![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
60 Cards in this Set
- Front
- Back
|
Most medically important gram + cocci:
|
*Staphylococcus (catalase-positive)
-Staphylococcus aureus (coagulase-positive) -Other species (primarily coagulase-negative) *Streptococcus (catalase-negative) -Beta-hemolytic streptococci -Viridans (nonhemolytic and alpha hemolytic) streptococci and Streptococcus pneumoniae (alpha hemolytic) *Enterococcus (catalase-negative) -Enterococcus faecalis (typically nonhemolytic) -Enterococcus faecium (typically alpha hemolytic) |
|
|
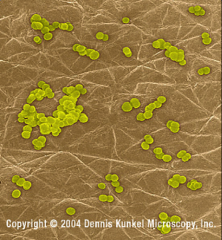
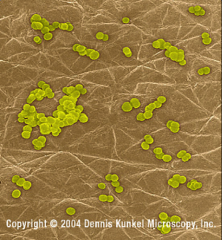
*Staphylococcus -- Gram+ cocci arranged in grape-like clusters
*Grapes of wrath, swiss-army knife; causes serious infections; has exotoxins. *Extremely resistant to antibiotics, especially ß-lactam antibiotics. *Ubiquitous. |
|
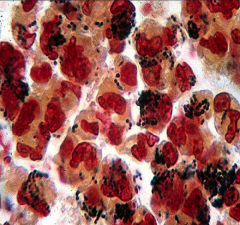
What is this?
General traits of this organism? |
*Staphylococcus aureus on the surface of human skin.
*All are ubiquitous *Major components of normal flora (skin, nose) *Important human pathogens *Significant host compromise is required for infection (cut, burn, etc.) *All are catalase positive!! *Nosocomial infections |
|
|
Summarize the kinds of staphylococci:
|
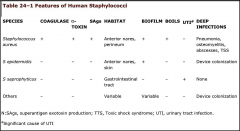
*Staph aureus is only one that is Coagulase positive.
*Staph aureus is most virulent. *Staph aureus has toxins. *Staph aureus can cause deep tissue infections. *Staph produces pus --> abscesses. *Epidermidis can colonize medical devices using its biofilm. *Saprophyticus associated with UTIs and young, sexually active women. |
|
|
*S. epidermidis: can form a viscous extracellular polysaccharide biofilm.
|
|
|
What test can you run to distinguish staph aureus from the other staph species?
|
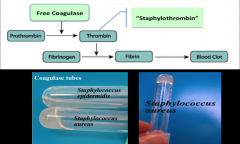
*Coagulase test: can be used to distinguish Staphylococcus aureus from other Staphylococcal species
*Aureus coagulates. |
|
|
What test can you run to distinguish staph from strep?
|
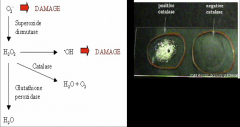
*Catalase test can be used to distinguish Staphylococcus from Streptococcus.
|
|
|
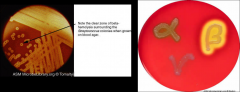
What aspects of staph aureus's fermentation allows for testing to differentiate it from other staph species?
|

*Staph aureus ferments Mannitol.
*Leads to a yellow color in the Mannitol salt agar. |
|
|
Key points about Staph aureus' structure:
|

*Bacterial colonies are white or golden (“aureus”) and hemolytic when grown on blood agar.
*Cell wall consists of a typical Gram-positive peptidoglycan. *A bit more teichoic acid than other gram positives. |
|
|
What diseases does staph aureus commonly cause?
|
*Abscess (hallmark)
*Food poisoning *Toxin-related diseases (like toxic shock syndrome) *Skin and wound infections |
|
|
What are common hospital and community-acquired infections that highlight staph aureus as an opportunistic pathogen?
|
*Pneumonia
*Osteomyelitis *Septic Arthritis *Bacteremia *Endocarditis *These infections occur nosicomially and out in the community. MRSA infection is a significant problem. Almost total ß-lactam resistance |
|
|
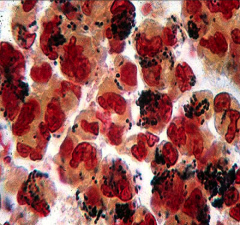
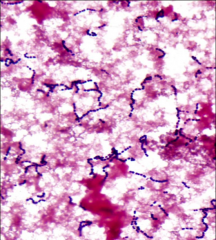
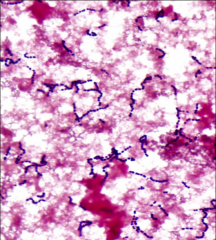
List all the gram + cocci:
|

