![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
|
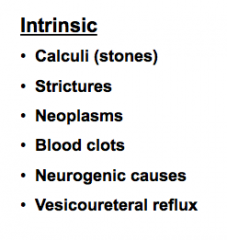
What are some intrinsic causes of ureter obstruction? |
|
|
|
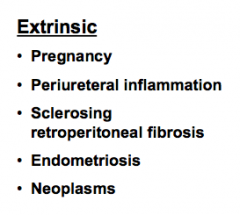
What are some extrinsic causes of obstructive lesions of the ureter? |
|
|
|
The overall result of ureter obstruction is what?
What occur if this is a long-standing process? |
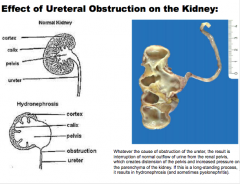
Interruption of normal outflow => distention of the pelvis => increased pressure on parenchyma (hydonephrosis if longstanding, sometimes pyelonephritis) |
|
|
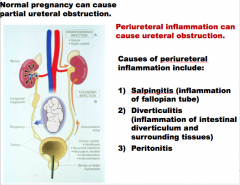
Can normal pregnancy cause partial ureteral obstruction? Can periuretal inflammation cause ureteral obstruction?
What are some causes of periureteral inflammation? |
|
|
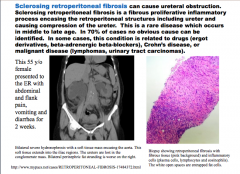
Can sclerosing retroperitoneal fibrosis cause ureteral obstruction? What type of inflammatory disorder is this? What does it encase? What age does this occur? Is an obvious cause often identified? What are some drugs, one disease, and malignancies that can cause it? |
|
|
|
What are some possible presenting symptoms for sclerosing retroperitoneal fibrosis? |
Abdominal and flank pain Vomiting and diarrhea 2 weeks duration |
|
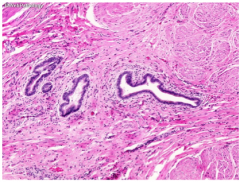
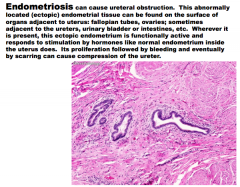
What is shown here? Can it cause ureteral obstruction? Where can it be found?
Does it respond to hormonal stimulation?
What causes compression of the ureter? |
|
|
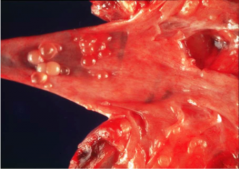
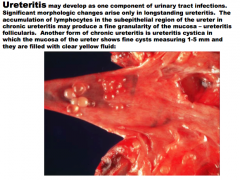
What may develop as one component of urinary tract infections? Timeframe? Pathogenesis? What is the name for the chronic presentation of this? What will you see? (shown here) |
Result of UTIs |
|
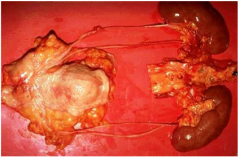
Congenital anomalies of the ureters are found in what percent of all autopsies?
What are double ureters usually accompanied by? |
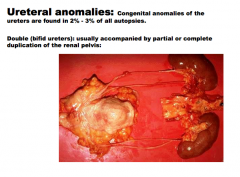
Usually don't cause any kind of morbidities. |
|
|
Ureteral anomalies:
Ureteropelvic junction obstruction:
Usually presents in infants or _____, more common in ____, more commonly on the ____. Abnormal organization of and/or excess ______ deposition of ______ between _____ muscle bundles. Results in ________.
|
Ureteral anomalies: Ureteropelvic junction obstruction: Usually presents in infants or children, more common in boys, more commonly on the left. Abnormal organization of and/or excess stromal deposition of collagen between smooth muscle bundles. Results in hydronephrosis.
|
|
|
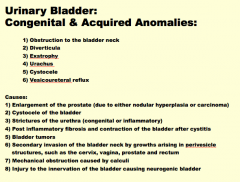
What are some congenital and acquired anomalies of urinary bladder? |
1) Obstruction to the bladder neck |
|
|
Causes: URINARY BLADDER CONGENITAL AND ACQUIRED ANOMALIES
|
|
|
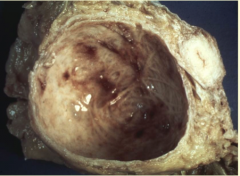
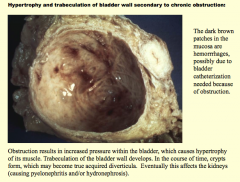
What is shown here?
