![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
25 Cards in this Set
- Front
- Back
|
bacteria invade _________ & ______________ where they survive & replicate hence termed ________________ pathogens |
bacteria invade monocytes & macrophages where they survive & replicate hence termed intracellular pathogens |
|
|
intracellular bacteria avoid/disrupt phagoctyosis |
Listeria monocytogenes - ruptures the early phagosome and escapes into cytosol Mycobacterium tuberculosis - blocking fusion of early phagosome with cell lysosomes get protection from extracellular immune system + Abs |
|
|
immune response to intracellular bacteria |
involves both CD4 Th1 cells = promote bacterial killing by infected phagocytes + CD8 T cells = directly kill infected cells |
|
|
T cell priming |
1. Immature DC get infected/take up antigen from intracellular bacteria 2. get activated via PRR/PAMP systems 3. migrate to local lymph nodes 4. mature into activated APC able to induce 1º CD4 + CD8 responses |
|
|
T cell priming activated DC cell specifics |
1. activated DC make MHCI + II and costimulatroy CD80/CD86/CD40 2. DCs release interleukins that promote activation and differentiation of IL-12; naïve CD4 → Th1 IL-18 naïve CD8 cells → CTL |
|
|
CLINCIAL APPLICATIONS genetic defect in IL-12/ IFN gamma |
defects in this pathway recurrent intracellular pathogen infections e.g. mycobacteria, salmonella typhi |
|
|
salmonellla type → which disease? |
typhoid fever |
|
|
Th1 cells |
After priming
1.pathogen specific Th1 goes back to infection site + interacts with MHCII/TcR 2.interaction with infected macrophages releases IFNgamma + TNFa α 3.these cytokines → macrophage activation → ↑ antimicrobial & antigen presenting capabilities 4.enhanced by CD40CD40L costimulation |
|
|
Monocyte/macrophage intracellular bacteria killing |
ROS Nitrogen intermediates (NO) lysosomal enzymes antimicrobial peptides IFN gamma signalling in infected cells overcomes pathogen induced block in phagosome maturation + consequently allows killing of bacteria in phagolysosomes |
|
|
Monocyte/macrophage intracellular bacteria killing diagram |

|
|
|
CTL cells |
on cognate MHC1/TcR interaction with infected cells primed CTL → cytotoxic granules |
|
|
CTL cytotoxic granules |
perforin - perforates target cell membrane by making a pore (similar to complement MAC) granzyme- degrades host cell proteins → apoptosis |
|
|
CTL cytotoxic granules: apoptotic pathways |
FAS/FASL binding Caspase enzyme system |
|
|
CTL cells: IFN gamma mediated macrophage activation by Th1 |
infection with TB 1.the cells still release metabolic + surface proteins 2.traffic to lysosome 3.degraded and resultant peptides loaded on MHC II 4.MHC II presentation to + recognition by Th1 |
|
|
CTL cells: Direct killing of infected cells by CTL |
infection with L monocytogenes 1. bacteria escapees into cytosol, from early phagosome, survives + replicates uses preforming toxin listeriolysin O 2. metabolic + surface proteins degraded by proteasome 3. transporter by TAP transporters into ER 4. loaded onto MHC I (as after viral infection) 5. MHC I deleted by specific CTL |
|
|
with both TB and Listeriosis... |
need both CD4 + CD8 T cells interact collaboratively |
|
|
in TB CTL also |
kills any infected cells which lack expression of MHC II e.g. pneumocytes fibroblasts epithelial cells |
|
|
DTH |
Delayed Type Hypersensitivity reaction n Type IV hypersensitivity memory T cell mediated (CD4 or CD8) response requires pre-sensitised host state ranges from mild → severe → fatal |
|
|
Mantoux test |
Dx TB 1.inoculate forearm intradermally with tuberculin 2. bacteria taken up by macrophages + immature DC 3. DC activated, guest lymph nodes 4. → strong memory T cell responses in TB infected patients 5. antigen specific Th1 migrate to forearm 6. inflammatory response occurs 7. 24-72 hours later visible inflammation 8. delay because Th1 cells → pro inflammatory cytokines + chemokine 9. consequent influx of monocytes + leukocytes this is a DTH response |
|
|
CLINICAL APPLICATION contact dermatitis |
due to DTH , Type IV hypersensitivity reactions
|
|
|
DTH diagram |
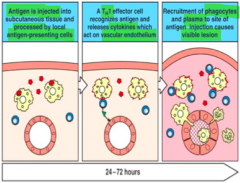
|
|
|
Granulomas what are they? |
form when DTH reaction to antigen which is foreign but unable to eliminate this final attempt to wall of chronic irritant/inflammation |
|
|
Granuloma classification |
infectious -presence of lymphocytes, in + surrounding macrophage mass CD4 cells try to activate cells CD8 cells try to kill cells -central cell necrosis non-infectious -sarcoidosis -granulomatosis -polyangiitis |
|
|
Granuloma formation cells |
interaction b/w macrophages + CD4 & CD8 T cells + inflammatory cells |
|
|
Granuloma formation diagram |
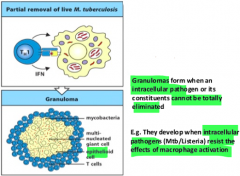
|

