![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
53 Cards in this Set
- Front
- Back
|
Pediatric Vital Signs - Rough Guide for BP and HR |
• HR = 150 – (5 x age in years)
• BP = < 70 mmHg + (child’s agein years X 2) mmHg (1-10 years) |
|
|
Pediatric Altered Mental State - GHOST |
· Glucose
· Headtrauma · O2deficiency/overdose · Shock/seizures · Temperature |
|
|
Pediatric - Extra Hx Questions |
• Ask medication use in breast feeding mother
• Question parents/patient (asage appropriate) to: – Signs and symptoms – Prodromal illness, recentviral infections, abdominal pain – Immunisation history – General health – Recent weight gain/loss – Compliance with medications,if any. – In infants – ask about nappiesin particular: • Have they been normal inappearance • Have they been as “wet” asnormal. • Colour of urine. |
|
|
Syncope - More serious etiologies in Children - Investigate and be cautious w/ |
o Evidence of injury especially head trauma. o Continuing altered mental state - especially if unconscious for > 5 minutes
o Recurrent episodes o History of cardiac conditions/surgery - associated chest pain or palpations o Significant persistent abnormalities in vital signs. o Thesyncopal episode was exercise related or occurred in the recumbent position o Afamily history of sudden death, deafnessor cardiac disease (QT syndrom) |
|
|
Febrile Convulsions |
o Usuallybetween 6 months to 6 years
§ Make sure no evidence of intracranialinfection, abnormality and toxins or endotoxins – if present, not febrileconvulsion o Feverthought to lower seizure threshold |
|
|
Status Epilepticus - Standard Definition |
Seizures persisting or recurring without a return to consciousness for anextended period, usually 30 minutes
|
|
|
Status Epilepticus - Issue with Standard Definition |
Most suggest that after 5 minutes the chance of the seizureself-resolving is limited and at .5 minutes neuronal injury can occur
|
|
|
Status Epilepticus - Operational Definition |
Generalized, convulsive status epilepticus inadults and older children (>5 years old) refers to ≥ 5 minutes of either continuous seizures or 2 or more discrete seizures between which there is incomplete recovery of consciousness
|
|
|
Prolonged Convulsion - Risks |
o Injury
o Acidosis& other electrolyte imbalanceso Hypoxia/hypercarbia o Hypoglycaemia o Hyperthermia o Permanentneuronal injury o Cardiovascularcollapse o Longerit lasts the more difficult to control o Increasesmorbidity and mortality |
|
|
DKA |
BGL11-15 mmol/L with ketonesusually seen in type 1 diabetics
|
|
|
DKA Features |
o Dehydration(sometimes not apparent)
o Acidosis o Electrolyteimbalances o Kausmallsrespirations Does not usually cause hypotension on its own |
|
|
DKA - Most common precipitating factors in children |
Ignorance and new onset diabetes followed byinfection – also six I’s
|
|
|
DKA - 6 Is |
o Infection
o Infarction(brain) o Ignorance o Ischemia(AMI) o Intoxication o Implantation(conditions of pregnancy) |
|
|
DKA - Initial and Definitive Treatment |
- Fluid therapy if initiated first - Definitive treatment is insulin therapy |
|
|
DKA - Insulin after Flfuis Justification |
o Insulincan lead to vascular collapse secondary to rapid shift of fluid intointracellular space. Should not be initiated until the blood pressure isstabilized.
o Hypokalemicpts should not receive insulin until K+ has been administered – could worsenhypokalemia |
|
|
DKA - Cerebral Edema |
- <1% patients - 40-90% mortality - Poorly understood mechanism associated with - Hypoxia - Osmotically driven movement of water into CNS when plasma osmolality declines too rapidly during treatment of DKA with aggressive fluid therapy (careful) - Usually 4-12 hours after treatment
|
|
|
Inborn Errors of Metabolism (IEM) |
o Hereditarydisorders involves gene mutations, usually of a single enzyme or transportsystem, cause significant blocks in metabolic pathways and accumulation ordeficiency of a particular metabolite
o Permanentneurologic sequelae o Previously normal neonate with acute clinicaldeterioration o Vomiting,neurologic abnormalities, metabolic acidosis and hypoglycaemia |
|
|
Pediatric Chest Pain - Life Threatening |
Rarely unless serious physical findings are present or pt has significant problems in medical history |
|
|
Pediatric Chest Pain - Myocarditis |
Oftenpreceded by viral respiratory illness.
