![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
49 Cards in this Set
- Front
- Back
|
visual agnosia
What is it? |
Inability to link visual perceptual input to known concepts for identification (inability to identify objects using vision)
|
|
|
Which region is affected in visual agnosia?
|
Caused by damage to the occipto-temporal region (approximately)
Described as a disconnection syndrome -> visual info areas and knowledge areas cannot communicate |
|
|
Associative agnosia
|
Can perceive objects OK
Cannot link percept to meaning Can see and describe the objects but can not identify them using vision (can identify them using other senses – ex. Sound, touch) |
|
|
Apperceptive agnosia
|
Can perceive basic sensory features
Cannot form a proper visual percept Cannot link impoverished percept to meaning Cannot describe any details about the object, cannot copy objects properly |
|
|
Prosopagnosia
What is Developmental prosopagnosia? |
* Cannot distinguish between faces but can identify people based on other basic visual features (or other senses)
Ex. Clothes, cologne, voice * Visual agnosia that is specific to faces * Understand that they are looking at a face, but cannot identify whose face it is (cannot recognize even own face in the mirror) |
|
|
Which side of the brain is affected in prosopagnosia?
How does it happen? |
* Affects right side of the brain specifically
* Developmental prosopagnosia: born with this condition (very rare) * Most commonly occurs with stroke * This region can also be used to acquire expertise in areas that are not face based |
|
|
Optic ataxia
|
* Difficulty using vision to guide action
* Can identify object but cannot interact with it (cannot grab the object), does not know exactly where the object is (precision is compromised) * Can still identify the object, can still move limbs (no fundamental visual problems) |
|
|
simultagnosia
|
can only see/process one object at a time
|
|
|
Where is the damage in optic ataxia?
How can it be simulated? |
* damage to dorsal stream
* Can simulate optic ataxia using transcranial magnetic stimulation (TMS) in neurologically healthy adults |
|
|
Which side of brain controls conscious spatial attention?
|
The control of conscious spatial attention is an essential cognitive function.
It is thought that this ability is preferentially controlled by the right hemisphere -> Damage to this network may result in subtle or profound impairments of attention |
|
|
Visuospatial neglect
( hemispatial neglect, neglect syndrome or even neglect ) |
Attention and awareness of the left side of space (and even the body) is absent
After stroke on right side, person may have the inability to pay attention to the left side of space |
|
|
Tests for visuospatial neglect (4)
|
line bisection task (identify middle of line says middle is more to the right)
Line cancellation test: cross out lines on the right side, neglect lines on the left Drawing: asked to label a clock, leaves left side blank but fills out all numbers Faces may be drawn fully because face area is fine, half of body is still missing Writing: only write on right half of the page |
|
|
Which hemisphere pays attention to which side of space?
|
* Left hemisphere pays attention to right side of space
* Right hemisphere pays attention to BOTH sides of space => Damaging right hemisphere… Only left with the left hem which only pays attention to right side of space |
|
|
Balint’s syndrome –
|
* double neglect (severe attention impairment)
* Complete obliteration of attention * Argued to being equally impairing as being completely blind * Low likelihood of recovery and dramatic impairment of function |
|
|
Which part of the brain is damaged in balint's syndrome?
|
Caused by bilateral parietal damage, may die (trauma, strokes)
|
|
|
Balint's syndrome symptoms (3)
|
3 symptoms
* Optic ataxia: difficulty using vision to guide action * Simultagnosia: can only see/process one object at a time * Sticky fixation: extreme difficulty moving gaze and changing direction of eyes * Also affects sound, touch, every other sense (ex. Can only process one sound at a time) Ex. If you have a pair of glasses and break them in half they will only see one half of the glasses because it is now 2 objects. Attention can constrain very quickly |
|
|
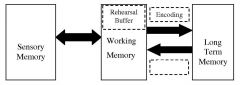
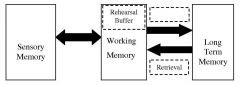
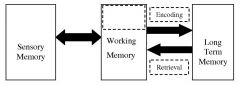
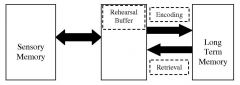
sensory memory
|
|
|
long term memory
* ‘Permanent’ store of knowledge that can be accessed at will When you learn something well enough to enter long term memory there is a permanent representation in your brain Capacity: impossible to test, arguably limitless Duration: limitless Longer you live, the more that is in your memory -> w/ age can be more difficult to access memories |
|
|
retrieval
Activation of LTMs, placed into WM for conscious consideration Retrieval failure? -> unable to access memories, brain gets stuck on the wrong answer and as you continue thinking about it you gets more stuck (brain continues to work on problems, so skipping the question will help) * Tip of the tongue phenomenon: retrieval failure * Stress, lack of sleep makes retrieval more difficult |
|
|
encoding
|
|
|
rehearsal buffer
|
|
|
working memory
|
|

|
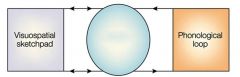
Visuospatial sketchpad
visual imagery |
|
|
Central executive
determines what to pay attention to (what is important) -> allocates resources to process either to loop or sketchpad |
|

|
Phonological loop (internal dialogue)
|
|
|
Which part of the brain supports working memory?
