![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
92 Cards in this Set
- Front
- Back
|
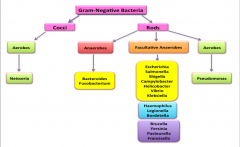
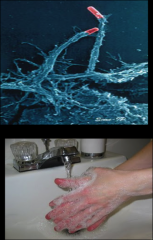
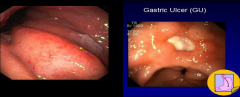
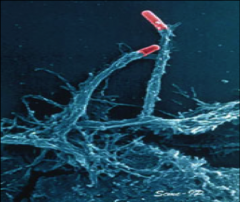
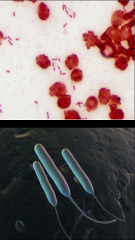
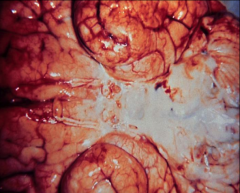
How do we visualize gram neg bacteria?
|

The peptidoglycan layer is thin and is overlaid by an outer membrane. In the stain, the decolorizer disperses the outer membrane and washes the crystal violet from the thin layer of peptidoglycan. Bacteria are visualized by the red counterstain (safranin).
*Photos on right are gram neg rods. |
|
|
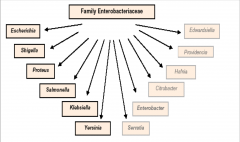
List all the gram neg rods:
|
|
|
|
List the gram ned rods that cause disease both within and outside the enteric tract:
|
Escherichia
Salmonella |
|
|
List all the gram neg rods that primarily cause disease within the enteric tract
|
Shigella
Campylobacter Helicobacter Vibrio |
|
|
List all the gram neg rods that only cause disease outside the enteric tract:
|
Klebsiella–Enterobacter–Serratia group
Proteus–Providencia–Morganella group Pseudomonas Bacteroides *especially associated with opportunistic infections. |
|
|
List all the gram neg rods that reside in the respiratory tract:
|
Haemophilus
Legionella Bordetella |
|
|
List all the gram neg rods that come from an animal source:
|
Yersinia
Brucella Pasteurella Francisella |
|
|
A 4-year old girl presents at the emergency room with bloody diarrhea, fever and vomiting. The child’s mother reports that the child has had these symptoms for about 24 hours and she has not passed any urine for about 12 hours. The child is enrolled in a day care center and the group had recently made a field trip to a fast food place to learn about different jobs. The children had a lunch of ground beef, fries and cola after meeting with different workers. This field trip was 4 days earlier on Friday. The child had a temperature of 39oC and showed physical signs of dehydration. Blood samples drawn showed evidence of greatly reduced kidney function and lysed red blood cells.
What is your diagnosis? What were the critical features to your diagnosis? What organism is responsible? What virulence factor mediates this disease? |
*E. coli (Shiga toxin caused bloody diarrhea).
*HUS from dirty ground beef. *4 day incubation period. |
|
|
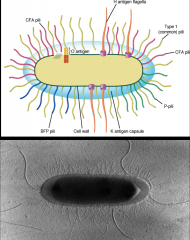
List the key points about Enterobacteriaceae:
Which are never part of the normal flora? |
*The largest, most heterogenous collection of medically important gram-negative rods.
*They are found in soil, water, vegetation, and in the colon of humans and other animals, many as part of the normal flora. *Salmonella serotype typhi and Shigella species are strict human pathogens!! |
|
|
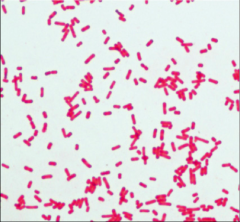
Describe the antigenic structure of Enterobacteriaceae family:
|
*O antigen- polysaccharide
*K antigen- capsule *H antigen *Serotypes are expressed with letter and number of the specific antigen, such as Escherichia coli O157:H7. |
|
|
List the most important disease-causing members of the enterobacteriaceae family:
|
|
|
|
In the enterobacteriaceae family, which are primary and which are opportunistic pathogens?
|
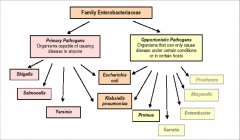
|
|
|
Describe the significance of the lactose fermentation test:
|

