![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
61 Cards in this Set
- Front
- Back
|
What are the two somatic symptoms and related disorders? |
Illness Anxiety Disorder and Conversion Disorder |
|
|
What are the factors that contribute to somatic symptoms and related disorders? |
- Genetic and biological vulnerability - Early traumatic experiences - Learning (e.g. attention obtained from illness, lack of reinforcement of non-somatic expressions of distress) - Cultural and social norms (that devalue and stigmatise psychological suffering as compared with physical suffering |
|
|
What is conversion disorder? |
A) one or more symptoms of altered voluntary motor or sensory function B) clinical findings provide evidence of incompatibility between the symptom and recognised neurological or medical conditions C) the symptom or deficit is not better explained by another medical or mental disorder D) the symptom or deficit causes clinically significant distress or impairment in social, occupational, or other important areas of functioning or warrants medical evaluation |
|
|
What is illness anxiety disorder? |
- Preoccupation with having or acquiring a series illness - Somatic symptoms are not present, or if present, are only mild in intensity - There is a high level of anxiety about health, and the individual is easily alarmed about personal health status - The individual performs excessive health-related behaviours (e.g. checking body for signs of illness) or exhibits maladaptive avoidance (e.g. avoids appointments with doctor) |
|
|
What are dissociative disorders? |
- Characterise by a disruption of and/or discontinuity in the normal integration of consciousness, memory, identity, emotion, perception, body representation, motor control, and behaviour - Dissociative symptoms can potentially disrupt every area of psychological functioning |
|
|
How are dissociative symptoms experienced? |
- Unbidden intrusions into awareness and behaviour - Inability to access information or to control mental functions that normally are readily amenable to access or control (e.g. amnesia) |
|
|
What is dissociative amnesia? |
- Inability to recall important personal information, usually of a traumatic or stressful nature, that is inconsistent with ordinary forgetting - The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning - Can be distinguished from brain disorders and substance abuse |
|
|
What percentage of the population has dissociative amnesia? |
1-2% |
|
|
What is dissociative identity disorder? |
Two or more distinct personalities appear to exist in one person and appear to control behaviour. Each personality has a unique identity, name, and behaviour patterns |
|
|
Why is dissociative identity disorder considered a survival technique? |
98% of all diagnosed with DID have a history of abuse. |
|
|
What is the prevalence rate of anorexia nervosa? |
0.4% of young girls |
|
|
What psychological effects does starvation have as found by Keys et al. ? |
Psychological effects – severe depression, mood swings, irritability, anger outbursts, compulsive behaviours, self-harming, obsessional thoughts of food and eating, hoarding of food, changes in eating habits (more salt, spices), binge eating that persisted for months after refeeding, became isolated and withdrawn due to focus on food. |
|
|
What is the prevalence rate of bulimia nervosa? |
1-5% |
|
|
What are the problems associated with bulimia nervosa? |
- Purging related depletion in the electrolytes of potassium, chloride, and sodium, electrolyte disturbance found in 50% of people with BN results in weakness, tiredness, depression, irregular heartbeats, sudden death - Ulceration of mouth and throat and dental deterioration from exposure to gastric acid from vomiting - Abdominal pain from binge eating - Amenorrhea and menstrual irregularities |
|
|
Who are the primary at risk group? |
Women in high school and tertiary education have higher prevalence of eating disorders than non-students |
|
|
What are the risk factors for an eating disorder? |
- Genetic influence - Psychological factors: low self-esteem, negative affect (anxiety), perfectionism - Cultural influences: expectations for ideal weight from society and media, e.g., women’s magazines have more emphasis on weight loss than men’s magazines |
|
|
What are the treatments of anorexia nervosa? |
- No consensus over the most effective psychological treatment
- Few controlled studies evaluation treatment effectiveness due to low prevalence and long-term nature of most treatments - High drop-out rates - Research suggests promising therapy approaches- motivational enhancement therapy, cognitive behaviour therapy, family therapy |
|
|
What are the treatments of bulimia nervosa? |
- More research of treatment effectiveness than AN - CBT is treatment of choice BUT many do not respond to treatment suggesting need to improve treatment approaches - Interpersonal psychotherapy also demonstrates effectiveness - Primary focus of IPT is to help identify and change current interpersonal problems (e.g. conflict) that are assumed to be maintaining the eating disorder (via poor self-esteem, negative affect |