What are the dark brown patches in the mucosa due to?
What is the pathway from obstruction => crypts and kidney damage? |
|
|
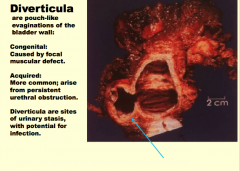
What are diverticula?
What are the congenital ones caused by?
What do acquired ones arise from?
Why are they do they have the potential for infection? |
|
|

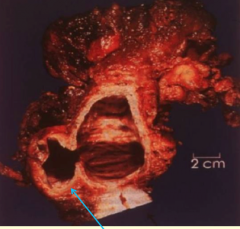
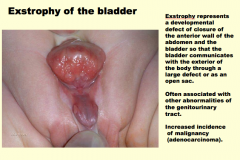
What is this?
Exstrophy represents the ______ tract. Increased incidence of ________ |
|
|
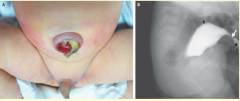
What is shown here?
5-6 cm vestigial structure located between the _____ of the bladder and the ______. In the embryo, this connected the bladder to the ______. Rarely the urachus may remain patent in part or in whole (______ urachus). When it is totally patent, a fistulous urinary tract is created that connects the ______ with the umbilicus. More often the umbilical end or the bladder end remains ________, while the central region is obliterated. In this case a sequestered umbilical epithelial rest or bladder _______ is formed that may provide a site for the development of ______. At other times only the central region of the _______ persists, giving rise to urachal _______. ________ arise in such cysts. These account for only 0.1%-0.3% of all ______ cancers, but 20%-40% of bladder _________. |
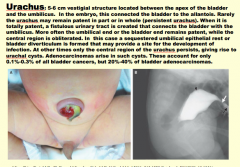
If you see a cancer in the bladder that is called adenocarcinoma => most likely to arise in the apex of the bladder! |
|

What is a cystocele? What is it caused by? |
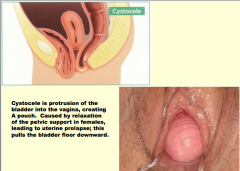
|
|
|
What vesicoureteral reflux?
The ureters enter the bladder in an ______(angled) course, terminating in slit-like orifice. The ______ of this _____ segment (“intramural” means located within the wall) of the ureteral orifice permits the enclosing bladder musculature to act like a ______ valve, blocking the upward reflux of urine even in the presence of marked _____ of the urinary bladder. |
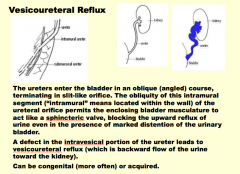
This is pretty common. 1 in a few hundred births.
Between 2 month and two years = first febrile bladder infection, go and look for vesicoureteral reflux |
|
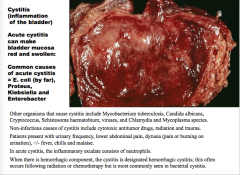
What is this? What can make the bladder mucosa red and swollen?
What organisms are common causes?
Non-infectionous causes?
How will the patient present?
What does the inflammatory exudate consist of predominantly? |
|
|
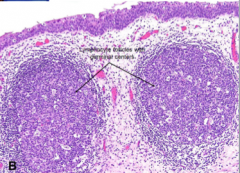
What cells will you see in chronic cystitis?
Where may lymphocytes form within? What is this called?
What is the most common situation? |
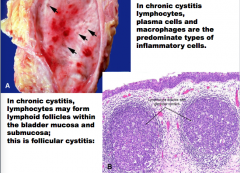
Older gentleman with a little BPH = static urine causes infection!
pathologyforurologist website |
|
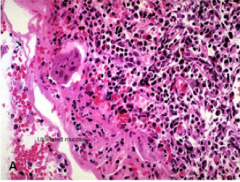
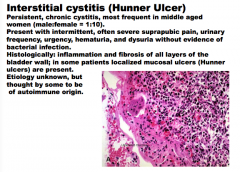
What is this? How is it most common in?
How will the patient present?
What does the histology show? In what layers of the bladder wall? What ulcers MAY be present in some patients? What is the suspected etiology? |
|
|
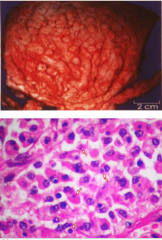
What is shown? This disease most likely represents a defective host response to what?
What cell types will be present?
What will the macrophages contain?
