![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
75 Cards in this Set
- Front
- Back
|
What is the primary function of the respiratory system? |
gas exchange between air and circulating blood |
|
|
What is the secondary function of the respiratory system? |
acid-case balance (by regulating CO₂ in the blood) |
|
|
The respiratory system consists of ___ and ___ zones |
conducting and respiratory zones |
|
|
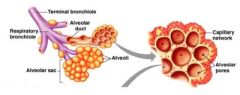
conducting zone |
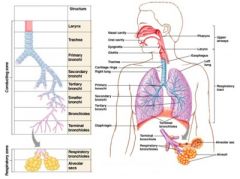
from nasal cavity to terminal bronchioles "dead space" |
|
|
respiratory zone |
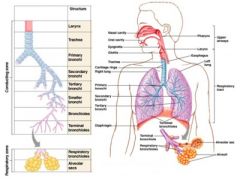
respiratory bronchioles and alveoli |
|
|
respiratory muscles |
diaphragm and other muscle that promote ventilation |
|
|
ANS regulates smooth muscle to control _____ diameter |
ANS regulates smooth muscle to control bronchiole diameter |
|
|
bronchodilation |
controlled by SNS → reduces resistance |
|
|
bronchoconstriction |
controlled by PNS and histamine release (allergies) → increases resistance |
|
|
What is alveoli? |
air-filled pockets within lungs where gas exchange takes place |
|
|
Alveoli are patrolled by _____ _____ (dust cells) - phagocytize microbes |
alveolar macrophages |
|
What are Type 1 cells? |
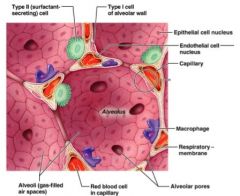
thin, delicate endothelial cells |
|
What are Type 2 cells? |
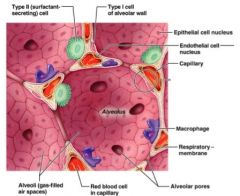
produce surfactant (oily secretion - coats epithelium & reduce surface tension) |
|
|
Surface tension |
caused by attraction of H₂O molecules to each other (collapses alveoli) (premature babies - immature Type 2 cells = little/no surfactant) |
|
|
Pulmonary capillaries |
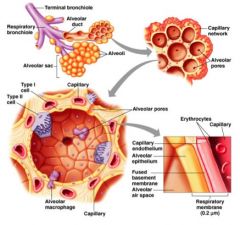
exchange CO₂ and O₂ with alveoli |
|
|
Respiratory Membrane |
thin membrane of alveoli where gas exchange takes place (air-blood interface) |
|
|
What are the three layers that gases must diffuse across? |
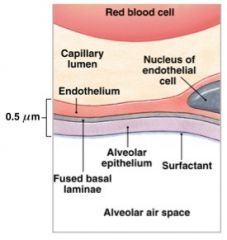
1. Type 1 alveolar cells |
|
|
Blood supply to the lungs: pulmonary circuit |
purpose is gas exchange (also nourishes respiratory membrane) |
|
|
Blood supply to the lungs: systemic circuit |
purpose is to nourish lung tissue |
|
|
Each lung is located within a double-layers _____ membrane |
serous |
|
|
Visceral pleura |
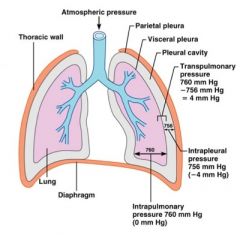
lines outer lung surface |
|
|
Parietal pleura |
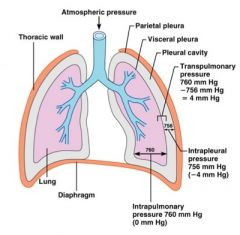
lines inner surface of thoracic wall |
|
|
Thoracic wall: |
• floor - diaphragm |
|
|
The right and left pleural cavities are separated by the _____ |
mediastinum |
|
|
Each pleural cavity holds a long and lungs function ____ |
independently |
|
|
pleural cavity |
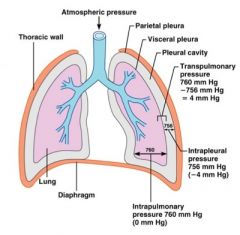
