![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
36 Cards in this Set
- Front
- Back
|
ALS - Pediatric Chain of Survival |
1. Preventionof injury or arrest 2. Earlyand effective CPR 3. EarlyEMS activation 4. EarlyALS |
|
|
Pediatric Airway Features |
· Obligate nasal breather when <6 months o Easilyblocked in URT infections · 3-8 y.o. – adenotonsillar hypertrophy cancontribute to obstruction and can make inserting airway adjuncts difficult · Flexed in supine position – head large · Large tongue · High anterior larynx · Reduction in airway diameter results insignificant loss of cross-sectional area o Resistanceincreases 16 fold – can double this in turbulent flow (crying) |
|
|
Pediatric OPA Consideration |
o Due tolarge tongue and possible trauma of turning OPA – may be necessary to usealternative method o Considerations: § Proper sizing § Proper positioning § Too large – epiglottis becomes obstruction § Too small – may bush tongue into hypopharynx |
|
|
Pediatric - Breathing Features |
· Increased RR - Infants diaphragmaticbreathers – muscles tire faster
· Increased metabolism and O2 consumption - 4ml/kgin adult, 6-8ml/kg in pediatric · Decreased functional residual capacity andalveoli:surface area- more prone to hypoxia · Increased chest wall compliance - prominentsternal recession and rib movement when compliance decreases or in airwayobstruction· Decreased alveolar recoil - Intrathoracicpressure less negative |
|
|
Pediatric - Signs of Respiratory Distress |
o Tachypnea
o Increasedrespiratory effort o Grunting– small airway or alveolar collapse (pneumonia, CHF, ARDs, pulmonary contusiono Stridor– sign of extrathoracic obstruction (inspiration)- foreign body, upper airwayobstruction, infection o Wheezing– Intrathoracic lower airway obstruction (bronchitis and asthma) o Abdominalbreathing or seesawing o Headbobbing – neonates - accessory sternomastoid muscle use |
|
|
Pediatric - Circulation Features |
· Stroke volume in infants is relativelyfixed (until 2 y.o.)
· Circulating volume per kilogram high butactual quantity low – small blood loss critical importance · Maintain good SVR to maintain BP –decompensate rapidly · Brachial pulse preferred site in infant (orapex of heart) · Blood pressure:o Hypotensiondefined (1-10 y.o.) - <70mmHg+ (childsage in years x 2) o <3y.o. – Rely on central pulse such as carotid · Cap refill in palms or soles of feet – agood indication of perfusion status |
|
|
Pediatric - Other Assessment Issues |
· Cranial sutures not fully fused until 1.5-2years
· Sunken frontanelle – dehydration/fluid loss· Tense fontanelle - ? Increased intracranialpressure · Cervical spine injuries can occur withoutbony damage SCIWORA · Due to chest compliance – potentialsignificant underlying chest issues without rib fractures · Low protection for abdominal organs |
|
|
Pediatric- Neonate Approximate Vital Signs |
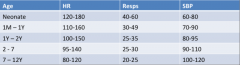
|
|
|
Pediatric GCS |

|
|
|
Approach to Neonates - Up to 1 month |
• Likes to be held and kept warm • Avoid loud noises, bright lights • May be soothed if allowed to suckle • Warm your stethoscope and hands before touching infant |
|
|
Neonate Characteristics - Up to 1 month |
• Normally alert, looking around • Focuses well on faces • Flexed extremities |
|
|
Approach to Neonates - Up to 3 months |
• Likes to be held by parents • Place older infants in sitting position • Examine from toes to head • Have parent remove clothing 1 item at a time, then replace • Distractwith a toy or penlight • Speak continuously in soft tones • Performpainful procedures last |
|
|
Neonate Characteristics - Up to 3 months |
• Normally alert • Eyes follow examiner • Slightly flexed extremities Can sit unaided by 6 to 8 months. |
|
|
Approach to Toddlers - 1-3 years |
• Speak to child and parent before physical contact • Engender child’s trust by gaining parent’s cooperation • Allow child to be held by parent • Examine from toes to head • Speak continuously in soft tones • Allow parent to help with examination • Respect modesty • Avoid discussing future events - hide wounds, needles and scissors |
|
|
Characteristics Toddlers - 1-3 years |
• Normally alert, active • Can walk by 18 months • Does not like to sit still • May grab at penlight or push hand away |
|
|
Approach to Children - 3-6 years |
• Explain actions using simple language
