![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
28 Cards in this Set
- Front
- Back
|
How is symphysis-fundal height (SFH) measured? What is normal at 12 wks? 20 wks? > 20 wks?
List 2 reasons for a smaller measurement than expected? List 2 reasons for a larger measurement than expected? |
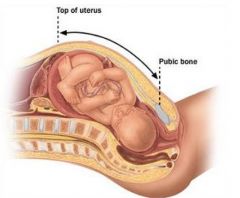
SPH: Distance over the abdominal wall from the top of the symphysis.
12 weeks: At Symphysis Pubis 20 weeks: At Umbilicus >20 weeks: Gestational age +/- 2 cm Smaller: 1) Wrong dates; 2) Small for gestational age; 3) Oligohydramnios; 4) Fetus in transverse lie Larger: 1) Wrong dates; 2) Molar Pregnancy; 3) Multiple Gestation; 4) Large for gestational age fetus; 5) Polyhydramnios; 6) Maternal obesity; 7) Maternal fibroid uterus. |
|
|
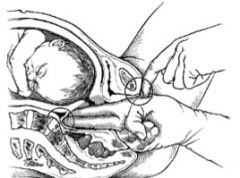
How are Leopold Maneuvers performed (4)?
|
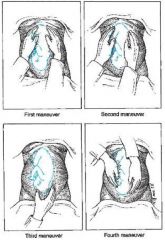
Leopold Maneuvers:
1)Identification of fetal pole at uterine fundus – breech (large, nodular) vs. head (hard, round, mobile) 2) Palms are placed on either side of the maternal abdomen to determine fetal back (firm, resistant) vs. fetal parts (small, irregular, mobile) 3) Use thumb & fingers to grasp presenting part just above symphysis pubis 4) Examiner faces mother’s feet and with the tips of the first 3 fingers of each hand exerts pressure in the direction of the axis of the pelvic inlet to determine position of presenting part. |
|
|
Describe fetal lie, presentation & position.
|
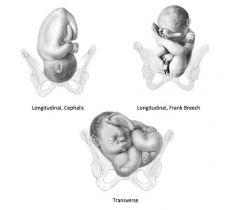
Lie – relationship of the long axis of the fetus to that of the
mother: Either 1) Longitudinal or 2) Transverse Presentation: – presenting part 1) Cephalic – fetal head (vertex, face or brow) or 2) Breech – buttocks (frank or complete) or footling Position – relationship of the presenting part to the maternal birth canal (i.e. distance down the canal) |
|
|
What are the four pelvic shapes?
Which has the best prognosis for a vaginal delivery? The worst? |
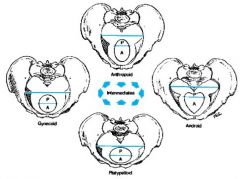
Four shapes: 1) Gynaecoid; 2) Anthropoid; 3) Android; 4) Platypelloid
Best Prognosis: Gynaecoid Worst: Android |
|
|
How is the diagonal conjugate measured?
|
Diagonal conjugate:
Distance from the sacral promontory to the lower margin of the symphysis pubis. Measured by: 1) Introducing 2 fingers in to the vagina and palpating the sacral promontory with the tip of the long finger 2)Then elevating the hand until it contacts the pubic arch 3)Mark adjacent point on the index finger 4)Withdraw hand and measure |
|
|
What is the obstetrical conjugate?
How is it estimated from the diagonal conjugate? |
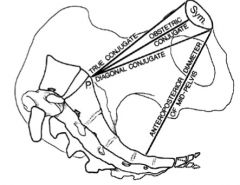
It is the Shortest anteroposterior diameter through which the fetal head must pass in descending through the pelvic inlet.
Subtract 1.5-2 cm from the diagonal conjugate to estimate the obstetrical conjugate. Diagonal conjugate > 11.5 cm is considered adequate for vaginal delivery of a normal-sized fetus |
|
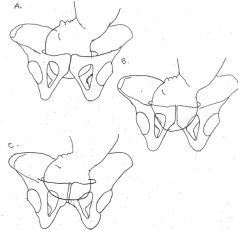
In which of these 3 diagrams is the vertex engaged?
|
B
Engagement is defined as reaching Station 0, at the Ischial Spine. You can see B has been drawn to have the vertex contacting the Ishial Spine. |
|
What is the station of the fetal head in this diagram?
|
Station 0.
Station is defined as the position of the presenting surface. Station 0 is at the Ischial Spine. |
|
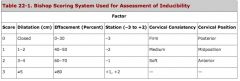
What is the Bishop Score of a mother whose cervix is 1 cm dilated, 30% effaced, of medium consistency, mid position and Station -2?
Is she ready for induction? |
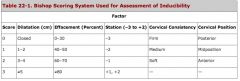
Dilation: 1
Effacement: 0 Consistency: 1 Position: 1 Station: 1 Bishop Score: 4 A score of 4 or less indicates an unfavourable cervix for induction. She'll need some "ripening." |
|