Presentswith: § Respiratory distress § Fever § Tachypnea § Tachycardia § Generalized malaise § ECG may show widespread ST segment changes |
|
|
PE - Adolescence - Risk Factors |
· Recent abortion
· Using birth control pill · Recent long bone fractures, surgery orperiods of immobility |
|
|
Kawasaki Disease |
Inflammation of blood vessels (including coronary blood vessels and may cause saccular dilations - aneurysms) |
|
|
Kawasaki Disease - Main Risk |
Anuerysms can be come obstructer by a thrombas - risk of infart or embolisation |
|
|
Kawasaki Disease - Features |
· Conjunctivitis
· Mucousitis (Strawberry tongue and fissured lips) · Persist fever exceeding 39.5°C not very responsive to normal treatment · Rash · Lymph node enlargement · Spindle-shaped swelling of the digits followed by desquamation |
|
|
Marfan Syndrome |
Abnormality of connective tissue causing weakened blood vessels and dilation of the aorta |
|
|
Marfan Syndrome - Risks Factors |
Usually effects tall, thin childre with long arms and fingers - may have visual disturbances |
|
|
Marfan Syndrom - Risk |
- Aortic dissection - Aortic rupture |
|
|
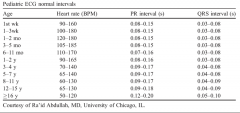
Pediatric ECG Intervals |
|
|
|
Pediatric - Bradyarythmias - Cause and Indication |
o o Mostcauses associated with hypoxia and acidosis o Indicatespre-arrest |
|
|
Primary Causes (rare) - Pediatric Bradyarthymias |
- Sick Sinus Syndrome - AV block |
|
|
Secondary Cause - Pediatric Bradyarthmias |
Midline sternal scar indicates dysrythmia is secondary to congental heart disease - may have implanted pacemaker Congenital heart defects may contribute to AV blocks (rare) |
|
|
Pediatric Tachycardias - Congenital Heart Disease - Most common rythm presentations |
o Atrialflutter
o Atrialfibrillation |
|
|
Pediatric Sinus Tachycardia |
o Childrenaugment cardiac output by increasing HR rather than SV
o HRincreases early, hypotension late o Forevery 1 degree Celsius increase in body temperature, HR increases 9.6 BPM –consider underlying process rather than intrinsic cardiac issue |
|
|
SVT - Types |
- AV reentrant tachycardia – WPW
- AV nodal or junctional tachycardia,cyclical reentrant pattern - Ectopic atrial tachycardia, is rare and ismanifested by rapid firing of a single ectopic focus in atrium |
|
|
SVT - Mx |
o Toleratedinitially – CHF and cardiogenic shock
o Valsalva o Icetowel on faceICP cardioversion |
|
|
Assystole |
Most common arrest rythm - usually associated with hypoxia |
|
|
Vfib/VT - Arrest Considerations |
- Reversible causes - A history of either congenital heartdisease or a precipitating event, such ashyperkalaemia (renal failure), hypomagnesaemia, or commotio cordis. - Respiratory failure leading to severehypoxemia, particularly in older children or adolescents suffering anexacerbation of chronic pulmonary disease, such as asthma. - Less commonly may occur with certain typesof drug overdose (tricyclic antidepressants; beta-agonists in asthmaticchildren), - Electrocution - Re-entry tachycardias includingWolff-Parkinson-White syndrome |
|
|
PEA - Arrest Considerations |
Tension pneumothorax, cardiac tamponade, severehypovolemia, severe acidosis, hypoxia, hypothermia or hypoglycemia
|
|
|
Long QT Syndrome |
Long QT interval secondary to imaired ion channels in the myocardiuam - Due to multiple genetic mutations leading to dysfunction of potassium, sodium and calcium channels - Overabundance of cations within myocardium - Risk of arrhythmias like torsades de pointes |
|
|
Long QT Syndrome - Common Presentation |
- Typically in late childhood and adolscence - Syncope with exercise or stress |
|
|
Long QT Syndrome - Inherited (Congenital forms) |
o Anautosomal recessive trait (Jervell and Lange-Nielsen syndrome) that isassociated with deafness
o Asautosomal dominant (Romano-Ward syndrome). |
|
|
Long Q Syndrome - Aquired forms |
- Myocarditis
- Mitralvalve prolapse - Electrolyte abnormalities - Drug induced |
|
|
Commotio Cordis |
o Life threatening dysrhythmia caused by a direct non-penetrating injury
o VF typical but also heart block, VT, BBB, ST-T wave abnormalities andasystole can occur |
|
|
