![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
110 Cards in this Set
- Front
- Back
|
A lymph node biopsy demonstrates normal architecture w/ a capsule, subscapular sinus, follicles, and paracortex.
Is this description likely to be localized or extensive? Mild or marked lymphadenopathy? |
This describes a reactive process because you can still see the normal architecture, therefore:
- Localized - Mild lymphadenopathy |
|
|
A lymph node biopsy demonstrates normal architecture w/ a capsule, subscapular sinus, follicles, and paracortex.
Is this description likely to be associated with a low grade fever or drenching night sweats? |
This describes a reactive process because you can still see the normal architecture, therefore:
Low grade fever |
|
|
A lymph node biopsy demonstrates normal architecture w/ a capsule, subscapular sinus, follicles, and paracortex.
Is this description likely to be caused by polyclonal or monoclonal B and/or T/NK cells? |
This describes a reactive process because you can still see the normal architecture, therefore:
Polyclonal B and T/NK cells |
|
|
A lymph node biopsy demonstrates a capsule, no sinuses (occluded), no follicles or paracortex.
Is this description likely to be localized or extensive? Mild or marked lymphadenopathy? |
This describes a malignant process because it is missing the normal architecture, therefore:
- Extensive - Marked lymphadenopathy |
|
|
A lymph node biopsy demonstrates a capsule, no sinuses (occluded), no follicles or paracortex.
Is this description likely to be associated with a low grade fever or drenching night sweats? |
This describes a malignant process because it is missing the normal architecture, therefore:
- Drenching night sweats (this is a "B symptom of lymphoma") |
|
|
A lymph node biopsy demonstrates a capsule, no sinuses (occluded), no follicles or paracortex.
|
This describes a malignant process because it is missing the normal architecture, therefore:
- Monoclonal B and/or T/NK cells |
|
|
What are the B symptoms of lymphoma?
|
Constitutional symptoms (eg, significant fever, night sweats, >10% weight loss)
|
|
|
How does the duration and growth interval compare for a reactive vs neoplastic lymphadenopathy?
|
- Reactive: self limited over short time course, w/ stable / small growth
- Neoplastic: longer duration and rapidly expanding |
|
|
How does the size compare for a reactive vs neoplastic lymphadenopathy?
|
- Reactive: Mildly enlarged
- Neoplastic: Very large |
|
|
How does the location and extent compare for a reactive vs neoplastic lymphadenopathy?
|
- Reactive: found at site of infection, lymph node in that area is enlarged
- Neoplastic: lymph nodes enlarged in area that you can't explain, can be more dispersed |
|
|
How does the tenderness compare for a reactive vs neoplastic lymphadenopathy?
|
- Reactive: tender
- Neoplastic: non-tender |
|
|
How does the mobility compare for a reactive vs neoplastic lymphadenopathy?
|
- Reactive: mobile (normal)
- Neoplastic: fixed |
|
|
What are some reactive causes of Lymphadenopathy?
|
– Infectious
– Autoimmune – Drugs – Foreign body – Castleman’s disease – Sarcoidosis – Kikuchi-Fujimoto – Kimura’s disease – Rosai Dorfmann |
|
|
What are some neoplastic causes of Lymphadenopathy?
|
– Lymphoma
– Leukemic involvement • Lymphoblastic lymphoma • Myeloid sarcoma – Metastatic tumor |
|
|
What histologic pattern in the lymph nodes is associated with infectious mononucleosis?
|
PARACORTICAL hyperplasia in lymph node because this is where the T cells are expanding
|
|
|
What are the histologic patterns of lymphadenopathy?
|
– Follicular hyperplasia
– Paracortical hyperplasia – Sinus histiocytosis – Necrotizing – Granulomatous – Mixed |
|
Case 1: 55y man evaluated for lumps on both sides of neck that have been present for 6 months. No fever, night sweats, weight loss, or recent illness. Lymph nodes are 1-2 cm and palpable on both sides of neck, axillae, and inguinal lymph node regions. Mild splenomegaly.
Based on the clinical information, what is the most likely diagnosis? |
Follicular Lymphoma because he presents with an indolent course
- Burkitt lymphoma and DLBCL are more aggressive processes and he does not have any "B symptoms" - CLL/SLL is also indolent - Hodgin Lymphoma is more localized - Infectious mononucleosis is not expected in this old of a patient |
|
Case 1: 55y man evaluated for lumps on both sides of neck that have been present for 6 months. No fever, night sweats, weight loss, or recent illness. Lymph nodes are 1-2 cm and palpable on both sides of neck, axillae, and inguinal lymph node regions. Mild splenomegaly.