What is the name for laminated mineralized concretions within and between macrophages? |
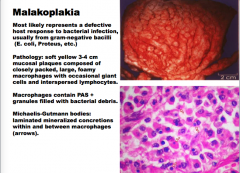
If you had this in the kidney, and the doctors all agree its cancer, do transplant. If bladder, new bladder. Really a benign disorder and don't need to do these things. |
|
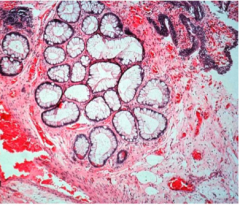
What is this?
Chronic cystitis can cause nests of _________ (Brunn nests) to grow downward into the ________, where they may undergo glandular ________ (termed cystitis glandularis) or retract to produce cystic spaces lined by flattened ________(cystitis cystica), with 0.1-1 cm cysts, filled with clear fluid. Cystitis glandularis |
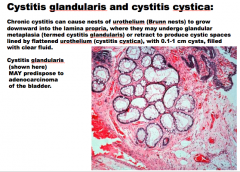
ASSOCIATED with adenocarcinoma of the bladder. |
|
|
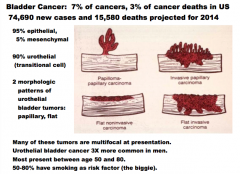
How common is bladder cancer? Where is 95% located (epithelial or mesenchymal)? Where is 5% located? What percent is urothelial (transition cell)?
What are the two morphologic patterns of urothelial bladder tumors?
Man of the tumors are ______ at presentation. What sex is it more common in? Ages? What is the biggest risk factor? |
|
|
|
What are the four types of carcinoma of the bladder? |

|
|
|
Bladder cancer:
[1] ______-of-function mutations in _____ are found predominantly in______ carcinomas and result in constitutive activation of the _____receptor tyrosine kinase.
|
Bladder cancer:
[1] Gain-of-function mutations in FGFR3 are found predominantly in noninvasive low-grade papillary carcinomas and result in constitutive activation of the FGFR3 receptor tyrosine kinase.
|
|
|
[3] Activating mutations in the ______ oncogene are frequent, particularly in _____-grade, noninvasive tumors.
[4] HRAS and ______ mutations are generally mutually exclusive in bladder cancer. |
[3] Activating mutations in the HRAS oncogene are frequent, particularly in low-grade, noninvasive tumors.
[4] HRAS and FGFR3 mutations are generally mutually exclusive in bladder cancer. |
|
|
30% to 60% of ______ carcinomas have losses of genetic material on chromosome ___, which are often the only chromosomal changes present in superficial ______ ______ tumors and occasionally in noninvasive _______ tumors, suggesting that these are early events in the evolution of bladder carcinomas. |
30% to 60% of bladder carcinomas have losses of genetic material on chromosome 9, which are often the only chromosomal changes present in superficial noninvasive papillary tumors and occasionally in noninvasive flat tumors, suggesting that these are early events in the evolution of bladder carcinomas. |
|
|
The Ps and Qs of Chromosome 9 Losses Early in Bladder Carcinogenesis
The deletions on _____ of bladder carcinomas span a region that includes the tumor suppressor gene ______, which encodes the cyclin-dependent kinase inhibitor p16/INK4a, and _____(a protein that augments _____ function) [1].
|
The Ps and Qs of Chromosome 9 Losses Early in Bladder Carcinogenesis
The deletions on 9p of bladder carcinomas span a region that includes the tumor suppressor gene CDKN2A, which encodes the cyclin-dependent kinase inhibitor p16/INK4a, and ARF (a protein that augments p53 function) [1].
|
|
|
What is the two pathway model of bladder carcinogenesis?
First pathway: FGFR3 and ______ mutations and chromosome ___ deletions cause ___-grade superficial papillary tumors. Of these, a minority may then lose TP53 and/or _____ function and progress to invasion.
Second more aggressive pathway, _____ mutations initiate noninvasive ___-grade flat or papillary lesions and then loss of chromosome ___ and acquisition of other, still to be characterized mutations, causes progression to invasion. |
First pathway: FGFR3 and RAS mutations and chromosome 9 deletions cause low-grade superficial papillary tumors. Of these, a minority may then lose TP53 and/or RB function and progress to invasion.
Second more aggressive pathway, TP53 mutations initiate noninvasive high-grade flat or papillary lesions and then loss of chromosome 9 and acquisition of other, still to be characterized mutations, causes progression to invasion. |
|
|
What is the classic presentation of urothelial bladder carcinoma?
What are some other symptoms?