|
|

|
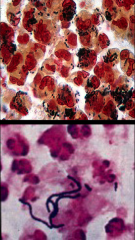
Top: Staph in clusters
Bottom: Strep in chains *Both gram + cocci. |
|
|
While on call on a Saturday night in July, you receive a call from the mother of a 15-year-old man who developed the acute onset of nausea, vomiting, and diarrhea shortly after returning from an outdoor party that was held at the home of a friend. At the party, a picnic lunch of hamburgers, hot dogs, potato salad, baked beans, and lemonade was served. The food was served on an outdoor picnic table, and the guests were free to eat at any time during the party. None of the food tasted spoiled or tainted. His symptoms started abruptly about an hour after he returned home, which was approximately 4 hours after he had eaten. He currently is unable to keep down anything. He does not have a fever and has not passed any blood in his stool or vomitus. Prior to calling you, your patient’s mother spoke with the hostess of the party, who said that she had heard from three other guests who became ill with similar symptoms.
What organism is the most likely cause of this patient's illness? Your patient's mother requests that you call in a prescription for an antibiotic to treat the infection. What is your response? |
*Staph aureus
-Loves to grow on carbs! (potatoes) *No antibiotic b/c the effects have been mediated by the toxin of the staph. The staph is likely already gone. |
|
|
Mr. C., a 37-year-old roofer, came to the emergency department with fever and a painful swelling on the left side of his neck. He had previously been healthy except for occasional boils. Three days before, he had noted a minor irritation around some whiskers. The lesion progressed to the size of a walnut, which prevented him from buttoning his shirt. Physical exam revealed a healthy man in mild distress. His temperature was 38.8°C. A 2- to 3-cm mass with a soft center was noted on his left anterior neck at the beard line, surrounded by erythema. Needle aspiration of the mass yielded about 1ml of pus that, under the microscope, showed large Gram-positive cocci in clusters and many neutrophils.
What was the source of the infection? What should be suspected if the infection fails to respond to b-lactam antibiotics? |
*Staph aureus.
-Abscess -Neutrophils attracted to abscess *Skin was the source. *If no response from ß-lactams, suspect MRSA. |
|
|
How does MRSA gain resistance?
|
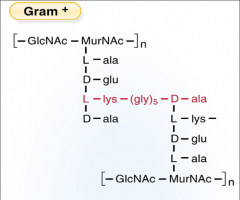
-Lysogenic transduction/conversion from bacteriophages (viruses that invade bacteria and pass on resistance).
-AA 3 (shown in red) in the CW (Penicillin-binding protein) gets altered. |
|
|
How does MRSA acquire new PBPs?
|

*MRSA strains produce new PBPs through acquisition of mecA gene.
*The new PBPs inhibit binding to ß-lactam antibiotics. |
|
|
Pathogenesis of S. aureus: Encounter and Entry:
|
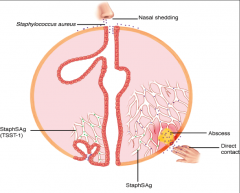
*Habitat = nasopharynx
*Rates among hospital personnel and patients are much higher. *Nasal shedding. *Once present on the skin, can gain deeper access either through skin or trauma. *Sag means superantigen -- leads to toxic shock syndrome. |
|
|
What aspects of s. aureus make it such a good pathogen?
|
It can:
*Evade phagocytosis *Produce surface proteins that mediate adherence of the bacteria to host tissues *Production of specific toxins and hydrolytic enzymes |
|
|
What CW factors make s. aureus a good pathogen?
|
*Teichoic acid and Fibronectin-binding proteins
*Capsule (anti-phagocytic) *Protein A (anti-phagocytic) |
|
|
What role do Teichoic acid and Fibronectin-binding proteins play in the virulence of s. aureus?
|

Important for adherence to host
|
|
|
What role do the capsule and Protein A play in the virulence of s. aureus?
|
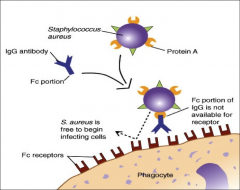
Defense against phagocytosis
|
|
|
What role do exotoxins play in the virulence of s. aureus?
|

