![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
82 Cards in this Set
- Front
- Back
|
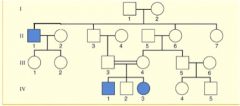
What type of pedegree?
|
autosomal recessive
|
|
|
How do you know if pedigree is showing autosomal dominant?
|
a. Trait expected in every generation
b. Affected offspring has one affected parent c. Unaffected individuals don't transmit d. Both sexes can transmit to both sexes |
|
|
How do you know if pedigree is showing Autosomal recessive?
|
a. Most affected individuals have normal parents
b. on average 1/4 siblings affected c. occurrence is more likely with consanguinity |
|
|
How do you know if pedigree is showing X-linked recessive?
|
a. unaffected males do not transmit the trait
b. All daughters of affected males are heterozygous carriers c. Female carriers transmit affected allele to 50% of offspring (sons and daughters) |
|

which pedigree does this show?
|
auto dominant
|
|
Which pedigree does this show?
|
Autosomal recessive
|
|
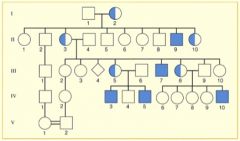
What pedegree is shown?
|
x-linked recessive
|
|
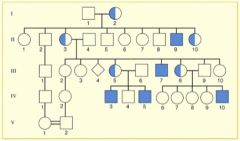
What type of pedigree is this?
|
x-linked recessive
|
|
|
Define the following terms about genetics...
1. Penetrance 2. Variable expressivity |
1. not all individuals who have genotype express it
2. individuals with the genotype express phenotype of gene different |
|
|
What is the difference between disorders caused by single genes and multiple ones?
|
Single genes can be mathematically calculated through punnet squares or HW, but with multiple factors it has to be done by shear numbers (1/200)
|
|
|
Define the following terms about genetics...
a. Liability b. Risk |
a. person's genetic predisposition to a disorder, but still needs an enviromental factor to cause it to occur
b. Risk is measured by how many "bad" genes that tend to show the disorder |
|
|
Define the following terms about genetics...
a. Threshold model of expression |
a. idea that the more genes you have compared to the rest of the population... the higher risk you go over the "threshhold" level that will make the disorder occur
|
|
|
Define the following terms about genetics
a. random drift b. founder effect |
a. random fluctuations in allele frequencies from generation to generations in a small population (A--> B, and no C's in small group, so C could easily die out)
b. Founder- small subgroup of a large population can trace a disease to first people in a certain area. Mutations stayed within group due to reproducing within small community |
|
|
Define the following terms about genetics...
a. active selection b. passive selection |
a. Group of people purposely choose specific mates and keep genes in population
b. survival advantages are found in small group of people living similarly for long time |
|
|
Define the following terms about genetics
a. multifactorial inheritances b. Consanguinity's role in multifactorial genetic disorders |
a. genes are independently inherited but not independently expressed (hair, skin color)... depends on environment and how many copies of however many genes carrying
b. Amount of blood relateness of offspring. The closer the related the more likely to have received some of the at risk genes |
|
|
What role does gender have in multifactorial inheritance?
What would you say about risk threshold of females if they were affected less? |
Sometimes it takes less at risks genes to be expressed on a male vs. female
risk threshold would be higher or more to the right on the graph. However they will transmit the condition and affect men |
|
|
Which mult. factor inheritance is more prevalent in men?
What two disorders are women more likely to get than men... ratio? |
5:1 Pyloric Stenosis, at risk of narrowing of stomach
Anencephaly- 1:2 male to female, when child has top neural tube forming spinal cord and brain dont develop in embryogenesis Spina Bifida (3:4) m:f failure of neural tube to close at lower place |
|
|
Give an example of risk and severity...
|
The more genes person has with the disorder, the worse the disorder...
Cleft lip- unilateral- subsequent siblings is 2.5%, but if bilateral lip and palate- subsequent siblings is 6.5% |
|
|
As a physician why would HW be used?
