![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
85 Cards in this Set
- Front
- Back
|
Which substance has net secretion in the proximal tubule?
|
PAH
|
|
|
Which substance has net reabsorption in the proximal tubule?
|
- Urea
- Na+, K+, Cl- - Pi - HCO3- - Glucose and amino acids |
|
|
Which substance has no net secretion or reabsorption in the proximal tubule?
|
Creatinine and Inulin
|
|
|
How does the reabsorption of Cl- compare to Na+ in the proximal tubule?
|
Cl- reabsorption occurs at a slower rate than Na+ in early proximal tubule and then matches the rate of Na+ reabsorption more distally; thus, its relative concentration increases before it plateaus
|
|
|
What is the action of Renin? Source?
|
Stimulates conversion of Angiotensinogen (from liver) to Angiotensin I
- Renin is from the kidney |
|
|
What is the source of Renin? What stimulates it?
|
Renin is from the kidney, release stimulated by:
- ↓ BP (Juxtaglomerular cells) - ↓ Na+ delivery to macula densa cells - ↑ Sympathetic tone (β1-receptors) |
|
|
What is the action of ACE? Source?
|
- ACE converts Ang I to Ang II
- ACE also stimulates Bradykinin breakdown - ACE is from the lungs and the kidneys |
|
|
What is the action of Angiotensin II?
|
- Vasoconstriction (via AT I receptors) → ↑ BP
- Constricts efferent arteriole of glomerulus → ↑ FF to preserve renal function (GFR) in low-volume states (when ↓ RBF) - Stimulates Aldosterone (adrenal gland) - Stimulates ADH (posterior pituitary) - ↑ Proximal tubule Na+/H+ activity → ↑ Na+, HCO3-, and H2O reabsorption (can permit contraction alkalosis) - Stimulates hypothalamus → thirst |
|
|
How does AngII increase the BP?
|
Acts at AT I receptors on vascular smooth muscle → Vasoconstriction → ↑ BP
|
|
|
How does AngII affect the filtration fraction (FF)?
|
Constricts efferent arteriole of glomerulus → ↑ FF to preserve renal function (GFR) in low-volume states (ie, when RBF ↓)
|
|
|
What is the effect of Aldosterone release? Source?
|
- ↑ Na+ channel and Na+/K+ pump insertion in principal cells
- Enhances K+ and H+ excretion (upregulates principal cell K+ channels and intercalated cell H+ ATPases) - Creates unfavorable Na+ gradient for Na+ and H2O reabsorption - From adrenal gland |
|
|
What is the effect of ADH release? Source?
|
- ↑ H2O channel insertion in principal cells, leading to H2O reabsorption
- From posterior pituitary |
|
|
What is the effect of Angiotensin II on the proximal tubule?
|
- ↑ Proximal tubule Na+/H+ activity
- Leads to Na+, HCO3-, and H2O reabsorption (can permit contraction alkalosis) |
|
|
Which hormone affects baroreceptor function, limiting the reflex bradycardia, which would normally accompany its pressor effects?
|
Angiotensin II
|
|
|
Which hormone is released from atria in response to increased volume, may act as a check on renin-angiotensin-aldosterone system, relaxing vascular smooth muscle via cGMP, causing ↑ GFR and ↓ renin?
|
ANP (Atrial Natriuretic Protein)
|
|
|
Which hormone is primarily responsible for regulating osmolarity and responds to low blood volume states?
|
ADH
|
|
|
Which hormone primarily regulates ECF Na+ content and volume, by responding to low blood volume states?
|
Aldosterone
|
|
|
What are the components of the juxtaglomerular apparatus?
|
- JG cells (modified smooth muscle of afferent arteriole)
- Macula Densa (NaCl sensor, part of the distal convoluted tubule) |
|
|
What is the function of the Juxtaglomerular cells?
|
Secrete renin in response to:
- ↓ Renal blood pressure - ↓ NaCl delivery to distal tubule - ↑ Sympathetic tone (β1) |
|
|
Which drugs can influence the juxtaglomerular apparatus?