|
|
What are the 10 classifications of drugs? |
Alcohol; cannabis; hallucinogens (two categories); inhalants opioids; sedatives, hypnotics, and anxiolytics; stimulants (amphetamine-type substances, cocaine, etc.); tobacco; other (unknown) |
|
|
Which drugs are stimulants? |
Amphetamines, ecstasy, tobacco, cocaine |
|
|
Which drugs are depressants? |
Alcohol, heroin, benzodiazepines, cannabis |
|
|
Which drugs are hallucinogens? |
PCP (angel dust), LSD, mushrooms, ecstasy |
|
|
What are the similarities between the three categories of drugs? |
If taken in excess directly activate the brain reward system |
|
|
What are the short term effects of methamphetamines? |
Euphoria, increased wellbeing, confidence, physical activity, improved cognitive and physical performance, suppression of appetite, reduced need for sleep |
|
|
What are the long term physical effects of meth? |
- Weight loss, malnutrition, lowered immune functioning - Impaired neuropsychological functioning - Vascular and organ damage |
|
|
What are the long term psychological effects of meth? |
Psychosis, delirium, paranoia, bizarre behaviour, sexual dysfunction, tactile hallucinations
|
|
|
What are substance-use disorders? |
Cognitive, behavioural, and physiological symptoms indicating that the individual continues to use the substance despite significant substance related problems |
|
|
What is Alcohol Use Disorder? |
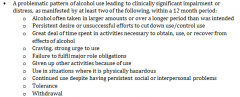
|
|
|
What are the biological factors that may cause alcohol use disorder? |
- Genetics – strong evidence that genetics predispose individuals to substance use disorders: e.g. significantly higher rate of alcohol use disorders in identical twins versus fraternal twins - Dopaminergic Reward System - Endogenous Opioid System |
|
|
What are the behavioural psychological factors that may cause alcohol use disorder? |
- Operant conditioning Positive reinforcement: the sense of pleasure or ‘high’ is the positive reinforcer Negative reinforcement: the alleviation of an unpleasant state (distressing mood, withdrawal or craving) - Classical conditioning Unrelated stimuli (e.g. syringe) becomes associated with drug use, and elicits compensatory response Partially explains tolerance and craving – physiological component and psychological component |
|
|
What are the cognitive psychological factors that may cause alcohol use disorder? |
- Outcome expectancy theory – positive expectations of substance abuse increase the likelihood of using the substance - Cognitive theory - those who are dependent have ‘dysfunctional beliefs’ E.g. “I am no good at socialising, alcohol makes me more confident” - Relapse prevention theory – people in high risk situations will use if they Do not have adequate coping strategies or self-efficacy Have positive expectations of drug use |
|
|
How common is comorbidity with substance use? |
Approximately 25% of those with a substance use disorder has another mental health disorder |
|
|
Why is comorbidity so common for substance use? |
- Mental health problems leading to substance use * Self-medication * Social vulnerability - Substance use leading to mental health problems * E.g. alcohol abuse – job loss – depression * Direct effects of substance use – cannabis and amphetamine use can both trigger psychotic episodes and once triggered there is a greater chance of continued psychotic illness |
|
|
What are the treatments of substance use disorders? |
- Detoxification - Appropriate goals – i.e. abstinence vs. moderation - Motivational Interviewing * Using Prochaska and DiClemete’s (1986) Stages of Change Model - Pre-contemplation – contemplation – preparation – action – maintenance - CBT/skills training interventions - Pharmacological interventions * Naltrexone, nicotine replacement, methadone - Relapse prevention |
|
|
What is the definition of gambling? |
Gambling “involves risking something of value in the hopes of obtaining something of greater value”
|
|
|
What are the different types of gambling? |
- Gaming: casino table games, electronic gaming machines (including online)
- Wagering: horse racing, betting on selected events - Lotteries: Lotto, Powerball, scratchies |
|
|
What are the similarities between gambling disorder and substance use disorder? |
- Gaming: casino table games, electronic gaming machines (including online) - Wagering: horse racing, betting on selected events - Lotteries: Lotto, Powerball, scratchies |
|
|
What is the Addiction Model of Gambling |
Individuals repeatedly engage in behaviours to achieve a euphoric state of arousal or to escape negative mood states |
|
|
What is the Gambling Disorder criteria? |
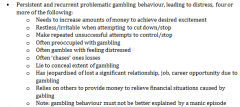
|
|
|
What are the biological factors that may cause gambling disorders? |