An excisional lymph node biopsy is done in the axilla. What benign finding is in the histologic differential diagnosis? |
Follicular Hyperplasia
- Follicles are very close together and large - No mantle zone or germinal center - Diffuse across lymph node |
|
|
Case 1: 55y man evaluated for lumps on both sides of neck that have been present for 6 months. No fever, night sweats, weight loss, or recent illness. Lymph nodes are 1-2 cm and palpable on both sides of neck, axillae, and inguinal lymph node regions. Mild splenomegaly.
Flow cytometry of this lymph node reveals a clonal B cell population, which has low forward scatter and is CD5(-), CD10(+), CD19(+), CD20(+), and CD23(-). Which chromosomal translocation is likely to be present on cytogenetic analysis? |
t(14;18)
|
|
|
What diseases are associated with the following cytogenetic transformations?
- t(8;14) - t(15;17) - t(11;14) - t(14;18) - t(12;21) |
- t(8;14) - Burkitt Lymphoma
- t(15;17) - Acute Promyelocytic Leukemia (APL) - t(11;14) - Mantle Cell Lymphoma - t(14;18) - Follicular Lymphoma - t(12;21) - B-ALL |
|
|
Case 1: 55y man evaluated for lumps on both sides of neck that have been present for 6 months. No fever, night sweats, weight loss, or recent illness. Lymph nodes are 1-2 cm and palpable on both sides of neck, axillae, and inguinal lymph node regions. Mild splenomegaly.
He is diagnosed with Follicular Lymphoma based on cytogenetic analysis t(14;18). He decides to defer treatment and be monitored. 18mo later they decide to treat d/t increasing fatigue. CT scan shows similar sites of involvement as initial presentation. What is the most appropriate treatment at this time? |
Chemotherapy and anti-CD20 monoclonal antibody therapy (Rituximab)
|
|
|
How should you treat Follicular Lymphoma?
|
- There is no survival benefit for treating right away
- Wait and observe until they get certain symptoms (eg, bad B symptoms, rapidly increasing lymph nodes, decreased normal blood counts, splenomegaly causing sx, etc) Treatment options: - Rituximab alone - Rituximab + chemotherapy - Radio-immunotherapy - Transplant for some relapsed patients |
|
|
What is the function of Rituximab?
|
- Chimeric (mouse/human) IgG kappa monoclonal Ab
- Binds to CD20 antigen on B cells (marker of maturity) - t1/2 = 76 hours after 1st infusion and 205 hours after 4th infusion |
|
|
What is the possible mechanism of Rituximab?
|
- Complement-Dependent Cytotoxicity (CDC)
- Antibody-Dependent Cellular Cytotoxicity (ADCC) - Apoptosis |
|
|
What happens in the Antibody-Dependent Cellular Cytotoxicity mechanism of Rituximab?
|
- Abs bind CD20 instead of triggering complement
- They help to attract cytotoxic T cells to this target (tumor cells) - Once cytotoxic cells engage those Abs it releases granzymes and perforins that kill cell |
|
|
What happens in the Apoptosis mechanism of Rituximab?
|
Just by having Ab bind to CD20 triggers some intracellular events that cause it to undergo apoptosis
|
|
|
What is the prognosis for Follicular Lymphoma?
|
- Advanced stage disease that is usually incurable
- Highly treatable when symptoms are present but not curable |
|
|
What do you need to know to diagnose Follicular Lymphoma?
|
Whether CD20 is on the cells - important for whether Rituximab will work (anti-CD20)
|
|
Case 1: 55y man evaluated for lumps on both sides of neck that have been present for 6 months. No fever, night sweats, weight loss, or recent illness. Lymph nodes are 1-2 cm and palpable on both sides of neck, axillae, and inguinal lymph node regions. Mild splenomegaly.