|
β-blockers (specifically β1) can decrease BP by inhibiting β1 receptors of JGA, causing ↓ renin release
|
|
|
Which hormones are secreted by the kidney?
|
- Erythropoietin
- 1,25-(OH)2 Vitamin D - Renin - Prostaglandins |
|
|
What is the source and function of Erythropoietin?
|
Released by interstitial cells in the peritubular capillary bed in response to hypoxia
|
|
|
What is the source and function of 1,25-(OH)2 Vitamin D?
|
- Proximal tubule cells convert 25-OH vitamin D to 1,25-(OH)2 Vitamin D (Active form)
- Enzyme: 1α-Hydroxylase (stimulated by PTH) |
|
|
What is the source and function of Renin?
|
Secreted by JG cells in response to ↓ renal arterial pressure and ↑ renal sympathetic discharge (β1 effect)
|
|
|
What is the source and function of prostaglandins?
|
- Paracrine secretion vasodilates the afferent arterioles to ↑ RBF
- From kidney |
|
|
What is the effect of NSAIDs on the kidney?
|
- NSAIDs block renal-protective prostaglandin synthesis → constriction of the afferent arteriole and ↓ GFR
- This may result in acute renal failure |
|
|
Which hormones act on the kidney?
|
- Angiotensin II (ATII)
- Atrial Natriuretic Peptide (ANP) - Parathyroid Hormone (PTH) - Aldosterone - ADH (Vasopressin) |
|
|
What causes Angiotensin II (AT II) to be released and act on kidney? Function?
|
- Synthesized in response to ↓ BP
- Causes efferent arteriole constriction → ↑ GFR and ↑ FF - Compensatory Na+ reabsorption in proximal and distal nephron - Net effect: preservation of renal function in low-volume state (↑FF) with simultaneous Na+ reabsorption to maintain circulating volume |
|
|
What causes Parathyroid Hormone (PTH) to be released and act on kidney? Function?
|
- Secreted in response to ↓ plasma [Ca2+], ↑ plasma [PO4(3-)], or ↓ plasma 1,25-(OH)2 vitamin D
- Causes ↑ [Ca2+] reabsorption from DCT, ↓ [PO4(3-)] reabsorption (PCT), and ↑ 1,25-(OH)2 vitamin D production - Increases Ca2+ and PO4(3-) absorption from gut via vitamin D |
|
|
Where are Ca2+ and PO4(3-) reabsorbed in nephron in response to PTH?
|
- Ca2+ reabsorbed in DCT
- PO4(3-) reabsorbed in PCT |
|
|
What causes Atrial Natriuretic Peptide (ANP) to be released and act on kidney? Function?
|
- Secreted in response to ↑ atrial pressure
- Causes ↑ GFR and ↑ Na+ filtration with no compensatory Na+ reabsorption in distal nephron - Net effect: Na+ loss and volume loss |
|
|
What causes Aldosterone to be released and act on kidney? Function?
|
- Secreted in response to ↓ blood volume (via AT II) and ↑ plasma [K+]
- Causes ↑ Na+ reabsorption, ↑ K+ secretion, ↑ H+ secretion |
|
|
What causes ADH (Vasopressin) to be released and act on kidney? Function?
|
- Secreted in response to ↑ plasma osmolarity and ↓ blood volume
- Binds to receptors on principal cells, causing ↑ number of water channels and ↑ H2O reabsorption |
|
|
Which conditions/drugs cause K+ to shift out of cells (causing hyperkalemia)?
|
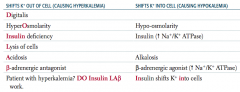
Patient with hyperkalemia? DO Insulin LAβ work
- Digitalis - HyperOsmolarity - INSULIN deficiency - Lysis of cells - Acidosis - β-adrenergic antagonist |
|
|
Which conditions/drugs cause K+ to shift into cells (causing hypokalemia)?
|
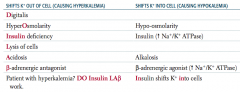
INsulin shifts K+ INto cells
- Hypoosmolarity - Insulin (↑ Na+ / K+ ATPase) - Alkalosis - β-adrenergic agonist (↑ Na+ / K+ ATPase) |
|
|
What electrolyte disturbance causes nausea, malaise, stupor, and coma?
