exterior is compact bone, interior is spongy bone, joint is covered with articular cartilage, the epiphyseal line seperates the epiphysis and diaphysis.
|
|
|
periosteum |
Outer layer contains connective tissue
Inside layer contains osteoblasts and osteoclasts |
|
|
endosteum |
layer covering internal bone surfaces. contains osteoblasts and osteoclasts. Lines canals of compact bone and lines trabeculea of spongy bone |
|
|
Yellow Marrow |
Mainly fat cells |
|
|
Red Marrow |
Marrow that gives rise to blood cells |
|
|
Wolff's Law |
Bones grow in response to the forces played upon them. Bones atrophy when they are not used. |
|
|
Control of blood Calcium |
When levels our below normal, parathyroid hormone is released and osteoclasts remove calcium from bone |
|
|
Stages of bone healing |
1) Hemotoma formation: torn vessels hemorrhage 2) Fibrocartilaginous callus forms splint across fracture. New vessels are formed and phagocytes remove debris. fibroblasts secret collagen. Osteoblasts secret spongy bone 3) Fibrocartilaginous callus converts into bony callus 4)Excess materials is removed. Compact bone is formed to form shaft walls. |
|
|
Osteoporosis |
Bone resorption is faster than bone deposition. Postmenopausal women are at the most risk. The spongy bone of the spine is the most at risk location in the skeleton. |
|
|
osteomalacia |
Main symptom is pain in when doing weight bearing activities. Inadequate mineralization of bone. Caused by a lack of calcium and/or vitamin D. |
|
|
rickets |
The bones of childern are inadequately mineralized causing them to be weakened. bowed legs, deformities of the pelvis, rib cage and skull are all common. Caused by a lack of calcium and/or vitamin D. |
|
|
Drawfism |
Genetic deficiency in growth hormone |
|
|
Three types of structural joints |
1)Fibrous (Skull bones,tibia-fibula ligaments) 2) Cartilaginous (ribs, vertebrae) 3) Synovial (limb joints) |
|
|
Three types of functional |
1)Synarthroses- immoveable 2)ampiarthroses- slightly moveable 3)diarthroses- freely moveable |
|

|

|
|
|
What increases the stability in synovial joints? |
1) shape of articular surfaces 2) ligaments 3) Muscle tone |
|
|
Shoulder Joint |
Ball-and-socket joint Problem: as freedom of motion increases, stability decreases. Stabilizing structures Thin, loose joint capsule Four ligaments, tendon of the long head of biceps, Rotator cuff (four tendons) encircles the shoulder joint and blends with the articular capsule |
|
|
hip Joint |
Ball-and-socket joint Limited by the deep socket and strong ligaments More protected than shoulder |
|
|
knee Joint |
Largest and most complex joint of the body
Allows flexion, extension, and some rotation
Three joints surrounded by a single joint cavity |
|
|
Gouty Arthritis |
Body is unable to excrete or break down uric acid Uric acid deposits in joints and soft tissues
Uric acid crystallizes (especially at cooler temperatures) Large toe generally affected first
Males and postmenopausal women at higher risk
Crystallization prompts an inflammatory response If untreated, the bone ends fuse and immobilize the joint
Treatments anti-inflammatory drugs Diet (avoid alcohol and foods with high purine content) |
|
|
Rheumatoid Arthritis |
Chronic, inflammatory, autoimmune disease
Usually arises between the ages of 40 to 50
Women at higher risk
Conservative therapy: pain relievers physical therapy
Aggressive treatments: anti-inflammatory drugs immunosuppressants drugs that neutralize inflammatory chemicals
|
|
|
Osteoarthritis |
“wear-and-tear” arthritis
Affects women more than men
More prevalent in the aged |
|
|
Tendonitis |
Inflammation of tendon sheaths
Typically caused by overuse Symptoms
Treated with anti-inflammatory drugs |
|
|
Bursitis |
Usually caused by a blow or friction
Symptoms are pain and swelling
Treated with anti-inflammatory drugs
Excess fluid may be aspirated |