He is diagnosed with Follicular Lymphoma based on cytogenetic analysis t(14;18). 8 months later he develops sudden onset of fatigue and night sweats along w/ rapidly growing sites of adenopathy in neck and groin. Excisional LN biopsy is performed. What proteins are expected to be over-expressed? |
This biopsy shows the "starry night" pattern which indicates the Follicular Lymphoma transformed into Burkitt Lymphoma
- c-MYC - characteristic of Burkitt lymphoma, t(8;14) - BCL-2 - over-expressed in original Follicular lymphoma |
|
|
What would Cyclin D1 overexpression and CD5+ be indicative of?
|
Mantle Cell Lymphoma
|
|
|
What would c-Myc and BCL-2 over-expression be indicative of?
|
- Burkitt Lymphoma that progressed from Follicular Lymphoma
- Diffuse Large B-Cell Lymphoma |
|
|
What would CD30+ and CD15+ be indicative of?
|
Classical Hodgkin Lymphoma
|
|
|
What can Follicular Lymphoma transform into?
|
- 1/3 transform into Diffuse Large B Cell Lymphoma
- Smaller amount transform into Burkitt Lymphoma (c-Myc and starry night appearance) |
|
|
What are the low grade B-cell Non-Hodgkin Lymphomas (NHLs)?
|
– Chronic lymphocytic leukemia/Small lymphocytic lymphoma (CLL/SLL)
– Follicular lymphoma – Marginal zone lymphoma – Lymphoplasmacytic lymphoma |
|
|
What are the high grade B-cell Non-Hodgkin Lymphomas (NHLs)?
|
- Diffuse Large B Cell Lymphoma
- Burkitt Lymphoma |
|
|
How do you treat Diffuse Large B-Cell Lymphoma? Prognosis?
|
- Curable (50-60% w/ conventional therapy)
- Combination of mAb (Rituximab) and conventional chemotherapy (6 cycles) - Transplant in 1st relapse for most patients |
|
|
What are the B-NHLs that have small tumors?
|
- Follicular lymphoma
- Marginal zone lymphoma - Lymphoplasmacytic lymphoma - CLL/SLL |
|
|
What are the B-NHLs that have medium to large (2x normal size) tumors?
|
- Diffuse Large B Cell Lymphoma
- Burkitt Lymphoma |
|
|
What are the B-NHLs that have can have any size of tumors?
|
Mantle Cell Lymphoma
|
|
|
What are the B-NHLs that have a nodular, follicular architecture? What size are they?
|
Small Tumors
- Follicular lymphoma - Lymphoplasmacytic lymphoma - CLL/SLL Any Size Tumors - Marginal zone lymphoma |
|
|
What are the B-NHLs that have diffuse architecture? What size are they?
|
Medium to Large Tumors
- Diffuse Large B Cell Lymphoma - Burkitt Lymphoma |
|
|
How can you distinguish the small B cell Leukemia / Lymphomas?
|
CD5+ CD23+
- CLL/SLL CD5+ CD23- - Mantle Cell Lymphoma CD5- CD10+ - Follicular Lymphoma CD5- CD10- - Marginal Zone Lymphoma |
|
|
Which small B-NHL is CD5+ CD23+?
|
CLL/SLL
|
|
|
Which small B-NHL is CD5+ CD23-?
|
Mantle Cell Lymphoma
|
|
|
Which small B-NHL is CD5+ CD10+?
|
Follicular Lymphoma
|
|
|
Which small B-NHL is CD5+ CD10-?
|
Marginal Zone Lymphoma
|
|
|
Which lymphoma has a t(14;18) translocation? Genes? Functions?
|
Follicular Lymphoma (IgH and BCL-2)
- BCL-2 overexpression inhibits normal apoptosis (also seen in Extra-Nodal Marginal Zone Lymphoma, but characteristic of F.L.) |
|
|
Which lymphoma has a t(11;14) translocation? Genes?
|
Mantle Cell Lymphoma (IgH and CyclinD1)
- Overexpression of Cyclin D1 modifies cell cycle (minor population of plasma cell myeloma and hairy cell leukemia) |
|
|
Which lymphoma has a t(8;14) translocation? Genes?
|
Burkitt Lymphoma (c-MYC and IgH)
(most common) |
|
|
Which lymphoma has a t(2;8) translocation? Genes?
|
Burkitt Lymphoma (c-MYC and kappa light chain)
|
|
|
Which lymphoma has a t(8;22) translocation? Genes?
|
Burkitt Lymphoma (c-MYC and lambda light chain)
|
|
|
Which lymphoma has a t(11;18) translocation?
|
Marginal Zone Lymphoma
|
|
|
How do you distinguish between Follicular Lymphoma and Follicular Hyperplasia?
|
Presence of BCL-2 denotes Follicular Lymphoma (but appear identical histologically)
|
|
|
What are the types of T/NK Cell Lymphomas?
|
- Peripheral T cell Lymphoma
- Anaplastic T cell Lymphoma, ALK+ - Extra-nodal Nk/T-cell Lymphoma |
|
|
What are the characteristics of T/NK Cell Lymphomas?
|
- Uncommon in US (more in Asia)
- Aggressive tumors (generally) |
|
|
Case 2: 16 yo previously healthy female presents w/ 3-day hx of sore throat and fatigue. Pharynx is red w/ white exudate (pus). Rapid test for Strep is negative. Physician makes presumptive diagnosis of infectious mononucleosis.