holds serous fluid that reduces friction as lungs inflate/deflate |
|
|
What are the two principles affecting air movement? |
atmospheric pressure and Boyle's Law |
|
|
Atmospheric Pressure |
(Patm) ~ weight of the Earth's atmosphere (on our bodies and everything around us) |
|
|
Respiratory Pressure |
is describe relative to Patm |
|
|
Boyle's Law |
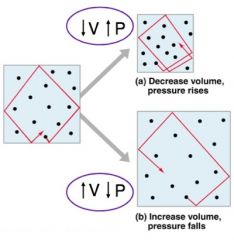
defines the relationship between gas pressure and volume |
|
|
Respiratory cycle |
1 inspiration (inhalation) + 1 expiration (exhalation) |
|
|
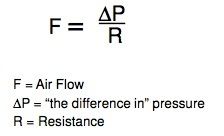
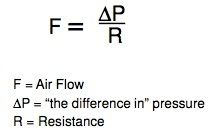
Mechanics of Breathing |
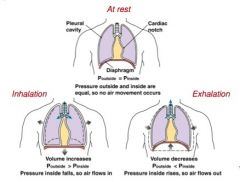
based on pressure differences (△P) between air in lungs and atmosphere during on Respiratory Cycle |
|
|
What is the normal atmosphere pressure? |
1 atm at sea level = 760 mm Hg |
|
|
intra-alveolar pressure (Palv) |
pressure of the lungs (within alveoli) |
|
|
During relaxed breathing .... |
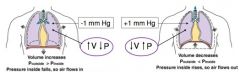
inhalation = −1 mm Hg inside lungs |
|
|
At rest ("Quiet" inspiration/expiration) the most important muscles are: |
diaphragm and external intracostal muscles of the ribs |
|
|
accessory respiratory muscles → |
activated only when respiration increases significantly ("forced" inspiration/exhalation) |
|
|
Quiet inspiration |
diaphragm and external intercostal muscles (inspiratory muscles) contract and the rib cages rises |
|
|
Quiet expiration |
inspiratory muscles relax and the rib cage descends due to gravity |
|
|
What are some physical properties of the lungs? |
elasticity, compliance, and airway resistance |
|
|
What is elasticity? |
stretching force |
|
|
What is compliance? |
ease of expansion |
|
|
What is airway resistance? |
depends of diameter of lungs |
|
|
Respiratory system adapts to changing oxygen demands by varying: |
• number of breaths per minute (respiratory rate) ( |
|
|
respiratory rate |
number of breaths per minute |
|
|
tidal volume |
volume of air moved per breath (Vt) |
|
|
Respiratory Minute Volume |
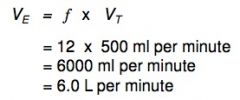
(VE) - amount of air moved per minute calculated by: |
|
|
Anatomical Dead Space |
volume of air that doesn't reach alveoli (air remaining in conducting passages - trachea, mouth, etc) |
|
|
Alveolar Dead Space |
if alveoli cease in gas exchange (e.g. damage or lined with mucus) |
|
|
Total Dead Space |
(Vd) = Anatomical Dead Space + Alveolar Dead Space |
|
|
Alveolar Ventilation (VA) |
amount of air reaching alveoli each minute |
|
|
Measurements of airflow: Respiratory volumes |
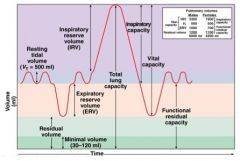
TV = volume of one breath |
|
|
Measurements of airflow: Respiratory volumes |
