![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
144 Cards in this Set
- Front
- Back
|
Where do lymphocytes develop from?
|
- Bone marrow (B cells)
- Thymus (T cells) |
|
|
Where are mature lymphocytes located? How do they get there?
|
- Peripheral lymphoid tissues: lymph nodes, spleen, tonsils, adenoids, and Peyer's patches
- Home to these locations by cytokines and chemokines |
|
|
What are the most widely distributed and easily accessible lymphoid tissues?
|
Lymph nodes
|
|
|
What is the clinical significance of lymph nodes?
|
- They are frequently examined for diagnostic purposes
- Trivial injuries and infections induce subtle changes - Significant infections produce nodal enlargement and sometimes leave residual scarring |
|
|
What is the structure of lymph nodes?
|
- Discrete, encapsulated structures
- Contain well-organized B-cell and T-cell zones - Richly invested w/ phagocytes and APCs |
|
|
What morphological changes occur in lymph nodes after activation of the resident immune cells?
|
- Within several days, primary follicles enlarge and transform into pale-staining germinal centers; this allows B cells to make high-affinity Abs
- Paracortical T-cell zones undergo hyperplasia |
|
|
What are the types of Lymph Node inflammation?
|
Acute and Chronic Non-specific Lymphadenitis
|
|
|
What is the most common cause of acute lymphadenitis in the cervical region?
|
Microbial drainage from infections of the teeth or tonsils
|
|
|
What is the most common cause of acute lymphadenitis in the axillary or inguinal region?
|
Microbial drainage from infections in the extremities
|
|
|
What is the most common cause of acute lymphadenitis in the mesenteric region?
|
Acute appendicitis (also can be caused by other self-limited infections that can mimic acute appendicitis)
|
|
|
What is the most common cause of acute generalized lymphadenitis?
|
Systemic viral infections (particularly in children) and bacteremia
|
|
|
What is the morphological appearance of lymph nodes during acute non-specific lymphadenitis?
|
- Swollen and engorged
- Grey-red - Large, reactive germinal centers contain mitotic figures - Macrophages contain particulate debris from dead bacteria or necrotic cells - Pyogenic organisms cause centers of follicles to necrose and they may contain pus |
|
|
What happens to the lymphoid sinuses during acute non-specific lymphadenitis?
|
- Endothelial cells lining the sinuses undergo hyperplasia
- Scattered neutrophils infiltrate about the follicles and accumulate within the lymphoid sinuses |
|
|
What are the symptoms of Acute Non-specific Lymphadenitis?
|
- Nodes are enlarged and painful
- If abscess formation is extensive, the nodes become fluctuant - Overlying skin is red - Sometimes, suppurative infections penetrate through the capsule of node and track to skin to produce draining sinuses - Healing of these lesions may lead to scarring |
|
|
What happens if suppurative infections penetrate through the capsule of the node?
|
- They may track to the skin to produce draining sinuses
- Healing of these lesions may lead to scarring |
|
|
What are the types of Chronic Non-Specific Lymphadenitis?
|
- Follicular Hyperplasia
- Paracortical Hyperplasia - Reticular Hyperplasia (aka sinus histiocytosis) |
|
|
What is the morphological appearance of lymph nodes during chronic non-specific lymphadenitis with Follicular Hyperplasia?
|
- Large oblong germinal centers (secondary follicles) - contain dark zone and light zone
- Surrounded by collar of small resting naive B cells (mantle zone) |
|
|
What causes follicular hyperplasia in chronic non-specific lymphadenitis?
|
Stimuli that activate humoral immune responses
|
|
|
What is the appearance of germinal centers in Chronic Non-specific Lymphadenitis? What makes up these areas?
|
- Large and oblong
- Surrounded by collar of small resting naive B cells = mantle zone Polarized into two distinct regions: - Dark zone: contains blast-like B cells (centroblasts) - Light zone: contains B cells w/ irregular or cleaved nuclear contours (centrocytes) In between the germinal B centers is a network of antigen-presenting follicular dendritic cells and macrophages ("tingible-body macrophages") that contain nuclear debris of B cells |
|
|
Where are centroblasts found?
|
Proliferating blast-like B cells found in the dark zone of the germinal center (secondary follicle) of lymph nodes during Chronic Non-specific Lymphadenitis
|
|
|
Where are centrocytes found?
|
B cells with irregular or cleaved nuclear controus found in the light zone of the germinal center (secondary follicle) of lymph nodes during Chronic Non-specific Lymphadenitis
|
|
|
What is found between the germinal B centers in Chronic Non-specific Lymphadenitis? What are their characteristics?