|
|
abduction |
Movement of a body part away from the median plane |
|
|
adduction |
To draw inward toward the median axis of the body or toward an adjacent part or limb |
|
|
circumduction |
circular movement of a limb |
|
|
Sprains |
The ligaments reinforcing a joint are stretched or torn
Partially torn ligaments slowly repair themselves
Completely torn ligaments require surgical repair |
|
|
Subluxation |
partial dislocation of a joint |
|
|
Muscle cramps |
Sudden, involuntary contractions of skeletal muscle
Generally caused by over-exertion, dehydration, poor blood flow or ionic imbalance
Generally short-lived |
|
|
Isotonic contraction |
Tension remains unchanged and the muscle's length changes |
|
|
Isometric contraction |
one in which the muscle fires but there is no movement at a joint |
|
|
Osgood-Schlatter disease |
Painful swelling of the bump on the anterior tibial tubercle. Appears related to overuse or repetitive injuries during growth Ex.) Imbalance in flexor/extensors (i.e. overdevelopment of quadriceps muscle)
Frequently seen in youth sports (soccer, basketball, volleyball)
Males generally at higher risk
Treatment: rest and reduce stress |
|
|
|
Involuntary contractions of skeletal muscle
Multiple causes including genetics
Apparently involves miscommunication between brain and muscles
Symptoms include tremors and twitching |
|
|
What causes Duchennese's muscular distrophy |
Muscle tissue replaced by fat and connective tissue deposits
Progresses from the extremities upward
Patients die of respiratory failure in their 20s
Caused by a lack of the cytoplasmic protein dystrophin
Inherited, sex-linked disease
Mother-son transmission |
|
|
What are the three types of muscles? |
1) Smooth-non-striated and involuntary 2) Skeletal- striated and voluntary 3) Cardiac- striated and involuntary |
|
|
Sarcolemma: |
muscle plasma membrane |
|
|
Sarcoplasm: |
cytoplasm of a muscle cell |
|
|
Sarcoplasmic reticulum: |
smooth ER that stores calcium |
|
|
Sarcomere: |
functional unit for contractions |
|
|
Myofilaments |
actin and myosin (motor protein) |
|
|
Skeletal Muscle |
Attaches to and covers the bony skeleton
Contracts rapidly but fatigues easily
Responsible for overall body motility
Controlled at neuromuscular junctions |
|
|
Smooth Muscle |
Found in the walls of hollow visceral organs (ex. stomach), upper airways, and arteries
Forces food and other substances through body channels
Relaxation opens airways (constricted in asthma)
Constriction in arteries increases blood pressure |
|
|
Cardiac Muscle |
Connected by intercalated disks
Does not fatigue
Contains much greater concentration of mitochondria |
|
|
Myofilament |
macromolecular structure (smallest unit of muscle) |
|
|
Sarcomere |
composed of several myofilaments (contractile unit of the muscle) |
|
|
Myofibril |
Composed of bundles of myofilaments with sarcomeres at both ends |
|
|
How do muscles contract? |
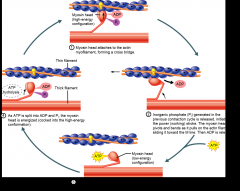
|
|
|
T tubulals |
release Ca2+ from the sarcoplasmic recticulum |
|
|
Neuromuscular Junction |
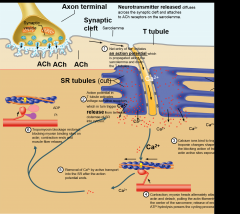
|
|
|
Glycolytic fibers |
Rely primarily on anaerobic respiration
Fatigue easily |
|
|
Oxidative fibers |
Rely primarily on aerobic respiration
Fatigue resistant |
|
|
innervation of smooth muscle
|
varacosities not nueromusclar junctions like skeletal muscle. The neurotransmitters/calmagulan are released into wide synaptic
|
|
|
The three membranes that surround muscle cells |
1) Endomysium covers the muscle fiber 2) Parimysium covers facicle 3) epimysium covers entire muscle |
|
|
Smooth muscles use Ca how? |
Calcium regulates contraction through calmodulin. Causing them to contract in a corkscrew fashion. |
|
|
Skeletal muscles use ca how?
|
Calcium ions bind to troponin; troponin changes shape, removing the blocking action of tropomyosin; actin active sites exposed.