*Aids in the identification of pathogens among normal flora.
*Most enteric bacteria ferment lactose including E. coli--> show up red. *Primary enteric pathogens (i.e Shigella, Salmonella, and Yersinia) are unable to ferment lactose. *Employs Eosin-methylene blue (EMB) or MacConkey’s agar |
|
|
Describe the encounter and entry of Enterobacteriaceae:
|
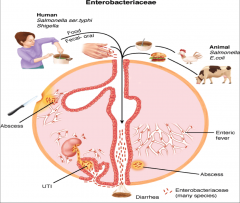
|
|
|
Decribe the significance of Endotoxins in Enterobacteriaceae:
-examples of systemic effects they can have? |

*A common virulence factor among Enterobacteriaceae.
*The activity of this toxin depends on the lipid A component of LPS, which is released at cell lysis. *Many of the systemic manifestations of gram-negative bacterial infections are initiated by endotoxin activation of complement, release of cytokines, leukocytosis, thrombocytopenia, disseminated intravascular coagulation, fever, decreased peripheral circulation, shock, and death. |
|
|
Decribe the significance of the capsule in Enterobacteriaceae:
|

*A common virulence factor among Enterobacteriaceae.
*Antigenic phase variation in K and H antigens--helps evade host immune system. *Type III secretion systems: like a syringe--injects virulence factors into tgt cell. |
|
|
Decribe the significance of the production of iron-binding siderophores and antimicrobial resistance in Enterobacteriaceae:
|

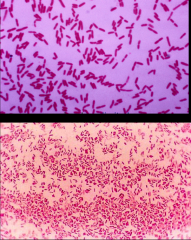
*Common virulence factor among Enterobacteriaceae.
*Antimicrobial resistance helps the bacteria live. *Conjugation (pictures, e. coli): the “mating” of two bacterial cells, during which DNA is transferred from one donor to the recipient. This horizontal gene transfer is controlled by plasmids. |
|
|
List the key points about Escherichia coli:
|

*Causes disease both within and outside the enteric tract
*Most abundant facultative anaerobe in the gut *Antigenically diverse. *Pathogenic strains are associated with specific serotypes, usually based on O and H antigens; sometimes K antigen is used. -O157:H7: linked to hemolytic uremic syndrome (HUS) outbreak. |
|
|
What kind of infections is e. coli involved in?
|
Important primary pathogen in three kinds of infections:
1. Gastrointestinal (diarrhea/colitis) 2. Urinary tract infection (UTI) 3. Neonatal meningitis E. coli is also an important opportunist! |
|
|
Describe the importance of pili in e. coli infection:
|
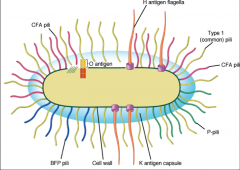
*Pili : Important in virulence as mediators of attachment to human epithelial surfaces.
*Type I: common pili; binds mannose on epithelial cell surfaces. *P pili: bind to digalactoside (Gal-Gal) residues on uroepithelial cells and certain erythrocytes. Cause UTIs. *Pili of diarrhea strains bind enterocytes. |
|
|
Describe the exotoxins produced by e. coli:
|
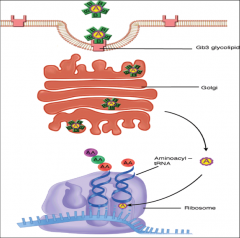
*Exotoxins that act in the enteric tract (a.k.a. enterotoxins)
*Two cause watery diarrhea: *Heat-labile toxin (LT): A-B exotoxin; The B subunit binds to the cell membrane, and the A subunit catalyzes the ADP-ribosylation of a regulatory G protein located in the membrane of the intestinal epithelial cell. Dysregulates cAMP-->diarrhea. *Heat-stable (ST): A-B exotoxin that stimulates guanylate cyclase. *Shiga Toxin (Stx): inhibits protein synthesis by altering tRNA binding site. |
|
|
Summary of the e. coli exotoxins:
|
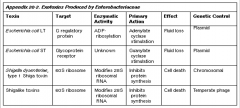
|
|
|
What are the 4 major classes of intestinal infections that e. coli is involved in:
|
EHEC: Enterohemorrhagic E. coli
EPEC: enteropathogenic E. coli ETEC: Enterotoxigenic E. coli EIEC: Enteroinvasive E. coli |
|
|
Describe Enterohemorrhagic E. coli:
|
*EHEC disease and the accompanying hemolytic uremic syndrome (HUS) are the result of consumption of products from animals colonized with EHEC strains.
*EHEC disease has emerged as an important cause of bloody diarrhea (Shiga) in developed nations and HUS linked to O157:H7 serotype. *Low infecting dose facilitates transmission (<100 organisms/gram of hamburger)!!!! *Modern meat processing facilitates widespread outbreaks. |
|
|
What's the common culprit in EHEC:
|
*O157:H7 is the most commonly identified serotype in U.S. (20,000-40,000 infections/yr).
*Hemolytic uremic syndrome (HUS) *Triad = hemolytic anemia, thrombocytopenia and renal failure (result of Shiga). Most common cause of renal failure in children <10 years old; fatal in 5-10% of cases. |
|
|
Unique traits to the pathogenesis in EHEC and EPEC:
|