Cytolytic or pore-forming:
*Alpha toxin (pore forming; tgts blood vessels) *Panton-Valentine Leukocidin (pore forming; atks leukocytes; MRSA expresses this) *Beta toxin (sphingomyelinase C is the tgt; pore forming in phospholipids) |
|
|
Discuss the exfoliative toxins of s. aureus:
|

*Exfoliative toxins A and B--Epidermolytic proteases
*Causes separation of the layers of the epidermis at the desmosomes. *Mediate Staphylococcal scalded skin syndrome (SSSS) |
|
|
Discuss TSST-1:
|

*An exotoxin in s. aureus.
*Toxic Shock Syndrome Toxin 1 (TSST-1) *A Superantigen: These toxins have an affinity for the CD4+ T cell receptor-MHC class II antigen complex at sites distinct from the classic antigen binding groove. |
|
|
When and why is TSST-1 produced?
|

*Produced during the course of infection with systemic disease as a result of absorption of toxin from the local site.
*ONLY the toxin crosses the mucosa of the vaginal tract and acts as a superantigen. *Cytokine-mediated effects. |
|
|
What is enterotoxin?
|
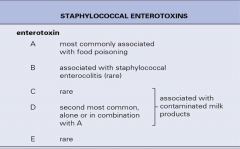
*An exotoxin from s. aureus.
*Food-poisoning, carried by humans -Superantigen -Not an infection -Food contaminated by humans - growth of bacteria - release of ENTEROTOXIN *Toxin stimulates vomiting center of the brain by binding to neural receptors in the upper GI tract. Very heat-stable. |
|
|
What virulent enzymes does s. aureus make?
|
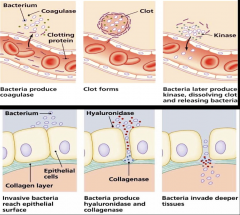
Coagulase
Catalase Hyaluronidase Staphylokinase Lipases *Allow s. aureus to invade and disseminate into deeper tissue. |
|
|
What two general types of infection do you see in s. aureus?
|
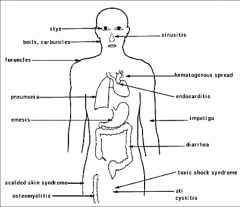
*Localized pyogenic infections
-Characterized by localized tissue destruction and abscess formation. *Disseminated toxin-mediated infections. -TSS and Scalded Skin Syndrome |
|
|
How do abscesses start to get formed in s. aureus?
|

-The alpha toxin forms a pore, lyses cell, and organism enters.
-Secretes coagulase, lays down fibrin, secludes organism. |
|
|
What is an abscess?
|
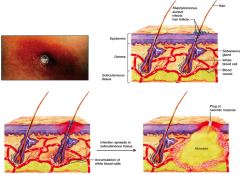
*Enclosed collection of liquefied tissue, known as pus, somewhere in the body. Enzymes made by the bacteria enable the destruction of inflammatory cells and thus the pouring out of lysosomal enzymes from neutrophils, which damage the surrounding tissue.
|
|