- Genetic and neurobiology * Disturbances in serotonin, dopamine, and norepinephrine neurotransmitter systems * Decreased serotonin associated with * Poor impulse control (e.g. suicide, violence) * Personality traits of impulsivity and sensation seeking * SSRI medication associated with some positive outcomes for gamblers |
|
|
What are the behavioural psychological factors that may cause gambling disorders? |
- Operant conditioning * Positive and negative reinforcement * Intermittent and variable schedules of reinforcement - Classical conditioning * Environmental cues (e.g. sights and sounds) trigger a state of arousal/excitement or craving |
|
|
What are the cognitive errors associated with gambling disorders? |
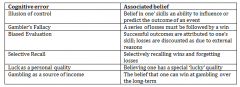
|
|
|
What are the treatments of gambling disorders? |
- Earliest – psychodynamic - Gamblers anonymous - Exposure therapy - Cognitive therapy - CBT – combination of exposure to gambling cues and use of cognitive challenging of common cognitive errors * Approximately 70% success rate - Pharmacology * Best evidence in treatment of comorbid gambling but some mixed evidence for SSRIs and mood stabilisers - Public health model |
|
|
What services do the National Standards apply to? |
The standards have been developed to be applied across the broad range of mental health services. This includes: - Bed based (hospitals) - Community mental health services - Non-government sectors - Private sector - Primary care and general practice |
|
|
What is the Standard 1. Rights and responsibility |
The rights and responsibilities of people affected by mental health problems and/or mental illness are upheld by the mental health service (MHS) and are documented, prominently displayed, applied and promoted throughout all phases of care |
|
|
What is the Standard 2. Safety? |
The activities and environment of the MHS are safe for consumers, carers, families, visitors, staff and its community |
|
|
What is the Standard 3. Customer and carer participation? |
Consumers and carers are actively involved in the development, planning, delivery and evaluation of services |
|
|
What is the Standard 4. Diversity responsiveness |
The MHS delivers services that take into account the cultural and social diversity of its consumers and meets their needs and those of their carers and community throughout all phases of care |
|
|
What is the Standard 5. Promotion and prevention? |
The MHS works in partnership with its community to promote mental health and address prevention of mental health problems and/or mental illness |
|
|
What is the Standard 6. Consumers? |
Consumers have the right to comprehensive and integrated mental health care that meets their individual needs and achieves the best possible outcome in terms of that recovery |
|
|
What is the Standard 7. Carers? |
The MHS recognises, respects, values and supports the importance of carers to the wellbeing, treatment, and recovery of people with a mental illness |
|
|
What is the Standard 8. Governance, leadership, and management? |
The MHS is governed, led and managed effectively and efficiently to facilitate the delivery of quality and coordinated services |
|
|
What is the Standard 9. Integration? |
The MHS collaborates with and develops partnerships within its own organisation and externally with other service providers to facilitate coordinated and integrated services for consumers and carers |
|
|
What is Standard 10.1 Supporting recovery? |
The MHS incorporates recovery principles into service delivery, culture and practice providing consumers with access and referral to a range of program that will support sustainable recovery |
|
|
What is Standard 10.2 Access? |
The MHS is accessible to the individual and meets the needs of its community in a timely manner |
|
|
What is Standard 10.3 Entry? |
The entry process to the MHS meets the needs of its community and facilitates timeliness of entry and ongoing assessment |
|
|
What is the Standard 10.4 Assessment and review? |
Consumers receive a comprehensive, timely and accurate assessment and a regular review of progress is provided to the consumer and their carer(s) |
|
|
What is the Standard 10.5 Treatment and support? |
The MHS provides access to a range of evidence based treatments and facilitates access to rehabilitation and support programs which address the specific needs of consumers and promotes their recovery |
|
|
What is Standard 10.6 Exit and re-entry? |
The MHS assists consumers to exit the service and ensures re-entry according to the consumer’s needs |
|
|
What are evidence based treatments? |
“Evidence-based treatment (EBT) refers to the interventions or techniques (e.g. cognitive therapy for depression, exposure therapy for anxiety) that have produced therapeutic change in controlled trails.” |
|
|
How is social and emotional wellbeing measured? |
- Psychological distress - The impact of psychological distress - Positive wellbeing - Anger - Life stressors - Discrimination - Cultural identification - Removal form natural family |