*Organism attaches to microvilli on enterocyte via bundle-forming pili to initiate a process that mediates the rearrangement of actin and cytoskeletal elements.
*Process forms a “pedestal” or attachment and effacing (A/E) lesion at brush border. *Only known example of bacterium providing its own receptor for binding to target cell (Intimin). Also present in EPEC. |
|
|
Describe enteropathogenic E. coli:
|
*Watery diarrhea (no Shiga); in developing countries accounts for 20% of childhood diarrhea (infants <1 year); can be life threatening in infants due to dehydration.
*Transmission is by oral/fecal route, from infants cases and adult carriers. |
|
|
Describe enterotoxigenic E. coli:
|
*Watery diarrhea, most common cause of “traveler’s diarrhea”; affects adults and children. In developing countries ETEC is an important cause of infant diarrheas (high mortality); not common in U.S.
*Transmission is by consumption of food or water contaminated with human waste or by person-to-person contact (fecal/oral) *LT and ST are the toxins involved in pathogenesis. |
|
|
Describe Enteroinvasive E. coli:
|
*Bloody diarrhea; uncommon, often foodborne. Mostly seen in children <5 years old in developing nations.
*Humans only reservoir; similar to Shigella sonnei (less virulent serotype). *No toxins involved; self-limiting |
|
|
Summary of action of the 4 major classes of intestinal infections from e. coli:
|
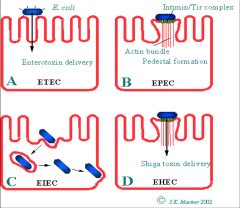
|
|
|
Summary of features of intestinal infecton by e. coli:
|
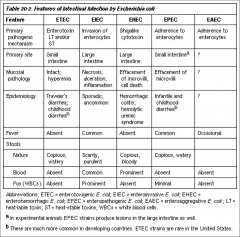
|
|
|
4 clinical syndromes resulting from salmonella enterica:
|
*Gastroenteritis = S. enteriditis
*Focal infection of vascular endothelium = S. typhimurium *Infections of specific organ systems (osteomyelitis) = S. typhimurium *Typhoid fever = S. typhi and S. paratyphi A and B (only human transmission; not in meat) |
|
|
Key points about salmonella enterica:
|

*single species; several serotypes
*Not a component of normal flora *Most species broadly distributed in nature, including important food sources *Fecal-oral transmission; may involve chronic carriers *Young children and elderly are highly susceptible |
|
|
Pathogenesis of salmonella infection:
|

*Enteric fever (typhoid, paratyphoid):
-In contrast to other serotypes, S. typhi exhibits prolonged intracellular survival in macrophages and continued multiplication. -They are carried to reticuloendothelial system. -Severe systemic infection with fever and abdominal symptoms results from endotoxin in blood. -S. typhi can colonize gall bladder and establish chronic infection (carried inside macrophages)--> typhoid fever. -Type 3 secretion system; forces non=phagocytic cells to phagocytose them. -They preferentially tgt M cells. |
|
|
Key points about Shigella:
|
*Non-motile and Unencapsulated
*Causes disease by invading and replicating in cells of the colon. *Strict human pathogen. *Low infecting dose facilitates fecal-oral spread. *It is acid-resistant and survives passage through the stomach to reach the intestine. *The incidence and spread of shigellosis is directly related to personal and community sanitary practices. In developed countries, it is largely a pediatric disease. *Most contagious bacterial diarrhea! |
|
|
What species of shigella have been described and what does each cause?
|
*S. dysenteriae (dysentery)
*S. flexneri and S. boydii (severe disease) *S. sonnei (milder; watery diarrhea) |
|
|
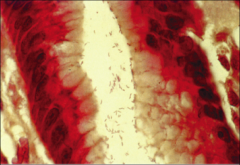
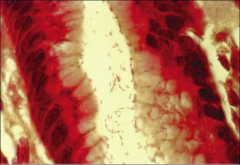
Pathogenesis of shigella:
|