What is the most likely clinical course for this infection? |
Self-limited
|
|
|
Case 2: 16 yo previously healthy female presents w/ 3-day hx of sore throat and fatigue. Pharynx is red w/ white exudate (pus). Rapid test for Strep is negative. Physician makes presumptive diagnosis of infectious mononucleosis.
14-y brother who is on immunosuppressive meds for kidney transplant. 2y later brother develops enlarged cervical lymph node, diagnosed as a B cell lymphoma. Positive for EBV. What is true about his tumor? |
Neoplastic proliferation dependent on a viral-encoded oncogene (EBV)
|
|
|
What are the symptoms of Infectious Mononucleosis?
|
- Lymphadenitis
- Hepatitis - Splenitis - Pneumonitis - Meningitis - Encephalitis |
|
|
What kind of virus is EBV?
|
- Gammaherpesvirus
- Large double-stranded DNA - Enveloped - labile in environment |
|
|
What are the life cycles of EBV?
|
- Lytic replication
- Latency |
|
|
What are the steps during the lytic replication of EBV?
|
1. Binding and fusion
2. Viral vhs degrades host mRNA 3. Viral transcription factor VP16 initiates transcription 4. HSV alpha gene transcribed by host RNA pol II 5. Alpha gene products activate beta genes 6. Beta gene products required for viral DNA synthesis 7. Triggers gamma viral genes 8. Gamma gene products are structural components of virion 9. Viral DNA packed into capsid and forms mature virion |
|
|
What is responsible for degrading host mRNA in a EBV infection?
|
Viral vhs
|
|
|
What EBV genes are transcribed first? How?
|
HSV alpha genes - transcribed by RNA polymerase II
|
|
|
What is the function of HSV alpha genes?
|
Activates beta gene transcription
|
|
|
What is the function of HSV beta genes?
|
Required for viral DNA synthesis, which triggers gamma viral genes
|
|
|
What is the function of HSV gamma genes?
|
Structural components of virion
|
|
|
What does EBV do before deciding a host is acceptable for latent infection?
|
Expresses immediate early (alpha) and early (beta) virus lytic genes
|
|
|
How is viral DNA maintained in a host?
|
Circular viral DNA is associated w/ host nucleosomes (viral chromatin) and maintained as an episome
|
|
|
How do you maintain latency of EBV infection?
|
Histones bear repressive "histone code" resulting in very little if any virus gene expression
|
|
|
What do latently EBV infected cells express in healthy people?
|
No EBV proteins or only EBNA1 (a poorly immunogenic protein that is responsible for viral episome maintenance in infected cells)
|
|
|
What is the function of EBV EBNA1?
|
A poorly immunogenic protein that is responsible for viral episome maintenance in infected cells
|
|
|
How do you trigger EBV reactivation from B cells?
|
- Triggered by B cell differentiation into plasma cell
- XBP-1 transcription factor induced during plasma cell differentiation to activate expression of viral lytic genes |
|
|
What are the physiological triggers of reactivation of EBV?
|
- Immunocompromise
- Stress - Infections with other viruses |
|
|
What is a significant risk factor for EBV-driven malignancies?
|
Poorly controlled reactivation of B cells
|
|
|
What are EBV EBERs?
|
- EBV encoded RNA that is transcribed in all infected cells (lytic and latent)
- Never translated into protein |
|
|
What are the types of latency for EBV? Implications?
|
- Latency Type 0: all viral protein translation is shut off
- Latency Type I: progresses to Burkitt Lymphoma or gastric cancer - Latency Type II: progresses to lymphoma, HL, NHL - Latency Type III: progress to lymphoma |
|
|
How is infectious EBV secreted?
|
In saliva (even in healthy people)
|
|
|
What are the implications of EBV infection in first decade of life?
|
Mild cold-like symptoms
|
|
|
What are the implications of EBV infection in adolescence and beyond?
|
Acute infection clinically defined as Infectious Mononucleosis ("kissing disease")
|
|
|
How common is EBV exposure in developed countries by age 12?