|
- Network of antigen-presenting follicular dendritic cells and macrophages (referred to as "tingible-body" macrophages)
- Contain nuclear debris of B cells - undergo apoptosis if they fail to produce an antibody w/ a high affinity for antigen |
|
|
What happens to B cells that fail to produce antibody with a high affinity for antigen?
|
Undergo apoptosis, phagocytosed by follicular dendritic cells and "tingible-body" macrophages
|
|
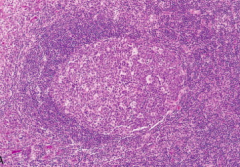
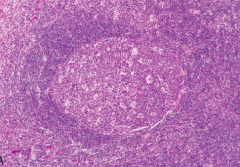
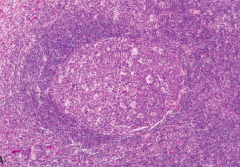
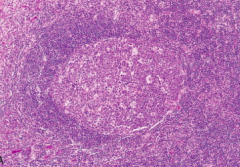
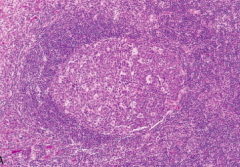
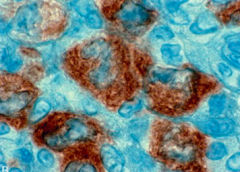
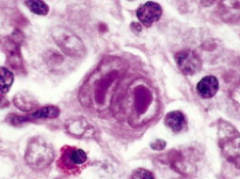
What does this image show?
|
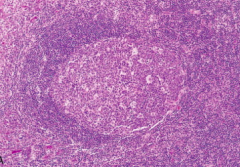
- Reactive follicle and surrounding mantle zone
- The dark-staining mantle zone is more prominent adjacent to the germinal-center light zone in the left half of the follicle - The right half of the follicle consists of the dark zone |
|
|
What are the causes of Follicular Hyperplasia in Chronic Non-Specific Lymphadenitis?
|
- Rheumatoid arthritis
- Toxoplasmosis - Early stages of infection w/ HIV |
|
|
What neoplasm is Follicular Hyperplasia similar to?
|
Follicular Lymphoma
|
|
|
What features favor a reactive (non-neoplastic) follicular hyperplasia?
|
- Preservation of the lymph node architecture (including interfollicular T-cell zones and sinusoids)
- Marked variation in shape and size of follicles - Presence of frequent mitotic figures, phagocytic macrophages, and recognizable light and dark zones (which are absent in neoplastic follicles) |
|
|
What is the morphological appearance of lymph nodes during chronic non-specific lymphadenitis with Paracortical Hyperplasia?
|
- T-cell regions contain immunoblasts, activated T cells 3-4x the size of resting lymphocytes, have round nuclei, open chromatin, several prominent nucleoli, and moderate pale cytoplasm
- May efface B cell follicles - Often hypertrophy of sinusoidal and vascular endothelial cells |
|
|
What causes Paracortical Hyperplasia?
|
Stimuli that trigger T-cell mediated immune responses (eg, acute viral infections like infectious mononucleosis)
|
|
|
What happens in Paracortical Hyperplasia?
|
- Immunoblasts expand
- Expanded T-cell zone may efface B-cell follicles - Hypertrophy of sinusoidal and vascular endothelial cells - Sometimes infiltrating macrophages and eosinophils |
|
|
What are immunoblasts? What do they look like? When do you see them?
|
- Activated T cells 3-4x the size of resting lymphocytes
- Round nuclei - Open chromatin - Several prominent nucleoli - Moderate pale cytoplasm - Found in paracortical hyperplasia in T-cell regions |
|
|
What needs to be done when immunoblasts are so numerous that they efface the B-cell follicles?
|
Need to do special studies to exclude a lymphoid neoplasm
|
|
|
What does Sinus Histiocytosis refer to?
|
- AKA reticular hyperplasia
- Increase in number and size of cells that line lymphatic sinusoids |
|
|
When is Sinus Histiocytosis more prominent?
|
In lymph nodes draining cancers such as carcinoma of the breast
|
|
|
What is the morphological appearance in Sinus Histiocytosis?
|
- Lining lymphatic endothelial cells are markedly hypertrophied
- Macrophages are greatly increased in numbers - Results in expansion and distension of sinuses |
|
|
What are the symptoms of Chronic Non-specific Lymphadenitis?
|
Lymph nodes are non-tender because nodal enlargement occurs slowly over time
|
|
|
Where is Chronic Non-specific Lymphadenitis common? Why?
