![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
21 Cards in this Set
- Front
- Back
|
What is the most common cause of liver disease worldwide?
What is the demographic is more affected why? |
Alcoholic Liver Disease
Women more susceptible at lower doses of EtOH. (also HCV, obesity, and hemochromatosis). Thought that estrogen ↑ activation of inflammatory response in liver. |
|
|
Describe the spectrum of alcoholic liver disease.
What lab abnormalities might you see in ALD? |
Benign fatty liver changes (no liver dysfunction, normal enzymes) --> Acute Alcoholic Hepatitis (encephalopathy, coagulopathy, etc.) --> Chronic disease/ Cirrhosis --> Liver cancer
Labs: ↑ AST >>ALT, ↑ GGT, low albumin, ↑ PT/INR, metabolic abnormalities (↑ insulin), Low electrolytes, pt might have high WBC (from hepatitis), anemia |
|
|
What is the etiology of Oriental flush syndrome?
What is the treatment for ALD? |
Some asians have deficient Aldehyde Dehydrogenase, Acetaldehyde builds up (causes n/v, flushing, systemic effects). ETOH --> Acetaldehyde --> Acetate. (Glutathione depletion can also do this)
Rx = Abstinence, Steroids (severe hepatitis), nutrition supplementation, Liver transplant (6mo. abstinence) |
|
|
Describe the pathogenesis of Alcoholic Liver Injury.
|
1. EtOH ↑ gut permeability, so endotoxins and LPS can enter portal circulation and liver --> activate Kupffer cells --> proinflammatory cytokines released
2. Byproducts of aldehyde also serve as antigens and ↑ immune response 3. Stellate cell respond to injury by producing fibrosis/collagen --> cirrhosis |
|
|
What is the clinical sepctrum of NAFLD (nonalcoholic fatty liver disease)?
What is thought to be the cause of the increase in NAFLD in this country? |
1. Simple steatosis
2. Steatohepatitis (NASH) - steatosis, inflammation of lobules, ballooning and degeneration, Mallory body, fibrosis 3. Cirrhosis Associated with increase in obesity, insulin resistance, T2DM, Metabolic syndrome |
|
|
How do you diagnose NASH?
What are some symptoms and signs of it? |
Non-alcoholic Steatohepatitis: ↑ AST, AST (ALT>AST), ↑ Alk Phos. Must have presence of associated diseases (T2DM, obesity, etc.) and non-alcoholic. BIOPSY shows classic finding.
Signs = mostly asymptomatic, sometimes RUQ pain. Hepatomegaly. Acanthosis nigricans (sign of inuslin resistance) |
|
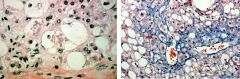
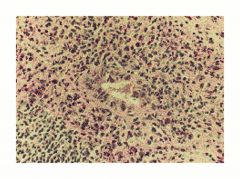
What does the biopsy here show?
What is the model for the development of this condition? |
NASH- note the ballooning degeneration of cells, Mallory hyaline (made up of keratin filaments). On right trichrome stain- you see chicken wire fibrosis.
2 Hit hypothesis: Obesity, T2DM --> Insulin resistance (1st hit) --> FFA accumulation, steatosis--> Oxidative stress/lipid peroxidation (2nd hit) --> cell damage and cytokine production --> stellate cell activation (fibrosis) |
|
|
What treatment is recommended for NASH?
|
Treat the associated conditions (lose weight, control diabetes and metabolic problems).
Unfortunately no approved drugs. But LIFESTYLE change can reverse condition! |
|
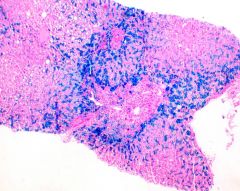
This is a liver stained with Prussian Blue. What disease is shown here?
What is the inheritance, and what demographic is affected? |
Hereditary Hemochromatosis (note the Fe deposition in the liver).
AR disorder, very common (1:250) especially Northern Europeans. |
|
|
What is the genetic etiology of Hereditary Hemochromatosis?
Describe the pathogenesis and what the classic presentation is. |
C282Y homozygote, or a compound heterozygote. For HFE gene (sensor protein, senses iron level.
Pathogenesis- typically HFE senses Fe level and prevents absorption of Fe in body (by ↑ hepcidin). Here there is a false impression of low stores, so Hepcidin is ↓, and Fe is continually absorbed. Deposits in liver and other tissue. |
|
|
What age and gender are typically more affected? Why?