Pediatric - Heart Failure |
Rare and usually due to structual disease |
|
|
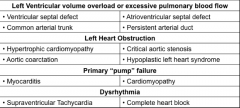
Pediatric Heart Failure- Structual heart disease |
|
|
|
Pediatric Heart Failure - Features |
o Breathlessness
o Cyanosis o Signs of cardiogenic shock o Failure to thrive o Refusal to feed o Persistent irritability o Poor toleration of respiratory illnesses o Crackles/heart murmurs |
|
|
Duct-dependent Congenital Heart Diseases |
– Pulmonary atresia – Critical pulmonary valvestenosis – Tricuspid atresia – Severe Tetralogy of Fallot – Transposition of the GreatVessels – Hypoplastic left heartsyndrome – Critical aortic stenosis |
|
|
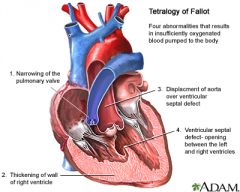
Tetralogy of Fallot |
o Most common cause of right-to-left shunt
o Pulmonary stenosis o Overriding aorta (enlarged and appears to arise from both left and rightventricles instead of left ventricle, as occurs in normal hearts) o Ventricular septal defect o Right ventricle hypertrophy |
|
|
Tetralogy of Fallot - Diagram |
|
|
|
Hypercyanotic Attacks (Tet Spells) - Definition and Immediate Tx |
– Patients with Tetralogy of Fallot havespells where they suddenly turn a blue color due to a low oxygen in theirbloodstream.
– When the patient has decreased blood flow throughthe lungs due to elevated resistance in the pulmonary blood vessels. – This is due to much of the blood goesdirectly from the right heart (less oxygenated) to the left heart through thedefects such as the Ventricular Septal Defect and the overriding aorta. – Immediate treatment includes puttingpatient in the lateral position with knees to chest or squatting. |
|
|
High Flow O2 in Neonatal Resucitation |
· High oxygen and lung-stretching lead to increased ROS (reactive oxygenspecies) production and expression of pro-inflammatory cytokines · Vaginal flora in lungs also predisposes to inflammation - can lead to chronic lung disease · Resuscitation of preterm neonates with 30% oxygen causes less oxidativestress, inflammation, need for oxygen, and risk of bronchopulmonary dysplasia. · No optimal O2 found yet |
|
|
Barriers to Pain Releif - Pediatrics |
- Historical beleif infants don't feel pain - No data existed on short and long-term effects of analgesics on children - Age-appropriate pain assessment tools lef physicians unable to conceptualise and quantify subjective pain experienced by children (FLACC or Wrong Backer) - Fear of adverse events persists - Parents believe the role of the hospital - Fear of inducing addiction - Childs fear of receiving injections |
|
|
Neonatal Resuscitation - Other points |
· Placenta performs respiratory, excretory, andendocrine functions during fetal life. As the cord is clamped, the neonate hasto rapidly adapt and perform all of the above functions.
· Breathing inhibited during parturition - severe asphyxia can inducegasping movements, resulting in aspiration of meconium during delivery. · Continuous breathing is triggered at birth by sensory stimulation suchas cooling, rising PCO2, removal of placental humoral inhibitory factors(possibly prostaglandins), catecholamine surge, and oxygen · Expansion of the alveoli leads to release of surfactant with lowered surfacetension. · During subsequent expiration, high positive pressures are createdpresumably by breathing against a closed glottis. This aids in clearing ofliquid in the lungs and a more uniform distribution of air throughout the lungand establishment of functional residual capacity · Primary apnoea – don’t treat with assisted ventilations – secondaryapnoea – treat quickly with assisted ventilation and or oxygen · Primary apnoea usually followed by 4-5 minutes of gasping · PEEP useful in alveolar expansion · Do APGAR at 1 and 5 minutes - Assessment of colour and respiration every 30 seconds · Auscultation more reliable than umbilicus palpation for pulse rate · Umbilical venous catheter · 10 ml/kg fluids in case of persistent hypotension – consider hypovolemia · Naloxone in respiratory depression and maternal narcotic use in last 4hours |
|
|
Inconsolability |
In children 3-6 months generally distinguishes aggitation from serious pain |