|
- Inguinal and axillary nodes
- Drain relatively large areas of body (extremities) and are challenged frequently |
|
|
What is the difference between leukemias and lymphomas?
|
- Leukemia: neoplasms in bone marrow and peripheral blood
- Lymphoma: neoplasms that arise as discrete tissue masses (these terms reflect the usual tissue distribution of each disease at presentation) |
|
|
What are the sub-groups of lymphomas?
|
- Hodgkin Lymphoma
- Non-Hodgkin Lymphomas (NHLs) - Plasma Cell Neoplasms |
|
|
Where do Plasma Cell Neoplasms arise?
|
- Arise in BM
- Only infrequently involve the lymph nodes or the peripheral blood |
|
|
How common are Lymphomas?
|
100,000 new cases diagnosed in US/year
|
|
|
What is the typical clinical presentation of all Hodgkin lymphomas and 2/3 of non-Hodgkin lymphomas?
|
- Enlarged non-tender lymph nodes (often >2cm)
- Hodgkin's Lymphoma often associated w/ fever related to release of inflammatory cytokines |
|
|
What is the typical clinical presentation of the remaining 1/3 of non-Hodgkin lymphomas?
|
Symptoms related to the involvement of extra-nodal sites (eg, skin, stomach, or brain)
|
|
|
What is the typical clinical presentation of the lymphocytic leukemias?
|
Signs and symptoms related to the suppression of normal hematopoiesis by tumor cells in the bone marrow
|
|
|
What is the typical clinical presentation of Plasma Cell Neoplasms? Most common type?
|
- Multiple Myeloma
- Causes bony destruction of the skeleton and often presents with pain d/t pathological fractures - Some plasma cell neoplasms cause symptoms via secretion of circulating factors (Eg, whole antibodies or Ig fragments) |
|
|
What are the categories of Lymphoid Neoplasms?
|
- I: Precursor B-Cell Neoplasms
- II: Peripheral B-Cell Neoplasms - III: Precursor T-Cell Neoplasms - IV: Peripheral T-Cell and NK-Cell Neoplasms - V: Hodgkin Lymphoma |
|
|
What are the types of Class II Lymphoid Neoplasms?
|
Peripheral B-Cell Neoplasms:
- Lymphoplasmacytic Lymphoma - Splenic and Nodal Marginal Zone Lymphomas - Extra-Nodal Marginal Zone Lymphoma - Mantle Cell Lymphoma - Follicular Lymphoma - Marginal Zone Lymphoma - Diffuse Large B-cell Lymphoma - Burkitt Lymphoma |
|
|
What are the types of Class IV Lymphoid Neoplasms?
|
Peripheral T-Cell and NK-Cell Neoplasms:
- Peripheral T-Cell Lymphoma, un-specified - Anaplastic Large-Cell Lymphoma - Extra-nodal NK/T-Cell Lymphoma |
|
|
What are the types of Class V Hodgkin Lymphomas?
|
Classical Sub-types:
- Nodular sclerosis - Mixed cellularity - Lymphocyte-rich - Lymphocyte-depletion Lymphocyte predominance |
|
|
What is necessary for diagnosis of Lymphoid Neoplasia?
|
Histologic examination of lymph nodes or other involved tissues is required for diagnosis although it can be suspected based on clinical features
|
|
|
What are the features of all daughter cells derived from the malignant progenitor in lymphoid neoplasia? Why?
|
Monoclonal population of lymphocytes:
- All share the same antigen receptor gene configuration and sequence - All synthesize identical antigen receptor proteins (Igs or T-cell receptors) - Because antigen receptor gene rearrangement precedes transformation |
|
|
What are the features of daughter cells in normal immune responses (that distinguish them from daughter cells in lymphoid neoplasms)?
|
Polyclonal populations of lymphocytes that express many different antigen receptors
|
|
|
How can you distinguish lymphoid neoplasms from normal immune response cells?
|
- Analyze antigen receptor genes and their protein products
- Distinguish reactive (polyclonal) and malignant (monoclonal) lymphoid proliferations |
|
|
What is the basis of detecting if there are any residual malignant lymphoid cells after therapy?
|
Each antigen receptor gene rearrangement produces a unique DNA sequence that constitutes a highly specific clonal marker (analyze antigen receptor genes and protein products to check for residual malignant lymphoid cells after therapy)
|
|
|
What kind of cells cause lymphoid neoplasms?