At term, which is the most common position of the fetal head as it enters the pelvis?
|
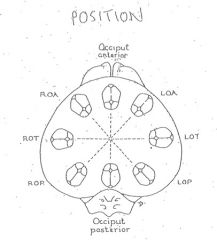
C
In full term pregnancy, the vertex usually enters the pelvic inlet in Occipital Transverse (OT) position. |
|
|
When a patient is pushing in the second stage of labour, what position of the fetal head is most likely to result in a normal spontaneous vaginal delivery?
|
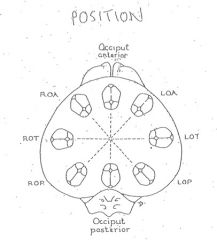
Occipital Anterior
|
|
|
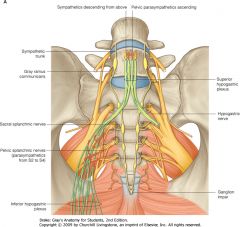
What nervous system and nerves control emission and ejaculation?
|
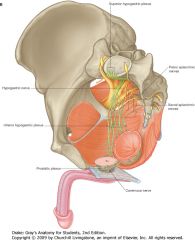
The efferent response for emission and the ejaculatory reflex involves the thoracolumber spinal ganglia (T12-L2) forming the hypogastric (sympathetic) nerve, which branches into preganglionic fibres at the prostate and seminal vesicles. Sympathetic stimulation results in closure of the bladder neck. The pudendal nerve (somatic) (S2-4) provides somatic nervous control to the external (striated) urinary sphincter and paraurethral striated sphincter.
|
|
|
Which muscles contract to propel seminal fluid?
|
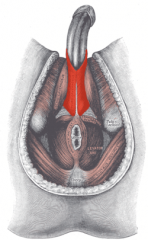
The bulbospongiosus muscles
|
|
|
Trace the path of sperm from the seminiferous tubules to the urinary meatus.
|
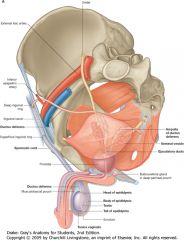
Seminiferous tubules (i.e. parenchyma of testes), rete testis, efferent ductules, epididymis, vas deferens, ejaculatory duct, prostatic urethra, penile urethra, urinary meatus
(Give it a trace in the picture) |
|
|
What structures may have been damaged during a retroperitoneal lymph node dissection that results in a patient not noting semen with ejaculation?
What might you see if you examined a urine specimen under the microscope shortly after he ejaculated? |
Injury to the sympathetic nerves (T12 – L2) will result in retrograde ejaculation. Lack of sympathetic stimulation results in the bladder neck remaining open during ejaculation, therefore, sperm may be indentified in the urine shortly after ejaculation.
|
|
|
Describe and identify the vascular supply of the corpora cavernosa.
|
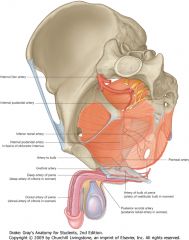
The internal pudendal artery branches into the deep artery of the penis to supply the corpora cavernosa (cavernous artery).
|
|
|
Trace the nerves responsible for erection from the spine to the corpora.
|
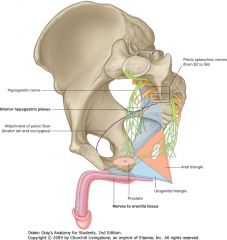
Afferent – The dorsal nerve of the penis from the pudendal nerve.
Efferent - The parasympathetic (pelvic splanchic nerves, S2-4, also known as the “pelvic nerve”). |
|
|
What kind of symptoms might be noticed with a bladder rupture? Define intra peritoneal and extra peritoneal bladder rupture and how to distinguish between the two.
|
A bladder rupture usually presents with hematuria (blood in the urine).
In addition there may be suprapubic or abdominal pain and an inability to void. Extraperitoneal bladder rupture usually results in urine leakage that is confined to the pelvis (i.e. below the peritoneal refection on the dome of the bladder). On a retrograde cystogram, this appears as a flame-shaped extravasation of contrast in the pelvis. Conversely, an intraperitoneal bladder rupture occurs where the peritoneum reflects over the bladder and results in urine leakage into the peritoneal cavity. On a retrograde cystogram, this is demonstrated by extravasation of contrast material that outlines the loops of bowel. |
|
|
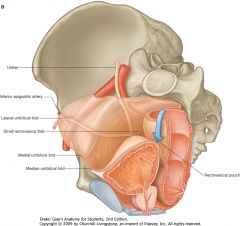
Define and identify the blood supply, venous drainage, and lymphatic drainage of the bladder.
|
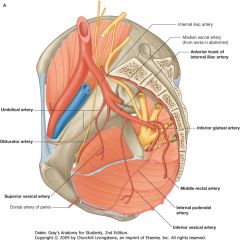
The bladder is supplied by the superior, middle and inferior vesical arteries, which arise from the anterior trunk of the internal iliac artery and by smaller branches from the obturator and inferior gluteal arteries. In females, the uterine and vaginal arteries also send branches to the bladder.
A rich plexus of veins surround the bladder which ultimately drain into the internal iliac (hypogastric) plexus. The lymphatics of the bladder drain into the vesical, external ilac, internal iliac, and common iliac lymph nodes. |
|
|
Identify the external urinary sphincter necessary for voluntary control of urination. What nerve supplies this sphincter?
|
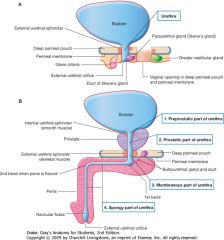
The pudendal nerve.
|
|
|
Identify the ligamentous support and muscles of the pelvis that are important in urinary continence.
|
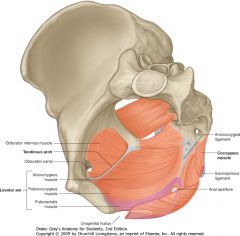
Note the: Endopelvic fascia, the urogenital diaphragm, levator ani
|
|
|
What is the trigone of the bladder?
|