|
~70% because of child care, parents' hygiene habits, etc
|
|
|
How common is EBV exposure in developed countries by adulthood?
|
>95% infected
|
|
|
What is Infectious Mononucleosis characterized by?
|
- Massive expansion of CD8+ T-cells (including in circulation) = "Downey cells"
- Many if not all specific for EBV-infected B cells (latency III and II) - Increase in activated B cells, leads to transient increase in production of antibodies against self antigens and against esoteric antigens expressed by other species - Basis of heterophile test that measures antibodies against pig or horse antigens |
|
|
What is the basis of the Monospot test?
|
- Testing for presence of antibodies against pig or horse antigens
- In infectious mononucleosis there is an increase in activated B cells some of which produce Abs against esoteric Ags expressed by other species |
|
|
What are the symptoms of Infectious Mononucleosis?
|
- Fever
- Lymphadenopathy - Hepatosplenomegaly - Pharyngitis - Malaise and fatigue - Virus in saliva |
|
|
What are the laboratory findings of Infectious Mononucleosis?
|
- Atypical lymphocytes
- Heterophile antibody titer (monospot test) |
|
|
What are the mechanisms of EBV viral oncogenesis?
|
- Direct transformation
- Hit-and-run - Bystander effect - Chronic inflammation |
|
|
What is required for direct transformation for EBV viral oncogenesis?
|
>80% of cancer cells are virus positive
|
|
|
What is required for hit-and-run for EBV viral oncogenesis?
|
- Virus changes cellular environment and promotes mutagenesis
- Once transformation occurs, virus is not needed and is lost in dividing cells |
|
|
What is required for bystander effect for EBV viral oncogenesis?
|
- Virus-infected cells secrete a "storm" of growth factors
- Eventually transform uninfected neighbors |
|
|
What is required for chronic inflammation for EBV viral oncogenesis?
|
- Chronic and excessive stimulation of immune response by virus
- Produces toxic products, such as Reactive Oxygen Species, that induce genome instability and cancer |
|
|
Case 3: 20y woman is evaluated fro lump in R side of neck that has been present for 4 months and grown larger in last month. No fever, night sweats, weight loss, or recent illness. 3.5cm R anterior cervical lymph node and 1cm R supraclavicular lymph node are palpable. Lab studies, CBC, monospot, all normal.
What should you do now? |
Immediate lymph node biopsy
|
|
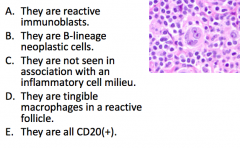
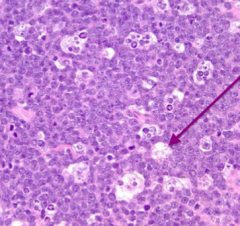
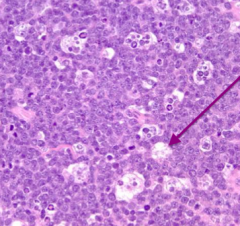
Case 3: 20y woman is evaluated fro lump in R side of neck that has been present for 4 months and grown larger in last month. No fever, night sweats, weight loss, or recent illness. 3.5cm R anterior cervical lymph node and 1cm R supraclavicular lymph node are palpable. Lab studies, CBC, monospot, all normal.
What is true about these cells? |
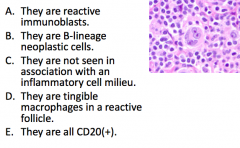
B-lineage neoplastic cells
|
|
Case 3: 20y woman is evaluated fro lump in R side of neck that has been present for 4 months and grown larger in last month. No fever, night sweats, weight loss, or recent illness. 3.5cm R anterior cervical lymph node and 1cm R supraclavicular lymph node are palpable. Lab studies, CBC, monospot, all normal.
Immunohistochemistry is performed to evaluate these large cells. Given the staining pattern what have we learned? |
CD30 and CD15 positive
|
|
Case 3: 20y woman is evaluated fro lump in R side of neck that has been present for 4 months and grown larger in last month. No fever, night sweats, weight loss, or recent illness. 3.5cm R anterior cervical lymph node and 1cm R supraclavicular lymph node are palpable. Lab studies, CBC, monospot, all normal.