|
- 85-90% are of B-cell origin
- Most of remainder are of T-cell origin - Rarely of NK-cell origin - Most lymphoid neoplasms resemble some recognizable stage of B- or T-cell differentiation |
|
|
What abnormalities are lymphoid neoplasms associated with? Implications?
|
Immune Abnormalities:
- Loss of protective immunity (susceptibility to infection) - Breakdown of tolerance (auto-immunity) - Individuals w/ inherited or acquired immunodeficiency are at risk of developing certain lymphoid neoplasms, particularly those caused by oncogenic viruses (eg, EBV) |
|
|
How do neoplastic B and T cells relate to normal B and T cells?
|
- Neoplastic B and T cells tend to mimic the behavior of their normal compartments
- Eg, they home to certain tissue sites, leading to characteristic patterns of involvement |
|
|
Where do follicular lymphomas occur?
|
Germinal centers of lymph nodes (B cells)
|
|
|
Where do cutaneous T cell lymphomas occur?
|
Skin
|
|
|
What governs the homing of the neoplastic lymphoid cells to certain areas of the body?
|
- Adhesion molecules and chemokine receptors help home cells to normal locations
- They can also recirculate through the lymphatics and peripheral blood to distant sites (as a result most are widely disseminated at time of diagnosis) |
|
|
Which types of lymphoid neoplasms are not as widely disseminated at time of diagnosis?
|
- Hodgkin Lymphomas: sometimes restricted to one group of lymph nodes
- Marginal Zone B-Cell Lymphomas: often restricted to sites of chronic inflammation |
|
|
How does Hodgkin Lymphoma spread? Vs. Non-Hodgkin Lymphoma? How does this affect staging information?
|
- HL: spreads in orderly fashion
- NHL: spread widely early in course in less predictable fashion - While lymphoma staging provides general prognostic information, it is more useful for Hodgkin lymphoma (d/t predictable spread) |
|
|
What are the neoplasms of Mature B Cells?
|
- Burkitt Lymphoma
- Diffuse Large B-Cell Lymphoma - Extra-Nodal Marginal Zone Lymphoma - Follicular Lymphoma - Mantle Cell Lymphoma |
|
|
Burkitt Lymphoma:
- Cell of origin - Genotype - Clinical features |
- Originates in germinal-center B cells
- t(8;14) - c-MYC and Ig loci - Some are EBV-associated - Affect adolescents or young adults with extranodal masses - Uncommonly presents as "leukemia" - Aggressive |
|
|
Diffuse Large B-Cell Lymphoma:
- Cell of origin - Genotype - Clinical features |
- Originates in germinal-center or post-germinal-center B cells
- Diverse chromosomal arrangements, most often BCL6 (30%), BCL2 (10%), or c-MYC (5%) - All ages affect, more commonly in adults - Appears as rapidly growing mass - 30% extra-nodal - Aggressive |
|
|
Extra-Nodal Marginal Zone Lymphoma:
- Cell of origin - Genotype - Clinical features |
- Originates in memory B cells
- t(11;18) - MALT1-IAP2 fusion gene - t(1;14) - BCL10-IgH fusion gene - t(14;18) - MALT1-IgH fusion gene - Arises at extra-nodal sites in adults w/ chronic inflammatory diseases - May remain localized - Indolent |
|
|
Follicular Lymphoma:
- Cell of origin - Genotype - Clinical features |
- Originates in germinal-center B cells
- t(14;18) creates BCL2-IgH fusion gene - Older adults with generalized lymphadenopathy - BM involvement - Indolent |
|
|
Mantle Cell Lymphoma:
- Cell of origin - Genotype - Clinical features |
- Originates in naive B cells
- t(11;14) creates CyclinD1-IgH fusion gene - Older males w/ disseminated disease - Moderately aggressive |
|
|
Which type of Lymphoma presents in adolescents or young adults with aggressive extra-nodal masses? Cell of origin? Genotype?
|
Burkitt Lymphoma
- Originates in germinal-center B cells - t(8;14) - c-MYC and Ig loci - Can be associated w/ EBV |
|
|
Which type of Lymphoma presents in all ages (especially adults) with aggressive, rapidly growing mass (30% extranodal)? Cell of origin? Genotype?
|
Diffuse Large B-Cell Lymphoma
- Originates in germinal-center B cells or post-germinal-center B cells - Diverse chromosomal rearrangements, most often BCL6 (30%), BCL2 (10%), or c-MYC (5%) |
|
|
Which type of Lymphoma presents with indolent, localized, extra-nodal lesions in adults with chronic inflammatory diseases? Cell of origin? Genotype?