The trigone refers to the triangular area of smooth urothelium that extends between the two ureteral orifices and the internal urethral meatus.
|
|
|
How does a normal (non-refluxing) ureter’s anatomy prevent vesico-ureteral reflux?
|

As the bladder fills and contracts, muscular tone of the trigone results in pulling on the intravesical ureter so that the ureter is occluded during periods of high intravesical pressure.
|
|
|
What is the vascular supply to the testicle?
|
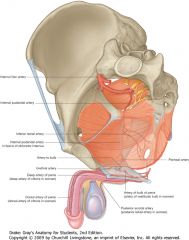
The testis has three arterial supplies: 1) internal spermatic testicular artery (primary supply- 90%), arises from the aorta; 2) deferential vasal artery (arises from the inferior vesical artery) ; and 3) external spermatic (aka cremaster) artery
|
|
|
When a man presents with testicular torsion, how long do you have to “save” the testicle?
|

Irreversible ischemic injury to the testicle may occur as soon as 4 hours after occlusion of the spermatic cord. Only 50% of men that have detorsion within 4 hours have a normal semen analysis. Therefore, any case of suspected torsion is a surgical emergency and requires immediate referral to urology (or general surgery if there is no local urology service).
|
|
|
If the testis had been ok on Doppler ultrasound what other scrotal structures could twist and cause pain?
|

The appendix testes (a mullerian/ paramesonephric duct remnant) and the appendix epididymis (a wolffian/mesonephric ducty remnant) may tort and cause localized scrotal pain and swelling that resolves spontaneously over a 4-5 day period with conservative management (rest, ice, and anti- inflammatories). It does not affect the vascular supply to the testicle.
|
|
|
What purpose does the pampiniform plexus of veins in th testes usually serve?
|
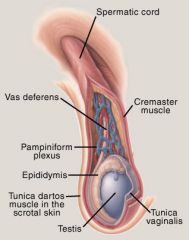
The pampiniform plexus not only drains blood from the testicle, it acts as a heat exchanger to regulate temperature. With a varicocele this ability may be lost and result in abnormal spermatogenesis.
|
|
|
How common is a varicocele? Does everyone with a varicocele experience infertility?
|
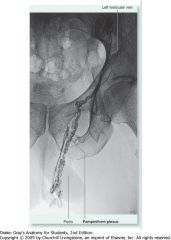
Varicoceles occur in 15% of men. Of men with infertility, 40% are noted to have a varicocele. Thus, not all men with a varicocele experience infertility. However, in some cases, a varicocele can result in sub-optimal semen analysis that can be improved by surgical repair of the varicocele.
|