• Engender child’s trust by gaining parent’s cooperation • Respect modesty • Allowchild to handle equipment • Make a game of assessment • Tell child what will happen next - hide wounds, praise good behaviour and tell child just before procedure if it will hurt |
|
|
Chracteristics - 3-6 y.o. |
• Normally alert, active • Cansit still on request • Can cooperate with examination • Understands speech • Will make up own explanations for anything not understood
|
|
|
Approach to Children - 6-12 years |
• Let child make treatment choices when possible
• Make acontract with child to encourage cooperation • Reassure the child • Respect modesty • Give praise for cooperation |
|
|
Approach to Children - 12-18 years |
• Speak directly to patient
• Obtain history from patient • Explainthe process as to an adult • Interviewprivately when appropriate • Be honest; encourage question • When possible, reassure patient regarding disfiguring injury • Respect modesty • Ask friends to comfort patient when needed |
|
|
Characteristics - 12- 18 years |
• Has clear concepts of future • Responds positively to attitude of respect • Can make decisions about care |
|
|
Pediatric Assessment Triangle - Components |
APPEARANCE CIRCULATION WORK OF BREATHING |
|
|
Pediatric Assessment Triangle - Appearance |
TICLS - Tone - Interactiveness - Look/gaze - Speach/cry |
|
|
Pediatric Assessment Triangle - Circulation |
- Pallor - Mottling - Cyanosis |
|
|
Pediatric Assessment Triangle - Work of Breathing |
- Abnormal sounds - Abnormal positioning - Abnormal retractions - Nasal flaring |
|
|
Pediatric Resuscitation - Classifications |
· Newborn - Firstminutes to hours of life
· Neonate-Lessthan 28 days · Infant-28days to 1 year · Small child-1-8years · Older child -9-12years |
|
|
Pediatric Resuscitation - IPPV |
· 12-20 breaths/min
· In newborns consider IPPV at 40-60/min · Avoid applying pressure on neck structures· Initially to increase functional residualcapacity |
|
|
Pediatric Rescucitation - CPR |
• 2 breathes to 15 compressions for paediatrics/Infants.
• In infant - if inadequately perfused and pulse < 60 - begin CPR • In children - if inadequately perfused and pulse < 40 - begin CPR • ETT – 12 to 14 ventilations/min with continuous cardiac compressions • 1 breath to 3 compressions for newborns immediately after birth • If inadequately perfused and pulse < 60 after 30/60 of IPPV - begin CPR • LMA where can't ventilate, can't intubate – considerable before intubationalso |
|
|
Defibrilation - Up to 8 years |
DCCS at 4 J/Kg Round up to the next highest setting on defibrillator |
|
|
Pediatric Cardiac Arrest - Asphyxial Arrest and Cardiac Pathways |
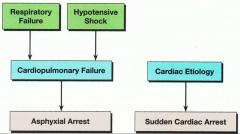
|
|
|
Pediatric Tempurature Control |
· Thermo-regulatorycontrols are under-developed
o Problemswith maintaining temperature control o <2months old infants generally cannot shiver · Significantamount of heat can be lost via head · Preventhypothermia |
|
|
Pediatric Arrest - Adrenaline |
– Use of IV Adrenaline by ACPs in paediatric cardiac arrest
• Use the 1:10000 strength • To make a 1:10000 strength dilute 1 mg (1:1000) ampoule with 9 mls ofnormal saline.• Still 1 mg (1000mcg) of adrenaline• Therefore each 0.1 ml of a 1:10000 strength of adrenaline will be 10mcgs. |
|
|
IO Injection Site |
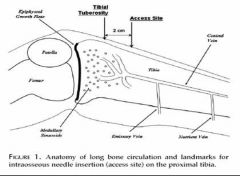
|
|
|
Apparent Life Threatening Events (ALTE) - Usually in infants - Characteristics |
– Apnoea (respiratory pause > 15 seconds)
– Decreased mental status – Colour change (pallor or cyanosis) – Alteration in muscle tone (rigidity or limpness) – Choking and – Usually required some degree of stimulation or resuscitation to resolveabove symptoms. Can be isolated or caused by life-threatening condition - should be investigated - usually no treatment required No relationship with SIDS established |
|
|
SIDS - Population |
• Usually in <1 year age group, peaks around 2-4 months
|
|
|
SIDS |
Unexplained death, usually during sleep, of a seemingly healthy baby less than a year old.
|
|
|
SIDS - Risk Factos |
- Overheating - Bead sharing - Mother <20 and unmarried mother - Short interpregnancy interval - Inadequate parental care - Lower socioeconomic status - Illness during pregnancy - Congenital defects - Neonatal respiratory abnormalities or viral illness - Previous ALTE - Sleeping position - Low APGAR score, birth weight, NICU admission - Male sex - Preterm birth - Mother use of addictive drugs - Low education levels |