|
Extra-Nodal Marginal Zone Lymphoma:
- Originates in memory B cells - t(11;18) - MALT1-IAP2 fusion gene - t(1;14) - BCL10-IgH fusion gene - t(14;18) - MALT1-IgH fusion gene |
|
|
Which type of Lymphoma presents with indolent, generalized lymphadenopathy in older adults and involves the BM? Cell of origin? Genotype?
|
Follicular Lymphoma
- Originates in germinal-center B cells - t(14;18) creates BCL2-IgH fusion gene |
|
|
Which type of Lymphoma presents with moderately aggressive, disseminated disease in older males? Cell of origin? Genotype?
|
Mantle Cell Lymphoma
- Originates in naive B cells - t(11;14) creates CyclinD1-IgH fusion gene |
|
|
What are the neoplasms of Mature T or NK Cells?
|
- Peripheral T-Cell Lymphoma, Unspecified
- Anaplastic Large-Cell Lymphoma - Extranodal NK/T-Cell Lymphoma |
|
|
Peripheral T-Cell Lymphoma, Unspecified:
- Cell of origin - Genotype - Clinical features |
- Originates in Helper or Cytotoxic T cells
- No specific chromosomal abnormality - Mainly older adults - Usually presents w/ lymphadenopathy - Aggressive |
|
|
Anaplastic Large-Cell Lymphoma:
- Cell of origin - Genotype - Clinical features |
- Originates in cytotoxic T cells
- Rearrangements of ALK - Children and young adults - Usually with lymph node and soft-tissue disease - Aggressive |
|
|
Which type of Lymphoma presents with aggressive lymphadenopathy mainly in older adults? Cell of origin? Genotype?
|
Peripheral T-Cell Lymphoma, Unspecified:
- Originates in Helper or Cytotoxic T cells - No specific chromosomal abnormality |
|
|
Which type of Lymphoma presents with aggressive lymph node and soft tissue disease in children and young adults? Cell of origin? Genotype?
|
Anaplastic Large-Cell Lymphoma
- Originates in cytotoxic T cells - Rearrangements of ALK |
|
|
Extra-Nodal NK/T-Cell Lymphoma:
- Cell of origin - Genotype - Clinical features |
- Originates in NK cells (common) or Cytotoxic T cells (rare)
- EBV associated - No specific chromosomal abnormality - Adults with destructive extranodal masses - Most commonly sinunasal - Aggressive |
|
|
Which type of Lymphoma presents in adults with destructive, aggressive extra-nodal masses, most commonly sinonasal? Cell of origin? Genotype?
|
Extranodal NK/T-Cell Lymphoma
- Originates in NK cells (common) or Cytotoxic T cells (rare) - EBV associated - No specific chromosomal abnormality |
|
|
What is the most common form of indolent Non-Hodgkin Lymphoma in US?
|
Follicular Lymphoma
|
|
|
What kind of cells does Follicular Lymphoma arise from? What do they express on their surface?
|
- Germinal center B cells
- Express CD19, CD20, and CD10 |
|
|
What genetic abnormality is Follicular Lymphoma associated with? Implications?
|
- t(14;18) creating BCL2-IgH fusion gene
- Leads to over-expression of BCL2 - BCL2 antagonizes apoptosis and promotes survival of follicular lymphoma cells - Normally, germinal centers contain numerous B cells undergoing apoptosis, therefore this is bad |
|
|
What are the morphological characteristics of Follicular Lymphoma?
|
- Centrocytes and centroblasts are predominant cell types
- Centrocytes (irregular w/ cleaved nuclear contours) predominate - BM involvement in 85% of cases, takes form of paratrabecular lymphoid aggregates |
|
|
What are the symptoms of Follicular Lymphoma? Treatment prognosis?
|
- Indolent course
- Incurable - Median survival 7-9 years (not improved by aggressive therapy) |
|
|
How do you treat Follicular Lymphoma?
|
- Low-dose chemotherapy or immunotherapy (eg, anti-CD20 antibody) when they become symptomatic
- Usually is an indolent disease and therapy does not improve survival time |
|
|
What is the most common form of Non-Hodgkin Lymphoma in US?
|
Diffuse Large B-Cell Lymphoma (DLBCL)
|
|
|
What are the morphological characteristics of Diffuse Large B-Cell Lymphoma (DLBCL)?
|
- Large cell size (4-5x diameter of small lymphocyte)
- Open chromatin and prominent nucleoli - Diffuse pattern of growth |
|
|
What are the clinical features / prognosis of Diffuse Large B-Cell Lymphoma (DLBCL)?