What are the HW equations? |
If heredity does not follow, it allows studies to figure out where or how disorder occured
p + q = 1 P2 + 2pq + Q2 =1 |
|
|
HW problem: Galactosemia (AR) resulting from mutations in GALT gene occur at a frequency of 1:10,000. What is the frequency of carriers?
|
q2= .0001
q=.01 p+.01=1 p=.99 2(.99)(.01)= .0198= 1/50 or 2% |
|
|
What is the basic five steps to cancer development?
|
1. Normal cell
2. Increased growth 3. Increased changes 4. Benign tumor 5. Metastatsis occurs |
|
|
What is an oncogene?
|
protein kinases that control proteins by phosphorylation which allows them to completely take over cell growth, differentiation, and translocation
|
|
|
What is the role of the following genes?
a. APC- b. RAS c. DCC d. TP53 e. PRL53 |
a. loss leads to increased growth (early tumor supressor)
b. Mutation leads to intermediate stage adenoma c. Loss leads to late stage adenoma d. loss leads to carcinoma e. if overexpressed it leads to metastasis |
|
|
What are three types of cancer resulting from translocation and what gene is translocated?
|
1. Burkitt Lymphoma- c-MYC translocated to immunoglobulin gene
2. Carcinoma of Lung, breast, cervix- c-MYC is not neccesarily translocated but is amplified 3. CML (chronic myelogenous leukemia)- c-ABL translocated to BCR locus |
|
|
What cancers result from these translocations?
a. c-MYC- amplification b. c-ABL translocated to BCR locus c. c-MYC translocated to immunoglobulin gene |
a. Carcinoma of the lung, breast, cervix
b. CML c. Burkitt Lymphoma |
|
|
What does loss of heterozygosity mean in development of mutations leading to cancer?
|
It causes cell to become homozygous for the mutated gene and therefore express the cancer gene.
|
|
|
How does loss of heterozygosity occur (5 examples)?
|
a. non-disjunction and loss of Ch. 13
b. Mitotic recombination c. Ch13q14 deletion: (Aa -->A- d. Gene inactivation e. Point mutation or small deletion: (Aa-->AA) |
|
|
What is the clinical presentation of retinoblastoma?
|
a. no family history
b. no pain c. Bilateral most cases d. Strabismus- eye tumor e. cross eyed f. leukocoria- yellow glow |
|
|
What are the heritable vs nonheritable comparisons of Rb?
|
1. Heritable
a. Bilateral b. early onset c. 20% family history d. multiple primary tumors risked e. multiple tumors else where likely f. Evidence of auto dom 2.Non- Heritable a. unilateral b. late onset (2 years) c. no family hx d. No increased risk of secondary primary tumors |
|
|
What is the gene involved in Familial adenomatous polyposis, Hereditary nonpolyposis colorectal cancer, and Retinoblastoma? (Say one thing about each)
|
a. FAP- gene is APC- tumor suppressor gene presents many polyps
b. HNPCC- gene is HNPCC no polyps c. Rb- gene is Rb-1 eye tumors |
|
|
How is the Rb-1 inherited?
What is the difference between FAP and HNPCC |
as dominant but expressed as recessive
FAP vs. HNPCC- FAP- shows more polyps at young age genetically dominant, has APC tumor supressor gene mutated, has a benign marker at CHRPE HNPCC- no polyps, later onset, look for MMR (mismatch repair) MSH2, MLH1 due to 60% of CRC having those genes... dominantly genetic |
|
|
What is the following techniques of genetics for...
1. Southern Blotting 2. Northern Blotting 3. Western Blotting |
1. reading DNA
2. reading RNA 3. reading Proteins |
|
|
What is the role of p53 in the cell cycle and what are some clinical consequences of mutations to this gene?
|
a. tumor suppressor gene that regulates the cell cycle
b. "known as guardian of genome" c. activated DNA repair, can hold cell cycle at G1/S point d. Also initiates apoptosis if problems are not fixed If mutated and loses function all hell breaks loose |
|
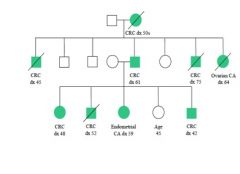
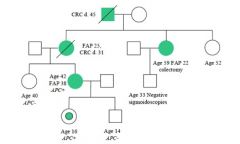
What is this tree showing?
|
HNPCC
|
|
|
What is this picture showing?
|
FAP
|
|
What is this picture showing?
|
FAP
|
|
what was this picture showing?
|
FAP
|
|
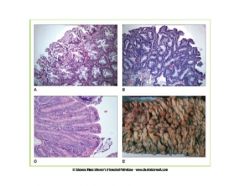
What is this picture showing and what does it have to do with cancer?