*Shigella are acid-resistant (survive stomach)
*After ingestion, survive passage through stomach, the small intestines and enter the colon. *Bacterial multiplication occurs mainly in the intracellular environment of the intestinal epithelial cells. Tgts M cells. *Invasion triggers an intense acute inflammatory response with mucosal ulceration and abscess formation. Associated with frequent defecation, strain, painful cramping, and diarrhea with gross blood and mucus. |
|
|
Describe damage resulting from shigella:
|

*S. dysenteriae type 1 produces SHIGA TOXIN
*Shiga Toxin: second most potent toxin known; it is a cytotoxin that kills intestinal epithelial and endothelial cells. *A-B toxin (1A:5B) that cleaves the host 60S ribosomal RNA, thereby blocking protein synthesis. *It can decrease sodium absorption and lead to excess fluid in the lumen of the colon. Effects contribute to the blood diarrhea that characterizes dysentery. |
|
|
Key points about Campylobacter jejuni:
|
*motile, curved, slender, gram-negative rod; has polar flagella and a typical “S” shape or “seagull” appearance.
*Fastidious and slow-growing; Microaerophilic (low oxygen 5-10%) *Found in the GI flora of wild and domestic animals. No person-to-person spread. *Most common source of infection is undercooked poultry and unpasteurized milk. *Leading cause of acute diarrhea worldwide (2 million cases/yr in U.S.). Low ID50! |
|
|
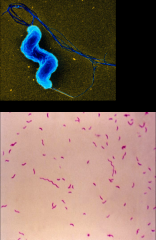
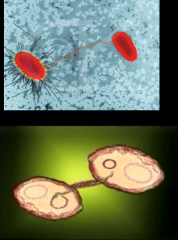
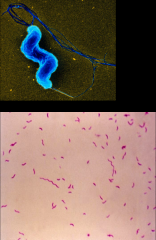
Key points about Helicobacter pylori:
|
*Motile, curved, slender, gram-negative rod; has polar flagella that facilitates penetration of mucous layer.
*Fastidious and slow-growing; Microaerophilic. *Produces urease enzyme that allows the organism to persist in low pH environment of the stomach by the generation of ammonia. *Vacuolating cytotoxin (VacA) causes apoptosis in eukaryotic cells it enters generating multiple large cytoplasmic vacuoles. |
|
|
Pathogenesis of h. pylori:
|
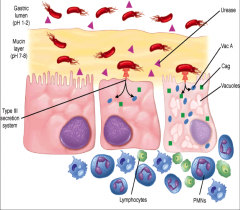
*urease is key for survival
*type 3 secretion *Vac A forms vacuoles. |
|
|
Describe long-term pathologic outcomes from h. pylori:
|
*Long-term pathologic outcomes are variable between infected persons:
*Ulceration (peptic ulcers) *Atrophic gastritis *Gastric cancer: second leading cancer in the world. *MALT (mucosa associated lymphoid tissue) lymphoma; most are completely eradicated by anti-Helicobacter pylori therapy. |
|
|
Briefly describe the enteric pathogens that only cause disease outside the enteric tract:
|
*Klebsiella–Enterobacter–Serratia group
These organisms are usually opportunistic pathogens that cause nosocomial infections, especially pneumonia and urinary tract infections. Also meningitis. *Proteus–Providencia–Morganella group These organisms primarily cause urinary tract infections, both community- and hospital-acquired. |
|
|
gram neg rods
|
|
|
When can bacteriodes be a problem?
|
It's a normal inhabitant of colon and vagina; if colon is perforated, they can cause opportunistic infection --> sepsis, abscesses, polymicrobial infections.
|
|
|