|
- Rapidly enlarging mass at nodal or extra-nodal site (can arise anywhere in body)
- Aggressive tumors - Fatal without treatment |
|
|
What are the types of Burkitt Lymphomas?
|
- African (endemic) Burkitt Lymphoma
- Sporadic (non-endemic) Burkitt Lymphoma - Subset of aggressive lymphomas occurring in individuals infected w/ HIV |
|
|
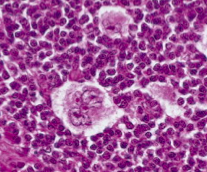
What are the morphological characteristics of Burkitt Lymphoma?
|
- Diffuse infiltrate of intermediate-sized lymphoid cells
- High mitotic index - Contains numerous apoptotic cells * Starry sky pattern d/t macrophages being surrounded by abundant clear cytoplasm |
|
|
What kind of cells are affected by Burkitt Lymphoma? What surface markers do they have?
|
- Mature germinal center B cells
- Express IgM, CD19, CD20, CD10, and BCL6 * Almost always fail to express anti-apoptotic protein BCL2 |
|
|
What is the genetic abnormality in Burkitt Lymphoma? Implications?
|
- Translocations of the c-MYC gene on chromosome 8
- Usually with IgH locus, t(8;14) - May also be t(2;8) with Igκ of t(8;22) with γ ligh chain loci - These translocations all drive c-MYC (oncogene) expression |
|
|
What is a feature of essentially all endemic Burkitt Lymphomas, 25% of HIV-associated Burkitt Lymphomas, and 15-20% of sporadic cases of Burkitt Lymphoma?
|
Latent infections with EBV
|
|
|
How common are latent infections of EBV in the types of Burkitt Lymphoma?
|
- ~100% of endemic tumors
- ~25% of HIV-associated tumors - ~15-20% of sporadic tumors |
|
|
Who is affected by Burkitt Lymphoma?
|
Children or young adults
|
|
|
How does endemic Burkitt Lymphoma present?
|
- Mass involving the mandible
- Shows unusual predilection for involvement of abdominal viscera, particularly the kidneys, ovaries, and adrenal glands - BM and PB involvement is uncommon - Very aggressive but responds well to chemotherapy |
|
|
How does sporadic Burkitt Lymphoma present?
|
- Most often appears as a mass involving the ileocecum and peritoneum
- BM and PB involvement is uncommon - Very aggressive but responds well to chemotherapy |
|
|
What happens to the neoplastic cells in Lymphplasmacytic Lymphoma?
|
- Undergo differentiation to plasma cells
- Secrete monoclonal IgM, often in amounts to cause a hyperviscosity syndrome known as Waldenström macroglobulinemia |
|
|
What type of lymphoma is associated with Waldenström macroglobulinemia? What happens in this?
|
- Lymphoplasmactic Lymphoma
- Differentiate into plasma cells that secrete monoclonal IgM that causes a hyperviscosity syndrome |
|
|
What is the morphological presentation of Lymphoplasmactic Lymphoma?
|
Marrow contains diffuse sparse-to-heavy infiltrate of lymphocytes, plasma cells, and plasmacytoid lymphocytes in varying proportions
|
|
|
How do you treat Lymphoplasmactic Lymphoma?
|
Plasmapheresis to alleviate the hyperviscosity and hemolysis caused by the high IgM levels
|
|
|
What kind of lymphoma has tumor cells that resemble the normal mantle zone B cells that surround germinal centers?
|
Mantle Cell Lymphoma
|
|
|
What are the morphological features of Mantle Cell Lymphoma?
|
- Majority have generalized lymphadenopathy filled with cells that resemble the normal mantle zone B cells that surround germinal centers
- 20-40% have peripheral blood involvement |
|
|
What is the genetic abnormality in Mantle Cell Lymphoma? Implications?
|
- t(11;14) involves IgH locus (14) and CyclinD1 locus (11)
- Causes CyclinD1 over-expression - Promotes G1- to S-phase progression during cell cycle |
|
|
What do the naive B cells express in Mantle Cell Lymphoma?
|
- CD19
- CD20 - Moderately high levels of surface Ig (usually IgM and IgD w/ κ or γ light chain) - Usually CD5+ and CD23- (which helps distinguish it from CLL/SLL |
|
|
How can you distinguish Mantle Cell Lymphoma from CLL/SLL?
|
Mantle Cell Lymphoma is CD5+ and CD23-
|
|
|
What is the prognosis for Mantle Cell Lymphoma?