|
It is hypertrophy of the retinal pigment epithelium in CHRPE a benign marker of FAP
|
|
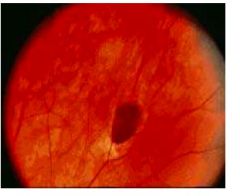
What is this family history of and what mutated gene causes this?
|
FAP the gene is APC
|
|
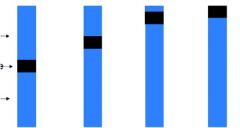
What are the pointers pointing to? Also type would you call each chromosome?
|
Pointers are pointing to P (above) centromere (black line in middle) Q (below) and from left to right (metacentric, submetacentric, acrocentric, and telocentric)
|
|

What is this type of translation? Where does it occur (which chromosomes) and what does it often lead to?
|
Robertsonian translocation- fusion of Q arms of acrocentric chromosome
usually involves 13,14,15, 21, 22 could lead to trisomy |
|

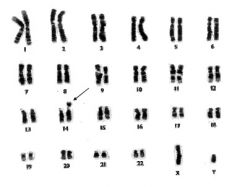
What cancer is forming here?
|
Chronic Myelogenous leukemia (CML)
|
|
|
What is a robertsonian translation and what does it lead to?
|
Fusion of Q arms of acrocentric chromosomes, usually 13,14,15,21,22 often leads to trisomies
|
|
|
What is cause of CML? What is translocation called?
|
translocation between chromosome 9 and 22 --> t(9;22) (q34;q11)
Called philadelphia chromosome |
|
|
What two genes fuse to form CML?
What gene does CD2 regulate? |
BCR-ABL
ABL |
|
|
What kind of tumor is associated with B-lymphocytes and produces antibodies?
|
Burkitt Lymphoma
|
|
|
What causes Burkitts Lymphoma?
Which genes are translocated |
Reciprical translocation t(8;14) (q24;32)
c-MYC from 8 to 14 leads to uncontrolled mitosis |
|
|
What cancer is from t(8;14) (q24;32)?
|
Burkitts Lymphoma
|
|

What does this picture represent?
|
Reciprical translocation... i.e. burkitts lymphoma
|
|
|
What are the two types of Burkitts lymphoma and how do u know physically and biologically?
|
1. Endemic- seen in africa enlarged mandible tumor- EBV strong association 10 million around 7 y/o
2. Sporadic- involves abdominal organs- around 11 y/o |
|
|
What are two advantages to using PCR?
|
1. Quick abundant substrate for mutation detection strategies.
2. Detecting changes in DNA length, such as small insertions or deletions. |
|
|
What do restriction enzymes do and how do you identify? What are some examples?
|
a. They cleave DNA at specific spots so when they are viewed you look for specific markers at certain spots...known as pallindromes ECO-R1
|
|
|
Where would the restriction enzyme cut?
|
If there is three codons and followed by its three that it would pair with cause A-T and G-C so GAATTC is like seeing pair inside out
|
|
|
What is the significance of Microarrays?
|
Shows in colors which genes are expressed in different people...
Allows to see if tumor expression is function of specific gene expression |
|
|
What is a SNP and significance to use in clinical medicine?
|
Single necleotide polymorphism- when a single nucleotide differs between members of species or individual paired chromosomes
Clinical- single differences in gene could make individuals more predisposed to disease or matches that resist disease. It is the study of SNPs that is synonomous with individualized medicine. |
|
|
What is cytochrome P450 used for?
|
Drug metabolizing enzymes that are used to make cholesterol steroids and other improtant lipids, contain a heme group
|
|
|
What is medical significance of AmpliChip CYP450?
What do labels P450, CYP2D6, and mean? |
It can find out which P450 genes you have functioning.
Cytochrome p450 is supergene family CYP= gene 2= Family number D= Subfamily 6= specific gene |
|
|
What are four stains used for visualization of chromosomes?
|
1. G-banding- stains AT rich
2. Q-banding- Stains AT rich with UV light 3. R-banding- Uses G but reverse image 4. Chromosome painting- labeling each individual pairs with colors |
|
|
Explain differences between genotype and phenotype...
|
Genotype- reflects genetic composition of a person at a specific place (locus, gene, allele)
Pheno- defined by genotype and environment- alleles expressed |
|
|
Define the parts of a chromosome and how would you explain label Chr 16p11.2?
|
P, Q are arms, regions is first number, bands are second number within region and sub-bands follow decimal
[Chromosome 16 1 region, 1 band sub band 2 arm p |
|
|
What is it called when there is a presence of an extra chromosome?