What can you see on cytologic examination of urine? What procedure can be performed for the biopsy? |
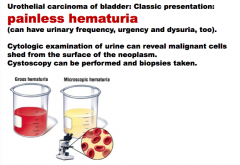
Hematuria may not be something you can see grossly. |
|

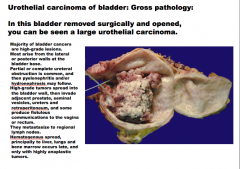
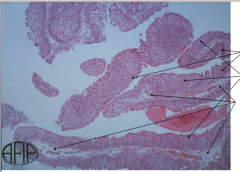
What is shown in this bladder?
Majority of bladder cancers are ___-grade lesions. Most arise from the ____ or _____ walls at the bladder base. Partial or complete ureteral _____ is common, and then ______ and/or |
|
|
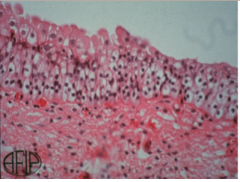
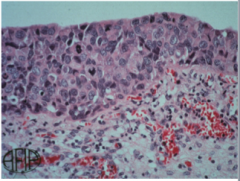
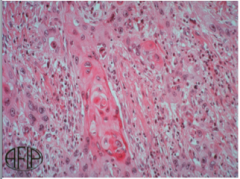
What is this? |
Normal bladder urothelium (above):
Anything much thicker or thinner than this is usually dysplasia |
|
What is this? |
Urothelial (transitional cell) carcinoma in situ (below): pleomorphic cells with pleomorphic hyperchromatic nuclei, prominent nucleoi and numerous mitotic figures. |
|
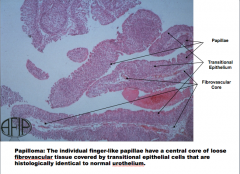
Identify the papillae, transitional epithelium, and fibrovascular core. What do the individual finger-like papillae have a central core of? Covered by what? |
|
|
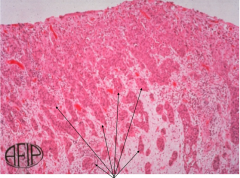
What is this? What do nests of malignant cells within the lamina propria represent? |
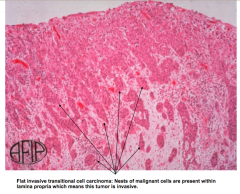
|
|
|
Treatment of Urothelial Carcinoma of Bladder:
“The selection of treatment for bladder cancer depends on the grade, ______, and whether the lesion is ____ or papillary.
For small, localized low-grade papillary tumors, the diagnostic _______ resection is the only surgical procedure done. Patients are followed with cystoscopy and _____ cytology for the rest of their lives to detect _______.
Patients at high risk of recurrence and/or progression (CIS; papillary tumors that are high grade, multifocal, have a history of recurrence, or are associated with lamina propria invasion) receive intravesical instillation of an attenuated strain of ___________ called bacillus Calmette-Guérin (BCG). The bacteria elicit a local _______ reaction that destroys the tumor.
Metastatic bladder cancer responds to ________, but is not curable with current agents.”
|
|
|
|
Tumor _____ determines more of the prognosis of urothelial carcinomas than most other types of carcinoma. ***
Patients have a high tendency to develop what after excision? What will recurrences exhibit in terms of grade (higher or lower)? The higher the grade of the tumor, the _____ the chance of recurrence.
What is the 10 year survival rate of urothelial carcinoma (TCC) Grade 1? What about Grade III? |
|
|
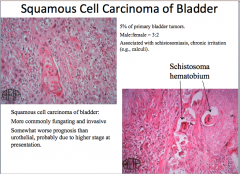
What is this? (we are in the bladder)
More commonly fungating and ______.
Somewhat _____ prognosis than urothelial, probably due to ______ stage at presentation.
What other two diseases is it associated with?
What percent of primary bladder tumors? Males or females? |
|
|
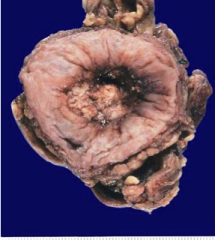
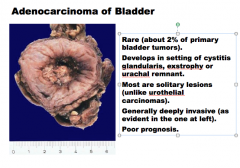
What is this? Are they rare?
Develops in the setting of what three things?
Most are what type of lesion (single or multiple)? Are they usually deeply invasive?
Good or bad prognosis? |
|
|
|
What are the four benign mesenchymal tumors that may arise in the bladder? All are RARE. |
Leiomyoma (most common of benign) Hemangioma Granular cell tumor Neurofibroma |
|
|
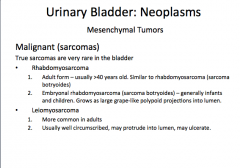
Malignant Mesenchymal Tumors: (also very rare)
What are the two major types?