|

|
|
|
Streptococcus ; Gram+ cocci arranged in pairs or chains with oval cells
|
|
|
General traits of Strep:
|
*Catalase negative
*Gram+ cocci arranged in pairs or chains with oval cells *Members of normal flora *Genus includes: -Streptococcus pyogenes (Group A Strep) -Streptococcus agalactiae (GBS) -Streptococcus pneumoniae -Viridans streptococci |
|
|
How do you classify the different types of strep?
|
*According to their hemolytic pattern on a blood agar plate.
*Hemolysis on blood agar: growth on blood agar causes a chemical change in the hemoglobin of RBC’s. *alpha: partial hemolysis (greenish tinge) *ß: complete hemolysis; get subdivided *gamma: no hemolysis at all |
|
|
What are the Lancefield groupings?
|
*Lancefield groupings: serologic reactivity of cell wall carbohydrate antigens, which are antigenic and easily extractable with dilute acid.
-Lancefield antigens define the pyogenic streptococci; primarily b-hemolytic. -Divided into groups A through U -Clinically most important groups of b-hemolytic streptococci are types A and B. |
|
|
Classification of most important streptococcal pathogens:
|
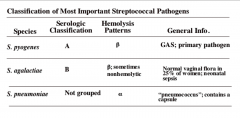
*pyogenes is most important (Group A strep)
*agalactiae is the Group B strep; normal vaginal flora that can infect infants during delivery. *Pneumoniae doesn't get grouped because it is an alpha hemolytic, not a ß-hemolytic; causes pneumonia. |
|
|
How can you classify the different kinds of strep by their biochemical properties?
|
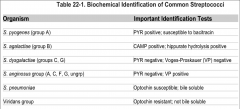
Biochemical properties: analyze the metabolism and presence of enzymes in the bacterium. Examples include catalase, L-pyrrolidonyl arylamidase (PYR) reaction.
*Catalase test is most important |
|
|
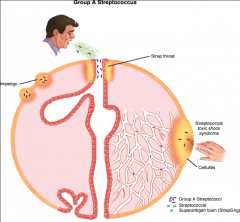
Describe group a strep:
|
*GAS is the most virulent of streptococcal group.
*Lives on human skin and mucous membranes; carriage rate as high as 20%. *Person-to-person spread via droplets; fomites; sometimes food borne. Very sturdy. *Causes suppurative (pyogenic) and non-suppurative diseases (acute rheumatic fever). |
|
|
Why is group A strep such a good pathogen?
|
-Not quite as versatile as s. aureus, but it has all these same traits.
*Pathology depends on the ability of the bacteria to: -Avoid opsonization and phagocytosis. -Produce surface proteins that mediate adherence of the bacteria to host tissues and invasion into the epithelial cells. -Production of specific toxins and hydrolytic enzymes. |
|
|
Encounter and Entry of GAS:
|
*Transiently colonize the URT and skin surface.
*Primary source of infection = respiratory droplets, direct contact or fomites. |
|
|
What are the most important virulence factors of GAS?
|
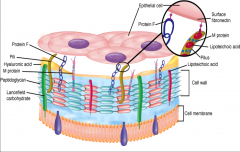
*Ones associated with the CW.
*Specifically, M Protein *Lipoteichoic acid *Lancefield carbohydrate *Protein F *Hyaluronic Acid capsule helps evade host immune response by mimicry |
|
|
Describe M protein in GAS:
|
*Major type-specific protein!
*Cell wall surface component that promotes antigenic variability *Used to differentiate strains; At least 80+ M protein serotypes of GAS exist. *Certain M-types are considered rheumatogenic since they contain antigenic epitopes related to heart muscle, and they therefore may lead to autoimmune rheumatic carditis (rheumatic fever) following an acute infection. |
|
|
Describe the structure of M protein in GAS:
|
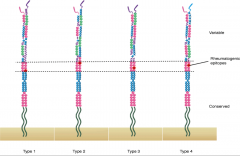
*Variable regions
*Epitope regions *Conserved regions |
|
|
What are the most important toxins and enzymes in GAS?
-Briefly describe what they are significant for. |
*Streptococcal pyrogenic exotoxins (Spe).
-The toxins act as superantigens. -Contributes to disease in necrotizing fasciitis and streptococcal toxic shock syndrome, as well as the rash observed in patients with scarlet fever. *Streptolysin S: (oxygen stable) -Lyses erythrocytes, leukocytes, and platelets. -Responsible for the characteristic β hemolysis seen on blood agar media. *Streptolysin O: (oxygen-labile) -Lysing erythrocytes, leukocytes, and platelets. -Antibodies are readily formed against streptolysin O and are useful for documenting recent group A streptococcal infection (anti-ASO test). *Streptokinase (A and B): -Lyse blood clots and fibrin deposits and facilitate the rapid spread of S. pyogenes in infected tissues. *C5a peptidase: -Disrupts the complement component C5a which mediates inflammation. *Exotoxin B: Protease |
|
|
Describe how GAS invades and spreads:
|

*Streptolysin O is pore-forming
*Other enzymes allow it to spread by interfering with complement (C5a peptidase), mimicking host (hyaluronidase). |
|
|
How do you categorize the different types of disease that GAS causes?
|
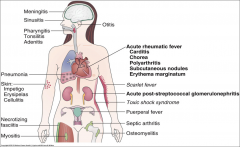
3 Categories:
*Pyogenic inflammation (skin, throat, ear, meningitis, necrotizing fasciitis) *Toxin-mediated infection (scarlet fever 2˚ to strep throat, toxic shock syndrome) *Immunological (acute rheumatic fever 2˚ to strep throat, acute post-strep glomerulonephritis 2˚ to strep throat OR cutaneous infection) |
|