What is germline mosaicism? What is mosaicism? |
- Chromosomal mosaicism
- Mutation that occurs in developing cells that is not part of parental cells - Cells within an individual with different DNA complements, or more that one genotype |
|
|
How is the X chromosome inactivate?
|
-Lyon's Barr Body hypothesis
- X-chromosome inactivating center (XIC) and proximal end of (Xq) - There is XIST RNA that binds to X-chromosome to inactivate |
|
|
If one X is inactivated then why is it important?
|
Still used for 15-20% of total gene expression
|
|
|
What are someways changes in chromosome # can occur?
|
1. Non-disjunction in MI or MII
2. Fertilization mistakes a. Partial Mole- two sperm fertilize one egg to equal 69 XXY or XXX b. Complete Mole- two sperm fertilize an empty egg== 46 XX or XY |
|
|
What is the lab presentations of complete vs. partial mole?
|
a. complete- no maternal contribution, no fetal parts, hCG higher than partial,
b. partial- maternal and paternal parts- fetals parts present embryo is viable for weeks |
|
|
What shows vaginal bleeding, abdominal pain, excessive uterine englargment, fetus smaller than gestational age, and ovarian cysts?
|
Mole! or Ovarian teratoma
|
|
|
What is the difference between ovarian teratoma and mole?
|
Teratoma- due to problem caused by all mom's genes
Mole- caused by double copy of Dad's genes |
|
|
What are the types of trisomys on non-sex chromosomes?
|
a. 13
b. 18 c. 21 |
|
|
How would you write trisomy 21 or 18? (for male)
|
47, XY +21
47, XY + 18 |
|
|
Compared to 18 and 21 what distinguishes presentation of 13?
|
SEVERE! and nondisjunction 80% from maternal and MI
- cleft lip/palate -patau syndrome |
|
|
What distinguishes 18 from other trisomy's?
|
- clenched fist
-rocker bottom feet -edwards syndrom MII nondisjuction |
|
|
What distinguishes 21 from other trisomies?
|
a. Simian crease
b. brushfield spots c. |
|
|
What is the most common cause of spontaneous abortions?
What is a sign of posibility of having a translocation downs? |
trisomy 16
- many spontaneous abortions |
|
What does this pedigree show?
|
translocation downs on 14
|
|
|
What are clinical signs of Klinefelter's syndrome?
|
a. elevated gonadotropic levels
b. infertility c. small testes d. gynecomastia- dude to High E:T level e. XXY |
|
|
A woman comes in with hanging arm (cubitus valgus) and a shielded chest and non development of secondary sexual characteristics.... she is?
|
45 X_
turners |
|
|
When a cystic hygroma develops in utero and the women born had short stature and micrognathia with no ovary development? whats ur diagnosis?
|
Turners
X_ |
|
|
You suspect patient to have turners and do a karyotype and find some Y chromosome... what cancer does she have a larger risk for?
|
gonadoblastoma
|
|
|
If non-disjunction occurs and mom gives u two chromosome and body tries to get rid of trisomy, but it gets rid of chromosome from Dad what is process called and disorder? What is process of trying to kill extra chromosome called?
|
a. uniparental disomy (two chromosomes but both from one parent)
b. chromosome rescue |
|
|
In uniparental Disomy whats the difference between disomy and isosomy?
|
Disomy- 2 chromosomes from same parent
Isosomy- 2 identical from same parent (non-disjunction in MII) |
|
|
What is Prader Wili Syndrom and Angelman Syndrom? How do you know which one it is?
|
microdeletion syndroms (uniparental disomy) both on 15q11-15 deletion
- Identifying on genes depends if child has disomy from mother (prader willi) and father (Angelman Syndrome) |
|
|
If you compared a prader willi subject to a Angelman syndrom person... what differences would you look for?
|
PW- short, fat, feeding problems who don't have vomiting reflex, hypogonadic, very awkward
AS- puppet like qualities very happy (angel like) |