|
|
|
Aerobic exercise results in an increase of |
Muscle capillaries Number of mitochondria Myoglobin synthesis |
|
|
Resistance exercise (typically anaerobic) results in: |
Muscle hypertrophy Increased mitochondria myofilaments glycogen stores |
|
|
The three parts of a neuromusclar junction |
Neuron axon: contains vesicles with the neurotransmitter acetylcholine (ACh)
Motor end plate of muscle: contains ACh receptors
Synaptic cleft: space separating the axonal ends from the muscle fiber |
|
|
facicle |
portion of muscle that is seperated by connective tissue |
|
|
enzyme cascade |
-sequence of successive activation reactions involvingenzymes |
|
|
eicosanoids |
-Lipid, signaling molecule
- |
|
|
glutathione |
-glutamate, cysteine and glycineOxidized and reduced forms -Most abundant intracellular antioxidant -Primary source is liver, but can made in most cells |
|
|
hyperplasia |
- the enlargement of an organ or tissue caused by an increase in the reproduction rate of its cells, often as an initial stage in the development of cancer. |
|
|
hypertrophy |
-enlargement or overgrowth of an organ or part due to increase in size of its constituent cells |
|
|
atrophy |
-waste away, typically due to the degeneration of cells, or become vestigial during evolution |
|
|
metaplasia |
-reversible replacement of one differentiated cell type with another mature differentiated cell type |
|
|
dysplasia |
-abnormality of development or an epithelial anomaly of growth and differentiation |
|
|
Liver damage following alcohol abuse |
- |
|
|
Why does the nervous system using electrical signalling? |
- Fastest way to communicate witht he rest of the body. |
|
|
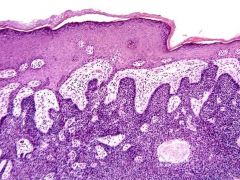
Why is our skin many layers thick? |
- Inorder to provide protection |
|
|
The effects of smoking and alcohol on cilia |
- Drinking alcohol slows cilia down. - smoking thickens mucous, and paralyzes cilia - together smoking and drinking have an additive effect on the moco-ciliary elevator |
|
|
The effects of prenatal Vitamin A overexposure and their relevance to the chemical structure of Vitamin A |
- Lipophilic, builds up in fat |
|
|
The difference between a tumor promoter and tumor initiator |
- Promoter=causes rapid cell growth - Initiator = damages or binds to DNA |
|
|
How the skin is repaired following injury |
-Platelets release clotting factors -Positive feedback leads to more platelets plugging the leak -Blood flow is stopped - The blood clot is replaced with granulation tissue -Blood supply restoredRegeneration and fibrosis -Surface epithelium regenerates -Scab detaches |
|
|
The key differences between healthy cells and metastatic cancer cells |
-Uncontrolled cell division -Cells ignore checkpoints in cell cycleFrequent errors in DNA replication -Tumor suppressors and proto-oncogenes often mutated (p53, BRCA1, BRCA2, Rb) -No limit on number of cell divisions -No requirement to adhere (metastasis) |
|
|
Key interactions in the body’s antioxidant response system |
- |
|
|
The need for multiple types of transport across cell membranes and multiple connections between cells |
- |
|
|
The effects of caffeine and epinephrine and their interplay with second messenger systems |
- |
|
|
Benign dermal tumors |
- |
|
|
malignant dermal tumors |
- |
|
|
Melanoma |
- |
|
|
Squamous cell carcinoma |
-Thin epidermus, intolerance to cold due to less dermal fat, and skin becomes dry and itchy - UV radiation increases skin aging |
|
|
Basal cell carcinoma |
- red itchy skin caused by bacteria |
|
|
identify the underlying cause of Tinea/ringworm/jock itch/athlete’s foot |
- Fungus |
|
|
identify the underlying cause of Impetigo |
- UV radiation and genetics |
|
|
identify the underlying cause of Tinea/ringworm/jock itch/athlete’s foot |
- Skin |
|
|
identify the underlying cause of Skin cancer |
- linings of mostly endodermal origin, covered in epithelium, which are involved in absorption and secretion. They line cavities that are exposed to the external environment and internal organs. |
|
|
cutaneous |
-serous fluid or serosal fluid is used for various bodily fluids that are typically pale yellow and transparent, and of a benign nature, that fill the inside of body cavities. |
|
|
mucous |
- secrete their essential product by way of a duct to some environment external to itself |
|
|
serous |
- directly into the blood rather than through a duct |
|
|
Exocrine Gland |
- one cell layer |
|
|
Endocrine Gland |
- multi cell layer |
|
|
simple |
- thin cell layer |
|
|
stratified |
- Cubidial shaped |
|
|
squamous |
- height are at least four times their width |
|
|
How does a neuron’s structure mimic the function of the nervous system? |
- The cell soma comunicates with dendrites. like the brain with its nerves |
|
|
columnar |
- Alopecia: occurs when your immune system mistakenly attacks hair follicles
- male pattern baldness: Genetic |
|
|
Can you identify all major tissue types and specialized cells within each tissue type? (e.g. neurons v. glia, basal cells, keratinocytes, fibroblasts, 3 types of muscle cells, squamous, cuboidal and columnar epithelium |
- |
|
|
Where is glycogen stored and why? Why don’t we store all of our excess calories as glycogen? |
- In the liver and muscle cells, muscle need extra energy and the liver helps to maintain blood glucose homeostasis. - We need fat to insulate organs |
|
|
major sub-types of connective tissue and their common form (matrix + cells) and progenitor cell (mesenchymal stem cells). Why are blood, bone and adipose tissue considered connective tissue? |
- |
|
|
Know the three major types of muscle cells (skeletal, smooth and cardiac). How does each one’s unique cell shape/structure relate to its function? |
- |
|
|
begininng of exam 3 |
- |
|
|
Be able to identify the cranial nerve responsible for ptosis and the most common effects of head injuries on cranial nerve function. What is the prognosis for head injury patients? |
-Cranial nerve III: ocularmotor. Ptosis wierd closed eye thing. - Most commonly the cranial nerves damaged are the olfactory, facial, and the three ocular nerves ( III, IV, VI) |
|
|
What do olfactory and gustatory receptors have in common? How are they different? |
-Olfactory receptors are plentiful and sense thousands of chemicals.