|

Strep throat
|
|

|

-Acute stage of erysipelas caused by GAS.
-Organism isn't spreading; it's contained. |
|

|

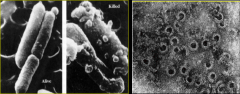
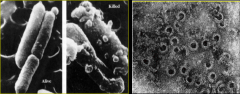
*Deep invasion with necrosis; necrotizing fasciitis (“flesh-eating bacteria”)
*A result of the different lytic enzymes in GAS. *Must debride thoroughly |
|

|
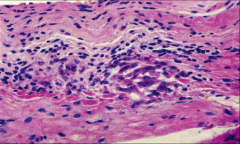
-A cellular reaction pattern consisting of lymphocytes and macrophages aggregated around fibrinoid deposits is found in human hearts. This lesion, called the Aschoff body, is considered characteristic of rheumatic carditis.
|
|
|
Briefly describe Viridans Strep:
|
*Heterogeneous collection of α-hemolytic and non-hemolytic streptococci. Their group name reflects the fact that many of these bacteria produce a green pigment on blood agar media (no Lancefield group).
*They colonize the oropharynx, gastrointestinal tract, and genitourinary tract. *This group of Streptococcus is responsible for various diseases, most notably dental caries (S. mutans); endocarditis (S. mitis); abscesses in brain, oropharynx or peritoneal cavity (S. anginosus). |
|
|
Briefly describe Strep pneumoniae:
|
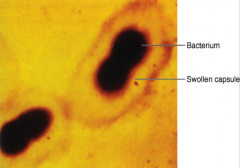
*Gram-positive, oval cocci arranged end-to-end in pairs.
*a-hemolytic streptococcus that colonizes the human nasopharynx. *Capsule is important virulence factor! Interferes with complement, opsonization, and phagocytosis. *It is a frequent etiologic agent of lower respiratory tract infections (pneumonia) and upper respiratory tract infections (otitis media, chronic bronchitis, sinusitis, and laryngitis). *Can also cause invasive infections such as bacteremia and meningitis. *Disease manifestations are characterized by an acute inflammatory response. |
|
|
strep pneumoniae
|
|
|
Describe the importance of the capsule of strep pneumoniae as a virulence factor:
|
*Antigenic diversity of polysaccharide capsule has lead to the generation of a large number of serotypes (>80).
*A small number, however, are responsible for the majority of cases and forms basis for polyvalent vaccine. *Vaccine contains the 23 most common serotypes and is recommended for the elderly and those with predisposing illnesses (children >2 years old and adults). |
|
|
How does strep pneumoniae invade and spread?
|
*Common inhabitant of the throat and nasopharynx in healthy people
*Typically aspirated from normal oropharyngeal flora to the lungs where it produces pneumonia. *Bacteremic spread can infect other sites = meningitis *Transmission via respiratory droplets, contaminated hands. |
|
|
How does GBS colonize the vagina and cause neonatal sepsis?
|

|
|
|
Virulence Factors of Strep Pneumoniae:
|
*Promotion of survival early in infection
-CAPSULE -Secretory IgA (sIgA) protease *Tissue destruction -Acute inflammatory response. -Pneumolysin: Intracellular, not secreted. Pore-forming toxin that causes tissue damage by destroying epithelial cells. -Pneumococcal cell wall components such as lipoteichoic acid induce cytokine release (IL-1 and TNF). These diffuse into bloodstream and cause systemic manifestations. |
|
|
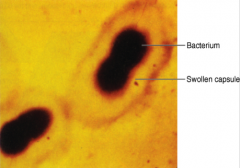
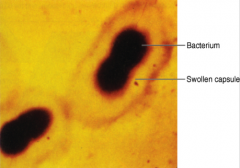
*S. pneumoniae
*Note the capsule |
|
|
Key points about enterococcus:
|
*ENDOCARDITIS and NOSICOMIAL INFECTIONS.
*Enteric bacteria which are commonly recovered in feces collected from humans and from a variety of animals. *Antibiotic-resistant strains has become a serious problem in hospitalized patients (nosocomial infection). *The urinary tract, peritoneum, and heart tissue are the sites involved most often. A particularly severe complication of enterococcal bacteremia is endocarditis. *The most commonly isolated and clinically important species are Enterococcus faecalis and Enterococcus faecium. |