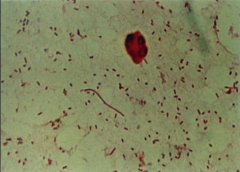
conjugating e. coli.
|
|

|

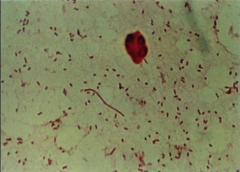
e. coli
|
|

|

EHEC/EPEC attachment to villi.
|
|

|

Salmonella.
|
|

|
shigella
|
|
|
2 pathogens that use acting polymerization to move from cell to cell:
|
Listeria
Shigella |
|
|
2 pathogens that use Shiga toxin:
|
-EHEC
-Shigella S. dysenteriae type 1 |
|
|
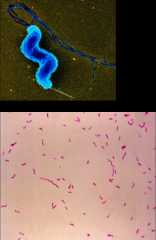
Campylobacter jejuni
|
|
|
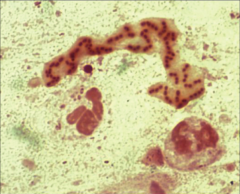
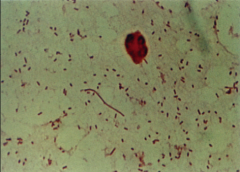
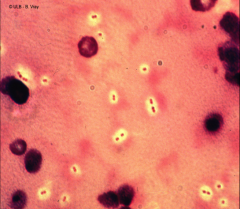
*h. pylori
*cytoplasmic vacuoles are visible |
|
|
What is sepsis and septic shock?
|
*Sepsis: the suspicion or proof of infection and evidence of a systemic response to infection, i.e. tachycardia, tachypnea, hyperthermia, or hypothermia. This response may be called systemic inflammatory response syndrome (SIRS).
*Septic shock: complex and life-threatening syndrome that results from sepsis. Hypotension. -Affects 750,000 people/year -Death rates = 20% for sepsis and >60% for septic shock. -Patients typically have underlying disease, trauma, or surgery; most cases are also nosocomial. |
|
|
How does sepsis occur?
|
*Alarm reaction to bacterial infection: Protective when localized, dangerous when systemic.
*Local: reaction mobilizes host defenses via cytokine release and inflammation, prior to activation of specific immune responses. Localized alarm reaction established at a site of infection is highly beneficial by concentrating anti-bacterial defenses. *Systemic (sepsis): catastrophic; triggered systemically by overwhelming and systemic invasion of bacteria and/or their debris. Bacteremia is common although not required. |
|
|
What is recognized to make sepsis happen in gram negative organisms?
|
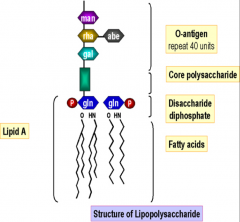
*Lipopolysaccharide (LPS, Lipid A portion) = ENDOTOXIN
|
|
|
What is recognized to make sepsis happen in gram positive bacteria?
|
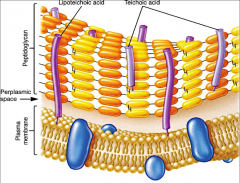
*Lipoteichoic and teichoic acid in cell of Gram-positive bacteria
|
|
|
What is the LPS response?
|

|
|
|
Another look at all the rxns LPS can elicit in the body:
|

*DIC ain't good.
|
|
|
Key points about pseudomonas aeruginosa:
|
*Aerobic, motile, Gram-negative rod with polar flagella.
*Widely distributed in nature. *Aerobic growth with minimal nutritional requirements. *Non fermenter and oxidase positive. *A major opportunistic pathogen!!!! |
|
|
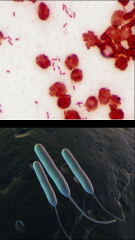
pseudomonas aeruginosa
|
|
|
What pigments does pseudomonas aeruginosa produce that are useful in identification?
|
*Blue Pyocyanin = blue pigment
*Pyoverdin = yellow-green pigment that fluoresces under UV light. *Pyoverdin + Pyocyanin diffusion into agar = blue-green color |
|
|
What kind of pseudomonas aeruginosa do you see in CF patients?
|
Strains that secrete alginate slime layer.
|
|
|
Pathogenesis of pseudomonas aeruginosa:
|
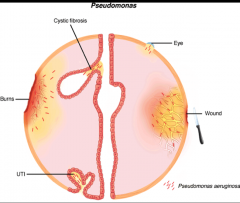
*An opportunistic pathogen of immunocompromised individuals.
*It typically infects the pulmonary tract, urinary tract, burns, wounds. *Frequent colonizer of medical devices. *Most common cause of nosocomial pneumonias and invasive infection. |
|
|
Virulence factors of pseudomonas aeruginosa:
|
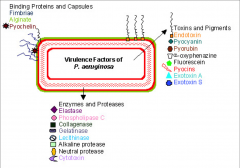
lots
|
|
|
How does pseudomonas aeruginosa destroy cells and enter the blood?
|
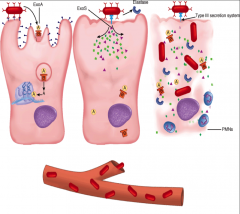
*ExoA
*ExoS *Type 3 secretion All this --> sepsis |
|