|
Low serum Na+
|
|
|
What electrolyte disturbance causes irritability, stupor, or coma?
|
High serum Na+
|
|
|
What electrolyte disturbance causes U waves on ECG, flattened T waves, arrhythmias, and muscle weakness?
|
Low serum K+
|
|
|
What electrolyte disturbance causes wide QRS and peaked T waves on ECG, arrhythmias, and muscle weakness?
|
High serum K+
|
|
|
What electrolyte disturbance causes tetany, seizures, and QT prolongation?
|
Low serum Ca2+
|
|
|
What electrolyte disturbance causes stones (renal), bones (pain), groans (abdominal pain), psychiatric overtones (anxiety, altered mental status), but not necessarily calciuria?
|
High serum Ca2+
|
|
|
What electrolyte disturbance causes tetany and Torsades de Pointes?
|
Low serum Mg2+
|
|
|
What electrolyte disturbance causes ↓ DTRs, lethargy, bradycardia, hypotension, cardiac arrest, and hypocalcemia?
|
High serum Mg2+
|
|
|
What electrolyte disturbance causes bone loss and osteomalacia?
|
Low serum PO4(3-)
|
|
|
What electrolyte disturbance causes renal stones, metastatic calcifications, and hypocalcemia?
|
High serum PO4(3-)
|
|
|
What is the effect of low vs high serum concentration of Na+?
|
- Low: nausea, malaise, stupor, coma
- High: irritability, stupor, coma |
|
|
What is the effect of low vs high serum concentration of K+?
|
- Low: U waves on ECG, flattened T waves, arrhythmias, muscle weakness
- High: wide QRS and peaked T waves on ECG, arrhythmias, muscle weakness |
|
|
What is the effect of low vs high serum concentration of Ca2+?
|
- Low: tetany, seizures, QT prolongation
- High: stones (renal), bones (pain), groans (abdominal pain), psychiatric overtones (anxiety, altered mental status), but not necessarily calciuria |
|
|
What is the effect of low vs high serum concentration of Mg2+?
|
- Low: tetany and torsades de pointes
- High: ↓ DTRs (reflexes), lethargy, bradycardia, hypotension, cardiac arrest, hypocalcemia |
|
|
What is the effect of low vs high serum concentration of PO4(3-)?
|
- Low: bone loss, osteomalacia
- High: renal stones, metastatic calcifications, hypocalcemia |
|
|
What is the pH, PCO2, and [HCO3-] associated with metabolic acidosis? Compensatory response?
|
- ↓ pH
- ↓ PCO2 - ↓↓ [HCO3-] - Immediate hyperventilation ↓↓ = 1° distrubance ↓ = compensatory response |
|
|
What is the pH, PCO2, and [HCO3-] associated with metabolic alkalosis? Compensatory response?
|
- ↑ pH
- ↑ PCO2 - ↑↑ [HCO3-] - Immediate hypoventilation ↑↑ = 1° distrubance ↑ = compensatory response |
|
|
What is the pH, PCO2, and [HCO3-] associated with respiratory acidosis? Compensatory response?
|
- ↓ pH
- ↑↑ PCO2 - ↑ [HCO3-] - ↑ Renal [HCO3-] reabsorption (delayed) ↑↑ = 1° distrubance ↑ = compensatory response |
|
|
What is the pH, PCO2, and [HCO3-] associated with respiratory alkalosis? Compensatory response?
|
- ↑ pH
- ↓↓ PCO2 - ↓ [HCO3-] - ↓ Renal [HCO3-] reabsorption (delayed) ↓↓ = 1° distrubance ↓ = compensatory response |
|
|
What is the Henderson-Hasselbach equation in terms of [HCO3-] and PCO2?
|
pH = 6.1 + log [HCO3-] / 0.03 PCO2
|
|
|
How can you calculate the predicted respiratory compensation for a simple metabolic acidosis? What does it tell you?