Cells are present in nodules and separated by bands of fibrosis. What is the expected finding on imaging? |
Mediastinal mass / lymphadenopathy
(Nodular Sclerosis HL presents w/ mediastinal mass) |
|
|
What are the characteristics of Hodgkin Lymphoma?
|
- Reed Sternberg cells
- Contiguous spread - Lymph node involvement - More commonly in young adults |
|
|
What is required to diagnose Hodgkin Lymphoma?
|
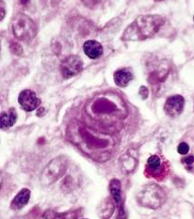
Reed Sternberg cells
- Large - Frequent binucleation - Large, eosinophilic nucleoli ("owl eyes") |
|
|
What are the variants of Reed Sternberg cells in Hodgkin Lymphoma subtypes?
|
- Lacunar cells (large clearing around RS cell) = seen in Nodular Sclerosis HL
- L&H cells (popcorn cells) = seen in Nodular lympohcyte predominant |
|
|
What are the classical sub-types of Hodgkin Lymphoma? Most common?
|
- Nodular Sclerosis (most common)
- Mixed Cellularity - Lymphocyte Predominant - Lymphocyte Depleted |
|
|
Nodular Sclerosis Hodgkin Lymphoma:
- Age - Sex - Location - RS cells / CD? - Morphology |
- Age: 15-35
- Sex: M=F - Location: Mediastinal - RS cells / CD: CD15, CD30 (+) - Morphology: lacunar cells and dense sclerosis |
|
|
Mixed Cellularity Hodgkin Lymphoma:
- Age - Sex - Location - RS cells / CD? - Morphology |
- Age: bimodal (young and older adults)
- Sex: M>F - Location: cervical, axillary - RS cells / CD: CD15, CD30 (+) - Morphology: lots of inflammatory milieu |
|
|
Nodular Lymphocyte Predominant Hodgkin Lymphoma:
- Age - Sex - Location - RS cells / CD? - Morphology |
- Age: 30-50
- Sex: M>F - Location: Cervical, axillary - RS cells / CD: CD20, CD45 (+) - Morphology: popcorn cells, L&H cells |
|
|
Which type of Hodgkin Lymphoma has mediastinal masses?
|
Nodular Sclerosis
|
|
|
Which type of Hodgkin Lymphoma has cervical and axillary masses?
|
- Mixed cellularity
- Nodular lymphocyte predominant |
|
|
Which type of Hodgkin Lymphoma is CD15 and CD30 (+)?
|
- Nodular Sclerosis
- Mixed Cellularity |
|
|
Which type of Hodgkin Lymphoma is CD20 and CD45 (+)?
|
Nodular Lymphocyte Predominant
|
|
|
Which type of Hodgkin Lymphoma is characterized by lacunar cells and dense sclerosis?
|
Nodular Sclerosis
|
|
|
Which type of Hodgkin Lymphoma is characterized by lots of inflammatory milieu?
|
Mixed Cellularity
|
|
|
Which type of Hodgkin Lymphoma is characterized by popcorn cells and L&H cells?
|
Nodular Lymphocyte Predominant
|
|
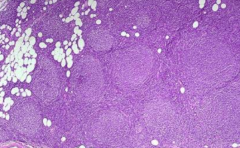
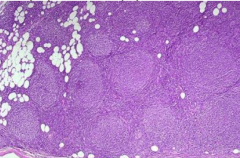
What is this?
|
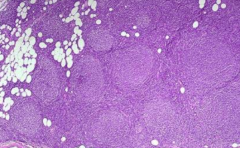
Follicular Lymphoma (or could be Hyperplasia)
|
|
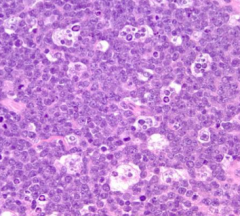
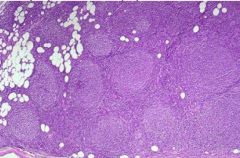
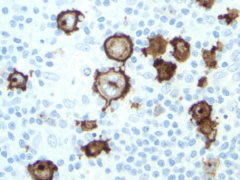
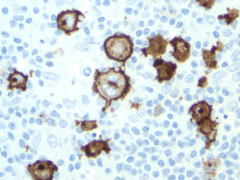
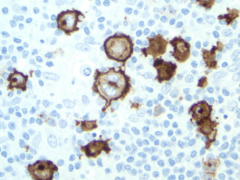
What is this?
|
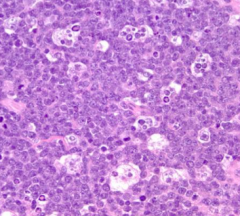
Burkitt Lymphoma ("starry sky")
|