|
Poor - median survival is only 3-4 years
|
|
|
Where do Marginal Zone Lymphomas arise?
|
- Lymph nodes
- Spleen - Other extra-nodal tissues (MALT) |
|
|
What kind of cells are affected in Marginal Zone Lymphoma?
|
Memory B-cells that often show evidence of somatic hyper-mutation
|
|
|
What did Marginal Zone Lymphomas at extra-nodal sites used to be called?
|
Maltomas (mucosa-associated lymphoid tumors)
|
|
|
What are the features of Marginal Zone Lymphomas at extra-nodal sites?
|
- Often arise within tissues involved by chronic inflammatory disorders of auto-immune or infectious etiology (eg, salivary glands in Sjögren disease, thyroid gland in Hashimoto thyroiditis, and stomach in Helicobacter gastritis)
- Remain localized for prolonged periods - May regress if inciting agent (eg, H. pylori) is eradicated |
|
|
Which type of lymphomas often arise within tissues involved by chronic inflammatory disorders of auto-immune or infectious etiology (eg, salivary glands in Sjögren disease, thyroid gland in Hashimoto thyroiditis, and stomach in Helicobacter gastritis)?
|
Marginal Zone Lymphomas
|
|
|
Which type of lymphomas are more common in Asia / Far East as opposed to US and Europe?
|
- Peripheral T-cell tumors: 5-10% of NHLs in US and Europe, but more common in Asia
- NK cell tumors: rare in West but more common in Far East |
|
|
What do Peripheral T-Cell Lymphoma, Unspecified do to lymph nodes? Types of cells?
|
- Efface lymph nodes diffusely
- Typically composed of pleomorphic mixture of variably sized malignant, mature T cells |
|
|
How do patients with Peripheral T-Cell Lymphoma, Unspecified present?
|
- Generalized lymphadenopathy
- Sometimes eosinophilia, pruritus, fever, and weight loss |
|
|
What is the prognosis of Peripheral T-Cell Lymphoma, Unspecified?
|
Significantly worse prognosis than comparably aggressive mature B-cell neoplasms
|
|
|
What genetic abnormality is associated with Anaplastic Large-Cell Lymphoma? Implications?
|
Rearrangements in ALK gene on chromosome 2p23
- Breaks the ALK locus and leads to formation of chimeric genes - Encode ALK fusion proteins, constitutively active tyrosine kinases, which trigger a number of signaling pathways including JAK/STAT pathway |
|
|
What are the morphological characteristics of Anaplastic Large-Cell Lymphoma?
|
- Large anaplastic cells
- Some contain hallmark cells (horse-shoe shaped nuclei and voluminous cytoplasm) |
|
|
Who is usually affected by Anaplastic Large-Cell Lymphoma? Prognosis?
|
- Children or young adults
- Very good prognosis (unlike other aggressive peripheral T cell neoplasms) |
|
|
What kind of lymphoma presents most commonly as a destructive nasopharyngeal mass?
|
Extra-Nodal NK/T-Cell Lymphoma
|
|
|
What is the most common presentation of Extra-Nodal NK/T-Cell Lymphoma?
|
- Destructive nasopharyngeal mass
- Leads to extensive ischemic necrosis |
|
|
What is Extra-Nodal NK/T-Cell Lymphoma associated with?
|
EBV
|
|
|
What is the prognosis of Extra-Nodal NK/T-Cell Lymphoma?
|
- Highly aggressive neoplasm, responds well to radiation but not to chemotherapy
- Poor prognosis in advanced disease |
|
Which type of lymphomas are characterized by the presence of a tumor giant cell, the Reed-Sternberg Cell?
|
Hodgkin Lymphoma
|
|
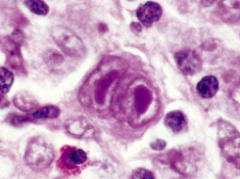
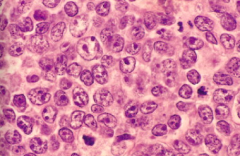
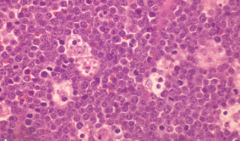
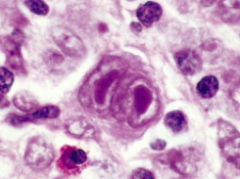
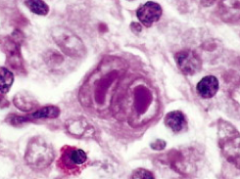
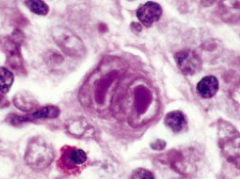
What kind of cell is this? What is it characteristic of?