- Gustatory receptors sense five diferent chemical stimuli
- Both are chemo-receptors |
|
|
For hearing, understand how sound waves generate forces that are received and transduced from the outer ear to the inner ear. What are the two types of hearing loss and what are some common causes of hearing loss? How do other structures in the ear affect balance and orientation? |
-hair cells in Perilymph in the Cochlea are vibrated by the oval window being vibrated by the stapes which is ultimately vibrated by the external auditory meatus
-Conduction hearing loss: ostoscterosis => aging => hearing aid
- Sensory Neural hearing loss: genetic loss of hair cells in inner cells => cholerear implant but can't fully impart hearing |
|
|
Know the difference between rods and cones, how our vision system adapts to light/dark and long v. short distance vision. What happens during aging? What are some common disorders of the vision system? Ex.) presbyopia, myopia, color blindness and macular degeneration. |
-Rods: Respond to dim light (as little as one photon) Night vision Up to 100 rods converge on a single ganglion cell Image is fuzzy and not distinct
-Cones: Require bright light for activation High-acuity color vision (1 cone 1 ganglion cell) Found in the macula lutea
- Disorders: Macular degeneration cells in the macula thin and breakdown. |
|
|
Eyes in the dark |

|
|
|
For each sensory system covered (vision, hearing, taste and smell), know the major anatomical structures and specialized receptor cell types (e.g. mechanoreceptors, chemoreceptors, etc.). |
- |
|
|
Understand the difference between cholingergic and adrenergic receptors. |
-Cholinergic: Binds Acetal choline (nictonic or muscorinic receptors) : generally inhibitor.
- Adrinergic (norepininphic binder) alpha recepto stimlatory beta receptor inhibitory
|
|
|
What is “referred pain?” Why should we care? What is the difference between a visceral reflex and a somatic reflex? What are examples of each? How do reflexes change during development? |
-Why does your left arm hurt when you’re having a heart attack? Pain stimuli from the viscera are perceived as somatic in origin Why? visceral pain afferents travel along the same pathways as somatic pain fibers |
|
|
How do the sympathetic and parasympathetic divisions antagonize each other? When do they cooperate? What are the “D” and “E” roles? When does the parasympathetic system INCREASE activity in a target organ? Why does the parasympathetic have short-lived, localized control while the sympathetic has longer-lived, more diffuse control? |
-Ex.) Digestion Sympathetic fibers inhibit digestion and elimination Parasympathetic fibers facilitate digestion, defecation and urination Ex.) Respiration and Circulation Sympathetic fibers increase heart and respiratory rates Parasympathetic fibers decrease heart and respiratory rates. Parasympathetic division Short-lived, highly localized control Why? Acetylcholine is rapidly degraded Sympathetic division Long-lasting, diffuse effects Diffuse neuronal connections Norepinephrine takes longer to inactivate Norepinephrine and epinephrine are released into the bloodstream |
|
|
Understand the basic functions of the CNS v. the PNS, the afferent v. efferent pathways, and the autonomic (sympathetic v. parasympathetic) and somatic nervous system divisions. What are the anatomical and physiological (functional) differences? What are the targets for the sympathetic v parasympathetic? Neurotransmitters? |
- CNS: Primarily conciously controled actions - PNS: |
|
|
Know the basic structure of a nerve, how nerve fibers regenerate and when they can’t regenerate. |
- |
|
|
How is the spinal cord organized? Where is the gray v. white matter? How is the organization/protection similar to the brain? What is the hierarchy of motor control? Why are lumbar punctures done below L3? Why is the epidural space a good location for anesthesia? |
-Spinal chord is organized the same way as the brain duramater, archnoid mater, pia mater, surrounded in cerebral spinal fluid and covered in bone. - hierachry of motor control
-Below L3 the spinal chord proper ends
- Epidural space is good for injections, because you do not puncture its protection and you allow for the drug t difuss into the spinal chord
|
|
|
Understand the basics of sleep (NREM v. REM) and the effects of sleep deprivation. Which is associated with dreaming? Nightmares? |
- |
|
|