Which are more common in adults? Which is just infants and children?
Which are well circumscribed, may protrude into lumen, and may ulcerate? |
|
|
What is this? |
Embryonal rhabdomyosarcoma (sarcoma botryoides = grape clusters) |
|
|
Urethritis:
Two common designations
Which one do E. Coli, Chlamydia, and Mycoplasma cause?
Urethritis is one component of what syndrome? Other two?
What can be a cause of urinary outflow obstruction with subsequent involvement of the urinary bladder, ureters, and kidneys? |
|
|
|
What is an inflammatory lesion presenting as a small, red, painful, friable mass about the external urethral meatus in the female patient?
What age is it found at?
How does it present histologically? |
|
|
|
Where do papillomas usually occur? What is their origin usually?
In what age and sex does carcinoma of the uretha occur? Where does it usually arise? What type of carcinoma usually? Are they usually more or less aggressive than bladder cancers? |
|
|

What is happening here? What does it result from? Which type is more common? What does it interfere with? |
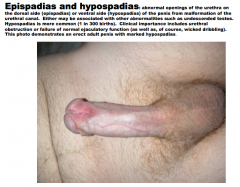
|
|
|
Phimosis: inability to easily retract the ______ can be from congenital malformation or _____ disease; it leads to the accumulation of secretions and ______ under the prepuce, associated with ______. In circumcised or uncircumcised adults, _______ (glans inflammation is balanitis; foreskin inflammation is posthitis) is most commonly related to ________. This photo demonstrates a child’s phimotic penis with associated inflammation; note the tight hooding of the glans and the ______ of the foreskin (which leads to _______ and even tighter hooding). |
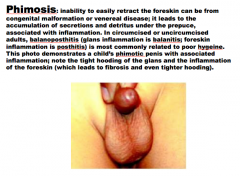
|
|
|
Syphilis and gonorrhea |
|

Condyloma acuminata: “warty,” _______ like growths which occur primarily in the _______ region. They are venereally transmitted and most often caused by HPV types ___ or ___. They are not _____, but tend to recur despite vigorous therapy. |
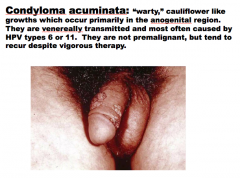
|
|
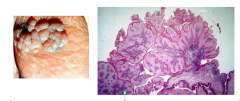
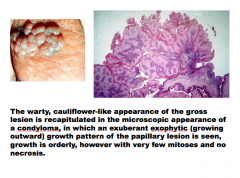
The warty, cauliflower-like appearance of the gross lesion is recapitulated in the microscopic appearance of a ______, in which an exuberant exophytic (growing outward) growth pattern of the ____ lesion is seen, growth is ______, however with very few mitoses and no necrosis. |
|
|
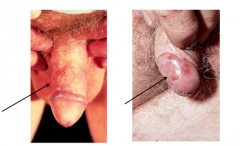
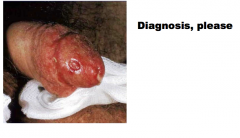
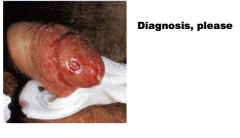
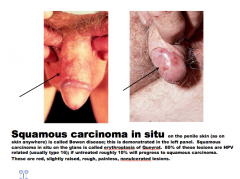
What is shown here?
On the penile skin (as on skin anywhere) is called _____ disease; this is demonstrated in the left panel. ______ carcinoma in situ on the glans is called ______ of Queyrat. 80% of these lesions are ____ related (usually type ___); if untreated roughly 10% will progress to ______ carcinoma. |
|
|
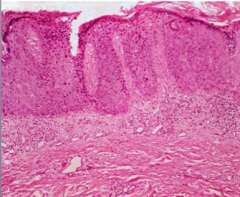
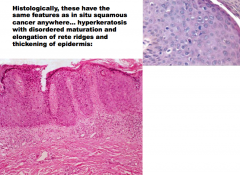
What features does squamous carcinoma of penis share with in situ carcinomas anywhere? |
|
|

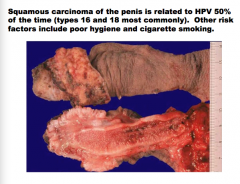
What is related to HPV 50% of the time? Which types most commonly? Two other risk factors? |
|
|
|
|