What are some sxs of HH? |
Older age (>40) - because it takes a while for Fe to accumulate and produce symptoms
M> F (female protected by menstrual blood loss). Sxs= organ system dependent (arthritis, bronze diabetes, impotence, cirrhosis, HCC). |
|
|
What is the treatment of HFE-related HH?
If someone with a C282Y Homozygous genome, and elevated TS (transferrin saturation) also is shown to have ↑ ALT, AST and Ferratin, what would you do? |
Weekly phlebotomy (till ferratin levels are lowered).
Get Liver biopsy (to rule out liver injury). |
|
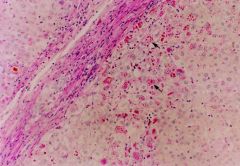
This is a biopsy of a liver stained with A1AT. Describe the pathogenesis of this condition and what two major organs it affects.
|
a1AT deficiency --> a glycoprtein that inhibits neutrophil elastase.
In liver: gain of toxic function causes retention of molecule in the ER of hepatocytes. In lung: causes emphysema- loss of a1AT permits proteolytic damage to CT matrix. *no treatment other than liver transplant |
|

What is the inheritance pattern of this individual's condition?
What symptoms might this person exhibit? |
Wilson disease- note the Kayser- Fleischer Rings (copper deposits in outer cornea)
AR, from accumulation of Cu in brain, liver. Symptoms seen before 30 yrs, typically neurpsych (tremor, personality change, depression, cirrhosis, hepatitis, etc.) |
|
|
What is the pathogenesis of Wilson's disease?
How would you diagnose it? |
ATP7B mutation (it's a protein that facilitates Cu2+ binding to Ceruloplasmin which excretes it into bile).
CP, when not bound to Cu, is rapidly degraded. Diagnose via testing for CP levels (should be low). Follow up with 24 hr urine Cu (elevated). |
|
What histologic findings would you expect to see in Autoimmune Hepatitis?
What is the clinical presentation of patients? How is it treated? |
Lymphocyte & plasma infiltrate in liver --> loss of tolerance --> destroy hepatocytes and induce inflammation
Typically female, may have other AI disease (Sjogren, RA, Hashimoto, etc.), Can be asymptomatic or have acute disease or cirrhosis. Have elevated serologic markers & antibodies. Treat with Predinosine and Azathioprine. |
|
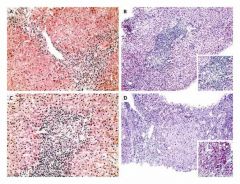
What type of liver disease is shown here?
What are some common presenting features? |
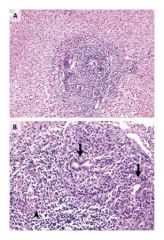
Primary Biliary Cirrhosis (immune mediated destruction of Intrahepatic bile ducts) --> fibrosis and cirrhosis. *pathology: florid ductal lesion
Mostly women, coexisting AI conditions. Can be asymptomatic, or have fatigue, pruritis, and portal hypertension. |
|
|
What is thought to be the pathogenesis of Primary Biliary Cirrhosis?
What is the treatment? |
Antimitochondrial antibodies (AMA) against proteins on biliary eptihelial cells. Can cause destruction of bile duct.
Treatment = UCDA = ursodeoxycholic acid (cytoprotective effect on bile duct cells, against toxic bile acids). Antipruritic agents (relieve itching, antihistamines). Treat osteoporosis. |
|

Name the above extraintestinal manifestations of IBD.
|
L--> R
Pyoderma gangrenosum, Erythema nodosum, Ankylosing Spondilitis Bottom: Uveitis, Aphthous ulcer, Primary Sclerosing Collangitis |
|
|
What is the pathogenesis of PSC? What is the gold standard for diagnosing this condition?
|
Unknown, chronic biliary disease which is associated with IBD (especially UC). Inflammation of intra and extrahepatic bile ducts --> cirrhosis.
Patients are positive for p-ANCA. Strong association with HLA types. Gold standard = ERCP or MRCP (look for dilation and stricture) |
|
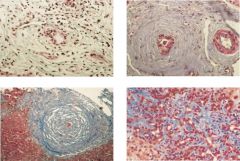
What condition is shown on the biopsy?
What is the treatment? |
Onion skin fibrosis around bile ducts in the liver (seen in PSC).
Treatment = antibiotics (during cholangitis), liver transplant = only curative therapy. ↑ risk of developing cholangiocarcinoma. |