How do the limbic system and reticular activating system function? What are the major types of memory? How do motor memory and fact memory differ? Short-term v. long-term memory? How are different brain regions and neurotransmitters involved? |
- |
|
|
Know the mapping of functional divisions (i.e. primary motor cortex, Broca’s area, Wernicke’s area, premotor and primary somatosensory regions). What are their major functions? How are they coordinated? |
- |
|
|
Understand the importance of folic acid in embryonic brain development and how a deficiency can lead to neural tube defects. |
- |
|
|
Be able to identify the function/basic location (telencephalon, diencephalon, brain stem) of each of the following: thalamus, hypothalamus, pineal gland, hippocampus, amygdala, corpus striatum, medulla oblongata, cerebellum, pons, corpus callosum, midbrain, superior colliculi, inferior colliculi, and prefrontal cortex. |
- |
|
|
What are the major types of neurotransmitters? What are two major roles for dopamine? acetylcholine? How are glutamate and GABA connected? What is the link between serotonin and mood? |
- |
|
|
Understand the difference between voltage-gated ion channels and chemically gated channels? Where are they found? How do they function? Where do neurotransmitters bind? |
- |
|
|
Understand how myelin sheaths are formed, their importance andthe differences in the CNS and PNS. What is “node-jumping?” What does that have to do with impulse speed? What else affects the speed of neuronal impulses? |
- |
|
|
Know exactly what is happening at each point in the graph as anaction potential is generated. Know where the absolute and relativerefractory periods are and what that means in terms of generating thenext action potential. Keywords: Na+, K+, threshold, depolarization, repolarization, hyperpolarization. How do excitatory and inhibitory neurotransmitters change the picture? What is spatial v. temporal summation?
|
- |
|
|
Understand the major parts of a neuron, their basic structure and function, how a neuron functions to transmit electrical signals and release neurotransmitters. |
- |
|
|
Know the six major neuroglial cells found in the nervous system, their basic functions, and whether they’re found in the central nervous system (CNS) or peripheral nervous system (PNS). |
- |
|
|
You should also be able to recognize the classic pathology for Alzheimer’s, Parkinson’s and Huntington’s diseases as well as multiple sclerosis and ALS. |
- |
|
|
MS |
-Multiple sclerosis (MS) is a disease in which your immune system attacks the protective sheath (myelin) that covers your nerves. Myelin damage disrupts communication between your brain and the rest of your body. Ultimately, the nerves themselves may deteriorate, a process that's currently irreversible. Signs and symptoms vary widely, depending on the amount of damage and which nerves are affected. Some people with severe MS may lose the ability to walk independently or at all, while others experience long periods of remission during which they develop no new symptoms. There's no cure for multiple sclerosis. However, treatments can help speed recovery from attacks, modify the course of the disease and manage symptoms. Age. MS can occur at any age, but most commonly affects people between the ages of 15 and 60. Sex. Women are about twice as likely as men are to develop MS. Family history. If one of your parents or siblings has had MS, you are at higher risk of developing the disease. Certain infections. A variety of viruses have been linked to MS, including Epstein-Barr, the virus that causes infectious mononucleosis. Race. White people, particularly those of Northern European descent, are at highest risk of developing MS. People of Asian, African or Native American descent have the lowest risk. Climate. MS is far more common in countries with temperate climates, including southern Canada, northern United States, New Zealand, southeastern Australia and Europe. Certain autoimmune diseases. You have a slightly higher risk of developing MS if you have thyroid disease, type 1 diabetes or inflammatory bowel disease. Smoking. Smokers who experience an initial event of symptoms that may signal MS are more likely than nonsmokers to develop a second event that confirms relapsing-remitting MS. |
|
|
Basal cell carcinoma |
|
|
Squamous Cell Carcinoma |
|
|
Eyes in the light |

|
|
|
Know at least ONE drug/toxin that affects each receptor class and their effects (are they agonists or antagonists?). See Ch.14 PowerPoint table. |
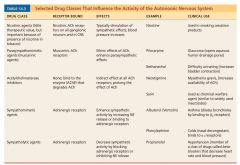
|