|
Prefrontal cortex (PFC) supports WM
Front 1/3 of the brain -> For working memory |
|
|
Evidence of WM being in prefrontal cortex: (3)
|
Work with non-human primates :
* Delayed match-to-sample task: Cue-> delay -> response. Before the response period of choosing where the item is, delay you keep the location of the item in the working memory. Delay period has the most prefrontal activity -> neurons hold info in mind (working memory) * Effects of cooling PFC: slows neural activity in the frontal lobes, therefore the monkey can’t hold on to memories (working memory suffers) -> impairs performance * Effects of dopamine infusions: working memory improves with dopamine agonist in the frontal lobe -> improves performance |
|
|
ADD
|
associated with frontal lobe dysfunction (not necessarily damage) -> more distractible
|
|
|
According to modal model of memory, why do we forget?
|
Can occur for many reasons :
* encoding fails (don’t spend enough time encoding, you will forget ex. Important to self test when studying for exam) * retrieval fails (info is in LTM but cannot access it) * attention (not paying proper attention to something) * Long term memory (destroyed by dementia, can be compromised by damage or disease) |
|
|
Declarative/explicit memory
|
memories you can talk about
* semantic * episodic |
|
|
Episodic memory:
|
memories of episodes of life, what happened and when it happened (context)
Flashbulb memories: memories that are incredibly emotional (often negative content), remember them even better ex. Vividly remembering where you were when the attacks of 9/11 occurred |
|
|
Semantic memory:
|
* For most info the context fades away and goes from episodic memory to semantic memory (natural process, lose resolution over time)
* only remembering what happened (not when you learned it) -> context fades, info that you know, not linked with when you learned it Ex. President of the United States (don’t know exactly when you learned it), knowing the colors (don’t know when you learned them) |
|
|
Non-declarative/implicit memory:
|
memories that are difficult or impossible to talk about
* procedural memory * priming * conditioning |
|
|
Procedural memory
|
outside of conscious awareness, do not need to focus on the specifics of the task, resistance to loss of these memories (will always remember how to ride a bike), knowledge about how to do something (can execute without conscious awareness)
ex. Driving, learning to ride a bike |
|
|
priming memory
|
brain activates concepts, which makes it easier to process them, processing related words faster
Ex. Briefly reviewing notes before going into the exam Conditioning (associative learning) |
|
|
Conditioning
|
(associative learning)
|
|
|
Gnostic hypothesis:
|
1 cell corresponds with 1 concept/piece of knowledge
“Grandmother cells” one cell to represent your grandma (corresponds to different pieces of knowledge you have) Very specific loss of knowledge w/ brain injury may be fine except for complete loss of knowledge of fruit (for example) |
|
|
Ensemble coding hypothesis
|
have cells that correspond to facial shape, hair, glasses, wrinkles, clothing, etc, activate lots of cells that make up Grandma
Representation of a concept by a set of neurons that code various features |
|
|
Retrograde amnesia (“soap opera”):
|
loss of memory from the past, tend to lose knowledge from more recently first (as severity increases, lose memories from farther back in time)
Temporally-graded |
|
|
Anterograde amnesia
|
inability to create new memories
|
|
|
Patient H.M. (1926 - 2008)
Which part was removed? |
Removal of his medial temporal lobes (MTL) bilaterally (Dr. Scoville)
|
|
|
What kind of memory in Patient H.M. was working? Which kind was impaired?
|
New memories in HM?
He can learn some things: Mirror tracing tasks: asked to trace shapes, and w/ experience he improves (less errors, faster), but doesn’t recognize he has done this task before evidence of learning but can’t remember that he learned Sequence learning: matching color sequences to numbers, improves w/ time + experience but again doesn’t remember learning it learning procedurally but is unable to remember learning b/c declarative memory is impaired |
|
|
What kind of amnesia did Patient H.M. develop?
|
* After-effects of the surgery -> profound anterograde amnesia (no new memories), partial retrograde amnesia (memory of his past was not jeopardized), short term memory and intelligence intact
|
|
|
The case of Clive Wearing:
What virus caused the damage? What kind of amnesia did he develop? |
Arguably the most severe memory patient in recorded history
Damage caused by Herpes Simplex Encephalitis (virus) -> sits on trigeminal nerve and ravaged his brain Anterograde and retrograde amnesia Cannot remember anything in his life except his wife Could only remember his wife -> each time he sees her it is as if it’s the first time he sees her (over and over and over again) |
|
|
Wernicke’s encephalopathy
|
Problems with eye and body movement, impaired
memory and confusion |
|
|
Cause of wernicke's encephalopathy?
|
Most commonly occurs in alcoholics, also occurs in anorexic and bulimic people
Chronic thiamine deficiency (vitamin B) |
|
|
Location of brain injury in Wernicke's encephalopathy?
|
Widespread but particularly affects the
mammillary bodies and part of the thalamus |
|
|
Korsakoff’s syndrome
|
When neurons in mammillary bodies and thalamus die completely
|
|
|
Korsakoff's syndrome symptoms (3)
Is recovery possible? |
Symptoms that persist after WE (permanent and irreversible)
* Severe anterograde amnesia * Retrograde amnesia * Confabulation: forget why they were going to do things, start to generate believable but nonsensible reasons for doing what they’re doing Ex. Grabbing winter coat in summer to put it away -> forget why they’re grabbing it -> say that it is freezing outside and that’s why they are grabbing their winter jacket Recovery is not possible |