|
- Reed-Sternberg (RS) Cell
- Characteristic of Hodgkin Lymphoma |
|
|
What is the distribution of cancer cells in Hodgkin Lymphoma?
|
Typically spreads in a step-wise fashion to anatomically contiguous nodes
|
|
|
What is the origin of cells affected by Hodgkin Lymphoma?
|
B cell origin
|
|
|
What are the morphological characteristics of Hodgkin Lymphoma? What cell surface markers do they have?
|
Reed-Sternberg (RS) cells (owl eye appearance) - express CD15 and CD30 (but not CD45)
|
|
|
What is the most common form of Hodgkin Lymphoma?
|
Nodular Sclerosis Hodgkin Lymphoma
|
|
|
What lymph nodes are most commonly affected by Nodular Sclerosis Hodgkin Lymphoma? Who gets it? Prognosis?
|
- Lower cervical, supraclavicular, and mediastinal lymph nodes
- Most are adolescents or young adults - Excellent prognosis |
|
|
What are the cellular characteristics of Nodular Sclerosis Hodgkin Lymphoma?
|
Presence of a variant of the Reed-Sternberg cells - Lacunar Cells (single multi-lobate nucleus that lies in empty space where cytoplasm tore away = lacunae)
|
|
|
What are the morphological characteristics of Nodular Sclerosis Hodgkin Lymphoma?
|
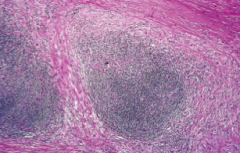
Collagen bands that divide the lymphoid tissue into nodules
|
|
|
What is the most common type of Hodgkin Lymphoma in patients over 50 years of age (25% overall)?
|
Mixed-Cellularity Hodgkin Lymphoma
|
|
|
Which type of Hodgkin Lymphoma expresses B cell markers (CD20) but usually fails to express CD15 and CD30?
|
Lymphocyte-Predominance Hodgkin Lymphoma
|
|
|
What are the clinical differences between Hodgkin and Non-Hodgkin Lymphomas in regards to the location?
|
- HL: more often localized to a single axial group of nodes (cervical, mediastinal, para-aortic)
- NHL: more frequent involvement of multiple peripheral nodes |
|
|
What are the clinical differences between Hodgkin and Non-Hodgkin Lymphomas in regards to the spread?
|
- HL: orderly spread by contiguity
- NHL: Non-contiguous spread |
|
|
What are the clinical differences between Hodgkin and Non-Hodgkin Lymphomas in regards to the Mesenteric nodes and Waldeyer ring?
|
- HL: rarely involved
- NHL: commonly involved |
|
|
What are the clinical differences between Hodgkin and Non-Hodgkin Lymphomas in regards to extranodal involvement?
|
- HL: uncommon
- NHL: common |
|
|
How do you stage Hodgkin and Non-Hodgkin Lymphoma?
|
- I: Involvement of a single lymph node region (I) or involvement of a single extralymphatic organ or tissue (IE)
- II: Involvement of two or more lymph node regions on the same side of the diaphragm alone (II) or with involvement of limited contiguous extralymphatic organs or tissue (IIE) - III: Involvement of lymph node regions on both sides of the diaphragm (III), which may include the spleen (IIIS), limited contiguous extralymphatic organ or site (IIIE), or both (IIIES) - IV: Multiple or disseminated foci of involvement of one or more extralymphatic organs or tissues with or without lymphatic involvement |
|
|
What are the characteristics of stage I Hodgkin and Non-Hodgkin Lymphoma?
|
Involvement of a single lymph node region (I) or involvement of a single extralymphatic organ or tissue (IE)
|
|
|
What are the characteristics of stage II Hodgkin and Non-Hodgkin Lymphoma?
|
Involvement of two or more lymph node regions on the same side of the diaphragm alone (II) or with involvement of limited contiguous extralymphatic organs or tissue (IIE)
|
|
|
What are the characteristics of stage III Hodgkin and Non-Hodgkin Lymphoma?
|
Involvement of lymph node regions on both sides of the diaphragm (III), which may include the spleen (IIIS), limited contiguous extralymphatic organ or site (IIIE), or both (IIIES)
|
|
|
What are the characteristics of stage IV Hodgkin and Non-Hodgkin Lymphoma?
|
Multiple or disseminated foci of involvement of one or more extralymphatic organs or tissues with or without lymphatic involvement
|