IRV = volume inhaled with maximum effort in excess of tidal volume |
|
|
Measurements of airflow: Respiratory volumes |
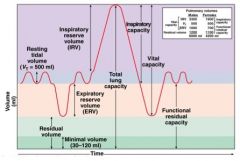
ERV = volume exhaled with max. effort in excess of tidal volume |
|
|
Measurements of airflow: Respiratory volumes |
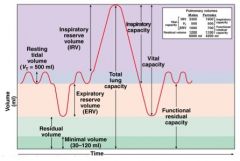
RV = volume remaining in lungs after max. expiration (keeps alveoli inflated) |
|
|
Measurements of airflow: Respiratory capacities |
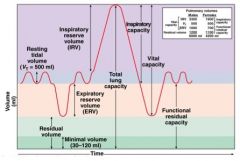
VC = volume exhaled with maximum effort after maximum inspiration |
|
|
Measurements of airflow: Respiratory capacities |
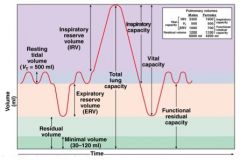
IC = volume of air inhaled after normal tidal expiration |
|
|
Functional residual capacity |
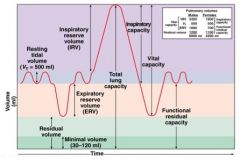
Functional residual capacity = volume in lungs after normal tidal expiration |
|
|
Total lung capacity |
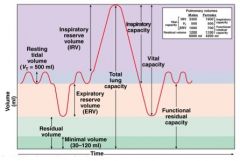
Total lung capacity = maximum volume lungs can contain |
|
|
VC = |
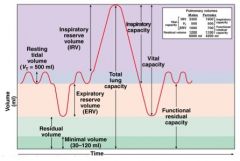
ERV + TV + IRV |
|
|
IC = |
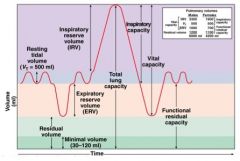
TV + IRV |
|
|
Functional residual capacity = |
ERV + RV |
|
|
Total lung capacity = |
VC + RV |
|
|
Pulmonary function tests |
used to asses one's respiratory status (compared with "normal" values) |
|
|
spirometer |
instrument used to measure different volumes of breathed air (water is displaced by the breathed air, and the volume can be recorded) |
|
|
Obstructive disorder |
difficult to get air out of the lungs (expiration) |
|
|
Restrictive disorder |
difficult to get air into the lungs (inhalation) |
|
|
Gas exchange occurs between air in ____ & ____ |
alveoli & blood → across respiratory membrane |
|
|
Gases are exchange by diffusion in response to a ____ ____ |
concentration gradient |
|
|
To understand how gases are exchanged between air in alveoli & blood you will need to consider: |
1. Partial pressure of gases (Dalton's Law) |
|
|
Dalton's Law of Partial Pressure (PP) |
• Total pressure (of gas mixture) = sum of individual gas pressures... called the partial pressures |
|
|
If you have a container with 4 gases: |
CO₂ = 400 mm Hg |
|
|
Henry's Law of Dissolves Gases |
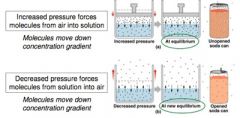
• When the mixture of gases is in contact with a liquid, each gas will dissolve in the liquid in proportion to its partial pressure |
|
|
Forced Exhalation includes respiratory accessory muscles such as: |
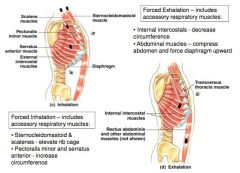
internal intercostals and abdominal muscles |
|
|
Force Inhalation includes accessory accessory respiratory muscles such as: |
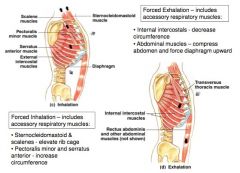
Sternocleidomastoid & scalenes and Pectoralis minor and serratus anterior |