|
Winters Formula
- If the measured PCO2 differs significantly from the predicted PCO2, then a mixed acid-base disorder is likely present PCO2 = 1.5 [HCO3-] + 8 +/- 2 |
|
|
If you suspect an acidosis or alkalosis, what do you check first?
|
Check arterial pH
- pH <7.4 = Acidemia - pH >7.4 = Alkalemia |
|
|
What do you test after you establish a patient has an acidemia (arterial pH <7.4)?
|
Check PCO2
- PCO2 >40 mmHg = Respiratory Acidosis - PCO2 <40 mmHg = Metabolic Acidosis with compensation (hyperventilation) |
|
|
What do you test after you establish a patient has an alkalemia (arterial pH >7.4)?
|
Check PCO2
- PCO2 <40 mmHg = Respiratory Alkalosis - PCO2 >40 mmHg = Metabolic Alkalosis with compensation (hypoventilation) |
|
|
What is the diagnosis if a patient has pH <7.4 and PCO2 >40mmHg? What causes this?
|
Respiratory Acidosis, caused by hypoventilation, such as:
- Airway obstruction - Acute lung disease - Chronic lung disease - Opioids, sedatives - Weakening of respiratory muscles |
|
|
What is the diagnosis if a patient has pH <7.4 and PCO2 <40mmHg? What should you check next?
|
Metabolic Acidosis with compensation (hyperventilation)
- Check for anion gap Anion Gap = Na+ - (Cl- + HCO3-) Normal: 8-12 mEq/L |
|
|
What is the diagnosis if a patient has pH <7.4 and PCO2 <40mmHg and an ↑ anion gap? What are the potential causes?
|
Metabolic Acidosis with compensation (hyperventilation)
MUDPILES: - Methanol (formic acid) - Uremia - Diabetic Ketoacidosis - Propylene glycol - Iron tablets or INH - Lactic acidosis - Ethylene glycol (oxalic acid) - Salicylates (late) |
|
|
What is the diagnosis if a patient has pH <7.4 and PCO2 <40mmHg and a normal anion gap (8-12 mEq/L)? What are the potential causes?
|
Metabolic Acidosis with compensation (hyperventilation) |
|
|
What is the diagnosis if a patient has pH >7.4 and PCO2 <40mmHg? What causes this?
|
Respiratory alkalosis, can be caused by: |
|
|
What is the diagnosis if a patient has pH >7.4 and PCO2 >40mmHg? What causes this?
|
Metabolic alkalosis with compensation (hypoventilation), caused by: |
|
|
What do these have in common? What would they cause?
- Airway obstruction - Acute lung disease - Chronic lung disease - Opioids, sedatives - Weakening of respiratory muscles |
Causes of hypoventilation → Respiratory Acidosis
|
|
|
What do these have in common? What would they cause?
- Methanol (formic acid) - Uremia - Diabetic Ketoacidosis - Propylene glycol - Iron tablets or INH - Lactic acidosis - Ethylene glycol (oxalic acid) - Salicylates (late) |
Metabolic Acidosis with compensation (hyperventilation) with ↑ Anion Gap |
|
|
What do these have in common? What would they cause?
- Hyperalimentation - Addison disease - Renal tubular acidosis - Diarrhea - Acetazolamide - Spironolactone - Saline infusion |
Metabolic Acidosis with compensation (hyperventilation) with normal Anion Gap (8-12 mEq/L)
|
|
|
What do these have in common? What would they cause?
- Hysteria - Hypoxemia (eg, high altitude) - Salicylates (early) - Tumor - Pulmonary embolism |
Causes of hyperventilation → Respiratory Alkalosis
|
|
|
What do these have in common? What would they cause?