|

Hot tub folliculitis from pseudomonas aeruginosa.
|
|
|
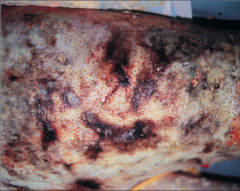
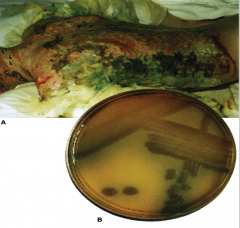
Burn infection from pseudomonas aeruginosa.
|
|

|

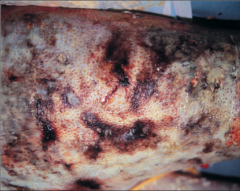
Ecthyma gangrenosum: bacterial infection caused by P. aeruginosa that results in black necrotic lesions; usually in immunocompromised
|
|
|
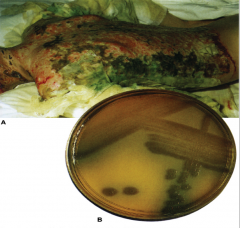
Pseudomonas aeruginosa: The blue color of pyocyanin when mixed with yellow tissue or media components typically produces a green discoloration. This is sometimes seen in clinical cases and on culture plates.
|
|
|
Key points about Haemophilus influenzae:
|
*Small Gram-negative rod (coccobacilli)
*Two classes of bacteria- 1) Nonencapsulated. Part of normal flora. Causes bronchitis, otitis media, sinusitis, conjunctivitis. No invasive disease. 2) Encapsulated. Six serological types (a-f); “Hib” = Haemophilus influenzae type b, associated with invasive disease, especially in young children. Can cause meningitis, epiglottitis, and cellulitis. *Both classes require X factor (hematin) and V factor (Nicotinamide adenine dinucleotide; NAD) for growth in culture. |
|
|
Pathogenesis of invasive H. influenzae: Encounter:
|
*Humans only natural host. Spread via aerosols to nasal epithelium. 3-5% carrier rate for encapsulated strains, nonencapsulated strains have a higher carrier rate.
*Nasopharyngeal colonization - Binds to epithelium and mucus; replication occurs and can invade locally. - IgA protease is a mucosal virulence factor - LPS: endotoxin, impairs ciliary function. |
|
|
Spread and damage from H. influenzae:
|
- Local: sinusitis, otitis media
- Systemic: Invasion at sites of epithelial damage, gain access to blood by traveling through endothelial cells. In the absence of antibodies, a high-grade bacteremia can develop, with dissemination to meninges. *LPS is proinflammatory *LPS causes damage to epithelial cells |
|
|
Haemophilus influenzae
|
|
|
Importance of the capsule in Haemophilus influenzae:
|
*Most important virulence factor for invasiveness; consists of polyribitol phosphate (PRP). Like pneumococcal capsule, promotes survival in blood and inhibits phagocytosis.
*Immunity and Vaccination -Young children do not generate an efficient antibody response to carbohydrate antigen. -Type b antigen conjugated to a protein (toxoid) is effective in children with immature immune system. |
|
|
What DOESN'T bind to the capsule in Haemophilus influenzae?
|
IgG and C3b
|
|
|
What else has a capsule similar to Haemophilus influenzae?
|
*Streptococcus pneumoniae
*a-hemolytic streptococcus that colonizes the human nasopharynx. *It is a frequent etiologic agent of lower respiratory tract infections (pneumonia) and upper respiratory tract infections (otitis media, chronic bronchitis, sinusitis, and laryngitis). *Can also cause invasive infections such as bacteremia and meningitis. *Disease manifestations are characterized by an acute inflammatory response. **There are more** |
|
|
What pathogens have capsules that act as virulence factors?
|
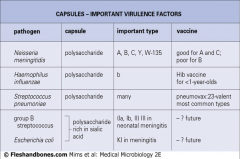
*Top 3 are most important
|
|
|
What key enzyme must bacteria have to survive in the mucosal epithelium and ultimately cause meningitis?
|
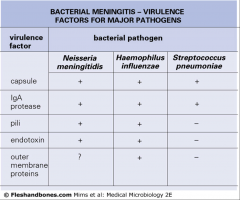
*IgA protease
*The gram negs have LPS endotoxin |
|
|
Main diseases caused by different kinds of haemophilus?
|
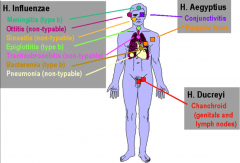
*aegyptius = conjunctivitis
*ducreyi = STI |
|
|
Key points about Haemophilus ducreyi:
|

*Sexually transmitted bacterial infection.
*Highly infectious and can invade on contact. *Major ulcerative disease in tropical and subtropical regions. *Lesions on skin and mucous membranes can progress to become ulcers with inguinal lymphadenopathy (bubos) |
|

|

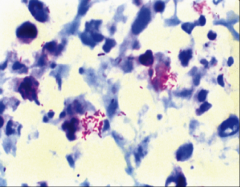
*Haemophilus ducreyi
*Lesions on skin and mucous membranes can progress to become ulcers with inguinal lymphadenopathy (bubos) |
|
|
Key things about bordetella?
|
*Bordetella pertussis causes whooping cough. Produces pertussis toxin
*Requires NAD iot grow *Similar to haemophilus (growth factors, resp. tract) |
|
|
Summary table of features of Haemophilus and Bordetella:
|

|
|
|
Key points about Legionella pneumophila:
|

*Gram-negative rods that stain faintly with standard Gram stain. Dieterle silver stain is used to visualize organisms.
*Requires charcoal yeast extract enriched with iron and L-cysteine for growth. *Common microbial cause of community-acquired pneumonia requiring hospitalization. Incidence has increased with central air conditioning systems in hotels, hospitals and office buildings. *Age, smoking, chronic lung disease and immunosuppression are all risk factors. *The organism parasitizes protozoa in the environment. *Typically found in non-marine aquatic environments. Human infection is an unfortunate “encounter”. |
|

|

Legionella pneumophila
|
|
|
Encounter and Entry of Legionella pneumophila:
|
*Typically inhaled from aerosol generated from contaminated water systems. The organism can colonize plumbing systems, cooling towers, air conditioning units because it lives inside protozoa. Has also been found in tap water, faucets and shower heads; highly resistant to heat.
*No person to person transmission! *Establishment of niche and multiplication: -Dependent on dose and host factors. -Infects the alveolar macrophage. |
|
|
Pathogenesis of Legionella pneumophila:
|
*L. pneumophila enters macrophage and secreted proteins block fusion of phagosome with lysosome. Inside the phagosome “vacuole”, the bacteria multiply within protected environment.
|
|
|
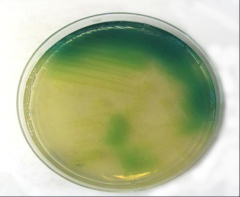
*Legionella
*Shows the gram neg rod within a macrophage |
|
|
*Coiling phagocytosis in Legionella pneumophila: Organism controls vesicular traffic (ribosomes, RER, mitochondria) to create replicative vacuole.
*Multiplication within macrophage reaches very high numbers. |
|
|
Virulence factors in Legionella pneumophila:
|
*Elicits a potent host immune response. Microabscesses with PMN’s, macrophages, fibrin, RBC’s and cell debris may form. Manifests itself as patchy or interstitial infiltrates in chest X-ray.
*LPS contributes to this inflammation. Several hydrolytic enzymes (metalloproteinase, phospholipase C) are also made by organism. |