- Loop diuretics - Vomiting - Antacid use - Hyperaldosteronism |
Metabolic Alkalosis with compensation (hypoventilation)
|
|
|
When should you calculate the anion gap? How? What is normal?
|
When you have a metabolic acidosis (pH < 7.4 and PCO2 < 40 mmHg)
Anion Gap = Na+ - (Cl- + HCO3-) Normal = 8-12 mEq/L |
|
|
What kind of disorder causes a non-anion gap hyperchloremic metabolic acidosis?
|
Renal Tubular Acidosis
|
|
|
What are the types of Renal Tubular Acidosis?
|
- Type 1: distal, pH >5.5
- Type 2: proximal, pH <5.5 - Type 4: hyperkalemic, pH <5.5 |
|
|
Which type of Renal Tubular Acidosis is caused by a defect in the ability of the α intercalated cells to secrete H+? Implications?
|
Type 1 (distal, pH >5.5)
- New HCO3- is not generated → metabolic acidosis - Associated with hypokalemia, ↑ risk for calcium phosphate kidney stones (d/t ↑ urine pH and ↑ bone turnover) |
|
|
What can cause Type 1 Renal Tubular Acidosis (distal, pH >5.5)?
|
Defects in ability of α intercalated cells to secrete H+
- Amphotericin B toxicity - Analgesic nephropathy - Congenital anomalies (obstruction) of urinary tract |
|
|
Which type of Renal Tubular Acidosis is caused by a defect in the proximal tubule HCO3- reabsorption? Implications?
|
Type 2 (proximal, pH < 5.5)
- Leads to ↑ excretion of HCO3- in urine and subsequent metabolic acidosis - Urine is acidified by α intercalated cells in collecting tubule - Associated with hypokalemia and ↑ risk for hypophosphatemic rickets |
|
|
What can cause Type 2 Renal Tubular Acidosis (proximal, pH <5.5)?
|
Defects in proximal tubule HCO3- reabsorption:
- Fanconi syndrome (eg, Wilson disease) - Chemicals toxic to proximal tubule (eg, lead, aminoglycosides) - Carbonic anhydrase inhibitors - Multiple myeloma (light chains) |
|
|
Which type of Renal Tubular Acidosis is caused by hypoaldosteronism, aldosterone resistance, or K+ sparing diuretics? Implications?
|
- Results in hyperkalemia
- Impairs ammoniagenesis in proximal tubule → ↓ buffering capacity and ↓ H+ excretion into urine |
|
|
What can cause Type 4 Renal Tubular Acidosis (hyperkalemic, pH <5.5)?
|
- Hypoaldosteronism
- Aldosterone resistance - K+ sparing diuretics |
|
|
What are the characteristics of Type 1 Renal Tubular Acidosis?
|
Distal, pH>5.5
- Defect in ability of α intercalated cells to secrete H+ - New HCO3- is not generated → metabolic acidosis - Associated with hypokalemia, ↑ risk for calcium phosphate kidney stones (d/t ↑ urine pH and ↑ bone turnover) Causes: - Amphotericin B toxicity - Analgesic nephropathy - Congenital anomalies (obstruction) of urinary tract |
|
|
What are the characteristics of Type 2 Renal Tubular Acidosis?
|
Proximal, pH<5.5
- Defect in proximal tubule HCO3- reabsorption - ↑ Excretion of HCO3- in urine and subsequent metabolic acidosis - Urine acidified in α intercalated cells in collecting tubule - Associated with hypokalemia and ↑ risk for hypophosphatemic rickets Causes: - Fanconi syndrome (eg, Wilson disease) - Chemicals toxic to proximal tubule (eg, lead, aminoglycosides) - Carbonic anhydrase inhibitors - Multiple myeloma (light chains) |
|
|
What are the characteristics of Type 4 Renal Tubular Acidosis?
|
Hyperkalemic, pH<5.5
- Results in hyperkalemia, which impairs ammoniagenesis in proximal tubule - ↓ Buffering capacity and ↓ H+ excretion into urine Causes: - Hypoaldosteronism - Aldosterone resistance - K+ sparing diuretics |
|
|
Which type of Renal Tubular Acidosis is associated with hypokalemia and and increased risk for calcium phosphate kidney stones?
|
Type 1 (distal, pH >5.5)
|
|
|
Which type of Renal Tubular Acidosis is associated with hypokalemia and increased risk for hypophosphatemic rickets?
|
Type 2 (proximal, pH <5.5)
|
|
|
Which type of Renal Tubular Acidosis is associated with hyperkalemia?
|
Type 4 (hyperkalemic, pH <5.5)
|

